Hepatic infiltration by silicone in a patient With ASIA syndrome
Potential conflict of interest: none.
Abbreviation
-
- ASIA
-
- autoimmune/inflammatory syndrome induced by adjuvants
Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) is frequently characterized by myalgias, myositis, arthralgia, neurological manifestations, fever, dry mouth, and cognitive alterations.1 In the range of clinical conditions related to ASIA syndrome, siliconosis after breast implants has been reported.1 Here, we report a case of hepatic infiltration by silicone in a patient with ASIA syndrome.
Case Report
A 55-year-old woman with a 10-year-old mammary prosthesis developed Sjögren's syndrome (sicca syndrome, anti-Ro, and salivary gland biopsy positivity) for 4 years and rupture of one side of the prosthesis for 1 year. After 3 months of moderate abdominal pain in the right hypochondrium, hyperthermia, pruritus, chronic fatigue, and myalgia, she was admitted to the emergency department. Physical examination showed pain on palpation of the right hypochondrium. Regarding laboratory findings, hepatic enzymes were elevated (alanine aminotransferase, 68 UI/L [reference value, 0-31 UI/L]; aspartate aminotransferase, 50.6 UI/L [reference value, 0-32 UI/L]) and anti-mitochondrial antibodies were positive (1:80). The viral infection panel and anti–smooth muscle antibody were negative. Abdominal magnetic resonance imaging revealed cholecystitis and abnormal hepatic enhancement without focal lesions. On the basis of these findings, cholecystectomy and hepatic biopsy were performed and revealed hepatic infiltration by silicone (Fig. 1).
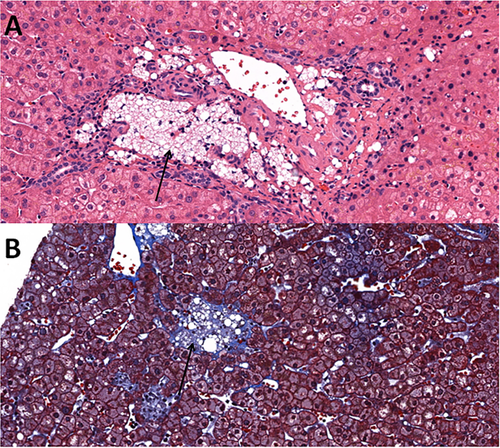
Considering the histopathological findings, history of rupture of the mammary prosthesis and infiltration of Kupffer cells with silicone, in association with Sjögren's syndrome, a diagnosis of ASIA was made. There were no other significant histological findings to suggest any other liver disease.
Chronic cholecystitis was shown in the biopsy of the gallbladder, which was negative for dysplasia or malignancy. Liver enzymes decreased to normal, the abdominal pain improved, and an abdominal CT scan 1 month later revealed a normal-sized liver.
Discussion
ASIA was first presented by Shoenfeld et al.2 in 2011, suggesting major and minor criteria for diagnosis. Our patient had chronic fatigue, myalgias, exposure to adjuvant (breast implant with rupture), and a typical biopsy of an involved organ and evolvement of an autoimmune disease (Sjögren's syndrome); therefore, ASIA was diagnosed. The patient displayed anti-mitochondrial–positive antibodies; however, in the absence of pathologic findings, the diagnosis of primary biliary cirrhosis was ruled out.
ASIA syndrome incorporates five immune-mediated conditions induced by exposure to agents with adjuvant characteristics: postvaccination phenomena and macrophagic myofasciitis syndrome (induced by aluminium hydroxide), as well as Gulf War syndrome probably induced by squalene, siliconosis, and sick building syndrome.3
Silicone implants have been used in various medical devices such as intraocular lenses, artificial heart valves, testicular prostheses, joints, and breast implants.3 A possible association between silicone exposure and autoimmune diseases in genetically prone individuals has been described previously in many studies.4 The silicone can infiltrate body tissues even in the absence of rupture of the prosthesis, inducing a foreign body reaction characterized by activation of immune cells, fibrosis, and formation of silicone-containing granulomas.5
The most frequent symptoms of this syndrome are myalgias, myositis, arthralgia, neurological manifestations, fever, dry mouth, and cognitive alterations. There are also non-specific symptoms such as fever, neurological impairment, skin lesions, and gastrointestinal and respiratory manifestations. In this case, the diagnosis was made formerly with clinical manifestations, then by way of biopsy and the presence of autoantibodies.
A case report of four patients by Nesher et al.5 presented evidence that silicone had infiltrated pulmonary and thoracic lymph node nodules. The investigators found that removal of the adjuvant did not necessarily improve the pathology and that treatment depends on the autoimmune syndrome that was triggered.
This syndrome should be part of the differential diagnosis of a patient with nonspecific symptoms, a history of exposure to an adjuvant, and development of an autoimmune disease.