Immune-monitoring of myelodysplastic neoplasms: Recommendations from the i4MDS consortium
Abstract
Advancements in comprehending myelodysplastic neoplasms (MDS) have unfolded significantly in recent years, elucidating a myriad of cellular and molecular underpinnings integral to disease progression. While molecular inclusions into prognostic models have substantively advanced risk stratification, recent revelations have emphasized the pivotal role of immune dysregulation within the bone marrow milieu during MDS evolution. Nonetheless, immunotherapy for MDS has not experienced breakthroughs seen in other malignancies, partly attributable to the absence of an immune classification that could stratify patients toward optimally targeted immunotherapeutic approaches. A pivotal obstacle to establishing “immune classes” among MDS patients is the absence of validated accepted immune panels suitable for routine application in clinical laboratories. In response, we formed International Integrative Innovative Immunology for MDS (i4MDS), a consortium of multidisciplinary experts, and created the following recommendations for standardized methodologies to monitor immune responses in MDS. A central goal of i4MDS is the development of an immune score that could be incorporated into current clinical risk stratification models. This position paper first consolidates current knowledge on MDS immunology. Subsequently, in collaboration with clinical and laboratory specialists, we introduce flow cytometry panels and cytokine assays, meticulously devised for clinical laboratories, aiming to monitor the immune status of MDS patients, evaluating both immune fitness and identifying potential immune “risk factors.” By amalgamating this immunological characterization data and molecular data, we aim to enhance patient stratification, identify predictive markers for treatment responsiveness, and accelerate the development of systems immunology tools and innovative immunotherapies.
INTRODUCTION
Myelodysplastic neoplasms (MDS) are a heterogeneous group of clonal hematopoietic stem and progenitor cell (HSPC) disorders arising in the bone marrow (BM),1 characterized by ineffective hematopoiesis, dysplasia, peripheral cytopenias, and an increased risk of transformation to acute myeloid leukemia (AML).2, 3 MDS evolve from clonal HSPC outgrowth with the acquisition of genetic lesions and the implementation of genetic alterations into prognostic scoring systems has improved MDS risk stratification.4-6
In addition to cell-intrinsic lesions, increasing evidence suggests that immune disruption and tumoral BM microenvironment alterations occur during MDS pathogenesis.7-10
The association between inflammation and MDS11 is reinforced by their linkage to an autoimmune disorder, present in 10%–20% of MDS patients.12-14 MDS-associated autoimmune disorders are typically refractory to immunosuppressive agents and difficult to manage,12, 15 and are associated with adverse impact on both patients' quality of life and clinical outcome.16 While immunomodulatory therapies may lead to a sustained response in some patients, universally accepted biomarkers that predict such a response are not yet established.17-19
Despite growing evidence highlighting the role of immune dysregulation in the pathogenesis and prognosis of MDS,20, 21 immune therapies remain underutilized in MDS management. Additionally, current diagnostic workups and prognostic models do not typically assess host immunity.5, 22
The International Integrative Innovative Immunology for MDS (i4MDS) initiative, supported by the European Hematology Association (EHA), is a consortium of clinician scientists, biologists, and physicians actively engaged in MDS patient research and clinical care. We envision that incorporating immunological profiling alongside molecular data could enhance patient stratification, uncover predictive treatment response biomarkers, and steer the development of innovative immunotherapies.
In this position paper, we review the main immune cell dysregulation during the disease course and propose comprehensive guidelines to harmonize and routinely implement immune assessment in MDS.
METHODS
Since its establishment in 2023, the i4MDS consortium has grown to encompass 27 centers across 10 countries, selected for their experience in the field of immunology in MDS.
The consortium has conducted several meetings to assess existing literature on immune dysregulation in MDS and to formulate recommendations for the monitoring of immune cells and cytokines.
