Methotrexate-Associated Lymphoproliferative Disorder: A Rare Case of Large Liver Tumors
Abbreviations
-
- CD
-
- cluster of differentiation
-
- EBER
-
- Epstein-Barr virus–encoded small RNA
-
- LDH
-
- lactate dehydrogenase
-
- LPD
-
- lymphoproliferative disorder
-
- MTX
-
- methotrexate
-
- MTX-LPD
-
- MTX-associated LPD
-
- TACE
-
- transcatheter arterial chemoembolization
Methotrexate-associated lymphoproliferative disorder (MTX-LPD) develops during MTX usage and is classified as “other iatrogenic immunodeficiency-associated LPDs.” Approximately 60%-90% of MTX-LPD patients show spontaneous regression after MTX withdrawal. We report a case of large liver tumors due to MTX-LPD.
Case Presentation
A 76-year-old woman presented with fever and abdominal pain, which had lasted for a week. She had a history of rheumatoid arthritis and had been receiving MTX for 5 years. Laboratory tests showed a lactate dehydrogenase (LDH) level of 761 IU/L. Physical examinations showed no remarkable findings. Although abdominal ultrasound 1 year before had shown no tumors, contrast-enhanced computed tomography revealed two tumors: one in the anterior segment (10 cm in diameter) (Fig. 1A) and another in the posterior segment (7 cm in diameter) (Fig. 1B). The tumors were slightly enhanced and showed a duct-penetrating sign (Fig. 1A, white arrow). A tumor in the right kidney (Fig. 1C) and a lymphadenopathy in the mediastinum (Fig. 1D) were also detected. We speculated that the presence of huge liver tumors extending to the liver surface with abdominal pain implied impending rupture of these liver tumors. Therefore, transcatheter arterial chemoembolization (TACE) was urgently performed to prevent rupture. Superior mesenteric arteriography showed a tumor stain both in the anterior and the posterior segments (Fig. 1E). Epirubicin plus lipiodol emulsion with gelatin sponge particles were administered from the anterior and posterior segmental branches of the right hepatic artery.
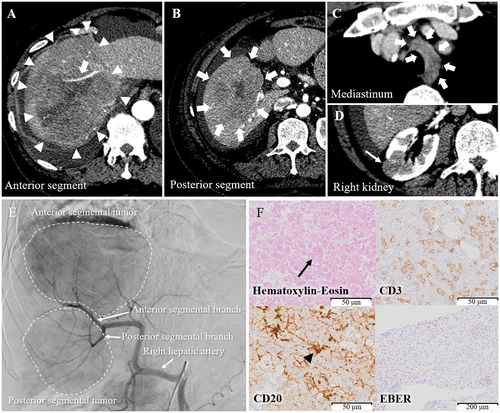
Computed tomography performed 17 days after TACE showed remarkable reduction in the size of the liver tumors; the extrahepatic tumors had also shrunk remarkably. Laboratory tests showed a normalized level of LDH. Furthermore, it was noted that the patient had discontinued MTX 11 days before undergoing TACE. Altogether, liver tumors due to MTX-LPD were suspected. For definitive diagnosis, echo-guided biopsy of the liver tumors was performed. Although necrotic tissues were predominantly present in the specimens, we observed atypical large lymphocytes (Fig. 1F, black arrow) that were positive for cluster of differentiation 20 (CD20; Fig. 1F, black arrowhead) and negative for CD3 and Epstein-Barr virus (EBV)–encoded small RNA (EBER) on immunohistochemistry, implying that the liver tumors were of B-cell origin. She was ultimately diagnosed with MTX-LPD. Subsequently, further spontaneous reduction of the liver tumors was observed (Fig. 2A,B). The extrahepatic tumors completely disappeared 129 days after TACE (Fig. 2C,D).

Discussion
MTX-LPD is an LPD that develops during MTX usage and is classified as “other iatrogenic immunodeficiency-associated LPDs.”1 Most MTX-LPDs are of B-cell origin, and their pathogenesis is associated with EBV infection. An increased level of LDH is associated with MTX-LPD.2, 3 The histopathological features of MTX-LPD are diverse, varying from polyclonal to monoclonal lymphocytosis.4 The frequency of extranodal involvement, including that of the lung, head, and neck, is relatively high; but hepatic involvement is extremely rare.5
Although there is no standard treatment for MTX-LPD, approximately 60%-90% of MTX-LPD patients show spontaneous regression following MTX withdrawal, which is seen more frequently in cases positive for EBER on immunohistochemistry.3-5 Therefore, a watch-and-wait strategy may be the first choice for MTX-LPD management, especially in EBER-positive cases. If spontaneous regression is not observed, aggressive chemotherapy is needed.2 Here, TACE, which is not a standard lymphoma treatment, was unintentionally performed. It might have influenced liver tumor shrinkage as the liver tumors showed striking regression.
In conclusion, the possibility of MTX-LPD should be considered in cases where tumors are noted in patients using MTX.