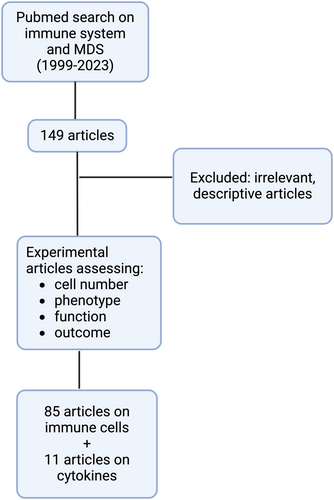
As an initial step, i4MDS conducted a comprehensive literature search, including articles published between 1999 and 2023. This search focused on keywords such as “Myelodysplastic Syndromes” in conjunction with the name of specific immune cell types, including “Cytotoxic T lymphocytes (CTL),” “Regulatory T (Treg) cells,” “T helper (Th) cells,” “Gamma-delta (γδ) T cells,” “B lymphocytes (Ly),” “Natural Killer (NK) cells,” “Dendritic cells (DC),” “Monocytes,” “Macrophages,” “Myeloid-derived suppressor cells (MDSC),” “Mesenchymal Stem cells (MSC),” and “Cytokines.” Articles selected for the review of each immune cell type were included if they explored variations in cell number, phenotype, and/or function among MDS patients (Figure 1).
Second, i4MDS conducted a survey involving eleven hemato-immunological clinical centers with expertise in the field: Leipzig University Hospital (Germany), MLL Munich Leukemia Laboratory (Germany), The National Heart, Lung and Blood Institute (US), Rigshospitalet, University of Copenhagen (Denmark), UMC of Amsterdam (Netherlands), University Hospital of Dresden Carl Gustav Carus (Germany), Vall d'Hebron Hospital (Spain), HMDS of Leeds (UK), Saint-Louis Hospital of Paris (France), and Cochin Hospital of Paris (France). The aim was to identify a core set of immune cell markers for clinical flow cytometry and clinically relevant cytokines for routine assessment in clinical care. The proposed recommendations underwent an iterative panel review process aimed at achieving consensus.
IMMUNE CELL DYSREGULATIONS IN MYELODYSPLASTIC NEOPLASMS
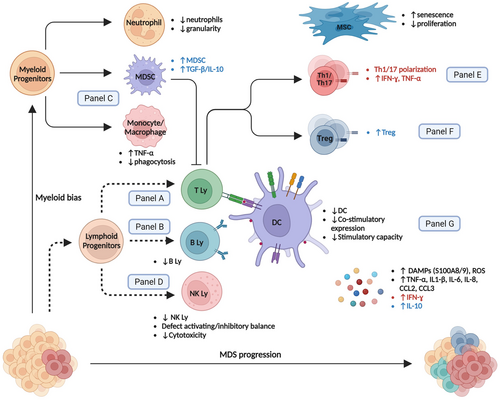
Low-risk (LR) MDS are characterized by a “proinflammatory state” with a higher prevalence of effector cells (e.g., Th17 and CTL)8, 23 whereas high-risk (HR) MDS are dominated by an “immunosuppressive state” with increased regulatory T cells (Tregs).7 We highlight the complex modifications in cell repertoire that occur during MDS progression (Figure 2 and Table 1). Additionally, as malignant stem cells can differentiate into mature immune cells, MDS-related genetic lesions transmitted to downstream myeloid and lymphoid progeny can trigger aberrant inflammatory signaling and contribute to maturation defects and immune dysregulation.106, 107
| Cell type | Number | Phenotype | Function | Outcome | Other |
|---|---|---|---|---|---|
| Neutrophils | ↓ Neutrophils24 ↓ CD54highCD181low subset, especially in HR-MDS7 |
↓ CD4325 and GM-CSF receptor expression26 (PB) |
↓ Phagocytosis7 ↓ Bactericidal and fungicidal activities7 |
Neutropenia correlated with reduced LFS and OS22, 27 | ↓CD54highCD181low correlated with response to decitabine28 (PB) |
| Natural killer cells (NK cells) |
↑ CD56bright/↓ CD56dim NK Cells ratio32 (PB + BM) |
↓ NKG2D, DNAM1, NKp30, NKp46 (activation)32-35 (PB + BM) ↑ TIGIT (inhibitory)36 (PB) ↓ Perforine/Granzyme B (lytic granules29 (PB) ↓ KIR (inhibitory/licensing)32 (PB + BM) |
↓ CD56dim correlated with reduced OS40 (BM) KIR haplotype correlated with reduced LFS and reduced OS41 ↓ cytotoxicity correlated with reduced OS42 (PB) |
NK cells derived from MDS clone38 (PB) ↓ function associated with higher IPSS, abnormal karyotype, excess blasts, and age-adjusted BM hypercellularity37 (PB + BM) ↓ activating receptor expression correlated with elevated BM blasts33 (BM) |
|
Dendritic cells (DC) |
↓ BM DC progenitors21 (PB) ↓ Myeloid cDC46 (BM) ↓ pDC46 (BM) |
↓ CD1a, CD54, CD80 and MHC class II44 (PB) ↓ HLA-DR, CD11c, CD80 and CD86 costimulatory molecules expression47 (PB) |
↓ Allostimulatory capacity44, 45, 48, 49 (PB + BM) ↓ Endocytosis45 (PB) ↑ IL-10 secretion49 (PB) |
↓ CD141High cDC correlated with reduced OS21 (PB) | DC derived from MDS clone43-45 (PB) |
| MDSC | ↑ in HR-MDS10, 50 (PB + BM) | ↑ Production of S100A951 (BM) ↑ IL-10/IL-12 and TGF-β/TNF-α ratio in HR-MDS52 (BM) |
↑ TGF-β/TNF-α ratio correlated with increased blast %52 (BM) | Expansion driven by S100A-CD33 interaction50 (BM) | |
| Monocytes/macrophages | ↑ Total,53 notably in HR-MDS54 (BM) ↓ Classical monocytes55 (PB) |
↑ CD40,56 HLA-DR expression57 (PB + BM) ↑ Thrombomodulin expression in LR-MDS58 (PB) ↓ CD206 and SIRPα expression53 (PB) |
↑ TGF-β54 and TNF-α56, 59 production (PB + BM) ↓ Phagocytic function53 (PB) ↑ Apoptotic index59 (BM) |
↑ BM monocytes correlated with adverse prognosis60 (BM) ↑ CD300E correlated with higher MDS risk and adverse LFS60 (BM) |
|
| T lymphocytes | ↑ Surface expression of activation markers (HLA-DR+, CD57+, CD28−, CD62L−)61 (PB + BM) | T clonality restriction,3, 62 loss of clonal T-cell populations in responders to ATG-based treatment3 | |||
| Cytotoxic T cells (CTL) | ↑ Effector CTL (CD57+)63-65 (PB + BM) ↓ Total CTL66 (PB) |
Exhausted (expression of TIM3, CD39, PD1, CTLA4)32, 52, 66, 67 (PB + BM) WT-1 specific cytotoxic T cells have a unique phenotype with coexpression of CD39 and CXCR468 (PB + BM) Contracted TCR-V β repertoire (clonal/oligoclonal)64, 69 (PB + BM) |
↓ Cytotoxicity65, 66, 70 (PB + BM) Effector CTL inhibits bone marrow hematopoiesis71 (BM) ↑ Tc1/Tc2 ratio72 (PB) |
In patients with abnormal karyotype deprivation of effector T cells increased the proportion of abnormal cells71 (BM) | |
| T regulatory cells (Treg) | In LR-MDS dysfunctional and impaired BM homing, in HR-MDS they retain their function and migratory capacity74 (PB + BM) | ↑ Treg in LR-MDS correlated with adverse prognosis79 (PB + BM) ↑ CD4+ Treg correlated with adverse prognosis7 (PB) In LR-MDS Treg subset CD4(+)FOXP3(+)CD25(+)CD127(low)CD45RA(−) CD27(−) (effector memory Treg) correlated with adverse prognosis80 (PB) ↑ Naïve Treg/induced Treg ratio correlated with adverse prognosis81 (BM) |
↓ In patients responding to treatment (induction cht)74 (PB + BM) | ||
T helper cells (Th) |
↑ Th1/Th2 ratio especially in LR-MDS72, 82 (PB + BM) ↔ Th1/Th2 ratio83 (PB) ↑ Th17 in LR-MDS8, 24, 84, 85 (PB + BM) ↑ Th22 higher in HR-MDS24 (PB + BM) |
↑ CD40L expression56 (PB + BM) | High Th1 correlated with levels of INF-gamma/TNF-α and apoptotic index of nucleated cells82 (BM) ↑ Th17 function in LR-MDS84 (PB + BM) |
↑ IL-17 expression associated with more severe anemia81 (BM) Th17 positive relation with normal karyotype, ANC, and Hb concentration; negative relation with morphologic blast count84 (PB + BM) |
|
| Gamma-delta T cells | ↓ Total gamma delta T cells86 (PB) | ↔ Function86 (PB) | Abnormalities in the Vdelta receptor repertoire87, 88 (PB) | ||
| B cells | ↓ Increase in apoptosis89 and reduced progenitors in LR-MDS90 (BM) | ↓ B progenitors correlated with adverse prognosis79 (PB + BM) | |||
| MSC | ↓ Proliferation91-93 and increased senescence93-95 (BM) | ↔ Phenotype96 (BM) Altered expression of osteopontin, Jagged1, Kit-ligand and angiopoietin91 (BM) |
↓ Supporting hematopoiesis function97, 98 (BM) ↓ Osteogenic differentiation91, 93, 95, 99-102 (BM) ↑ Inhibition of DC differentiation and function in HR-MDS103 (BM) ↑ Production of IL-6 and TNF-α59 (BM) ↑ TGF-β, apoptosis, and immunosuppression in HR-MDS97 (BM) |
Abnormal karyotype104, 105 (BM) |
- Abbreviations: BM, bone marrow; HR, high risk; IPSS, international prognostic scoring system; KIR, killer-cell immunoglobulin-like receptor; LFS, leukemia-free survival; LR, low-risk; MDS, myelodysplastic neoplasms; NK, natural killer; OS, overall survival; p/cDC, plasmacytoid (pDC)/conventional myeloid (cDC); PB, peripheral blood.
CHANGES IN INNATE IMMUNITY
Neutrophils
Functional deficits, including reduced phagocytosis108 and decreased bactericidal and fungicidal activities,109 have been described in MDS neutrophils. Moreover, neutrophils have been found to display an aberrant phenotype with reduced expression of GM-CSF receptor26 and CD43 adhesion molecule,25 correlating with defective chemotaxis mostly in HR-MDS.110 A recent study demonstrated a higher frequency of low-granule neutrophils in individuals with clonal hematopoiesis related to TET2 mutations.111 TET2-inactivated neutrophils had more compact neutrophil extracellular traps (NET) and decreased flow cytometer (FCM) median side scatter (SSC)-assessed granularity. Consistently, decreased granularity has also been reported in MDS patients.112, 113
Natural killer (NK) cells
MDS are characterized by a decrease in NK cells, mostly the mature cytotoxic CD56dim subset, and numbers inversely correlate with disease severity.29, 30, 32 MDS NK cells further show a “less activated” phenotype, reduction of lytic perforin/granzyme granules, and licensing NK Killer Ig-Like Receptors (KIRs) molecule expression.29, 32, 37 These phenotypic alterations further correlate with reduced tumor necrosis factor-α (TNF-α) and interferon-γ (IFN-γ) secretion following interleukin-2 (IL-2) stimulation,29, 33, 38 defective NK in vitro degranulation,33 and reduced cytotoxicity capacities,33, 37, 38 which have been associated with adverse prognosis.42 A recent study correlated the presence of TET2 mutations with reduced KIR expression and impaired NK functions, which were restored with hypomethylating agent (HMA) therapy.114
Dendritic cells (DC)
In MDS, all BM DC subsets show significantly lower frequencies ex vivo or following in vitro generation from DC precursors.43, 46, 48, 115 MDS patients also have reduced numbers of DC progenitors,21 and the reduction in DC further correlates with higher blast percentage and IPSS risk.46 Additionally, CD141high conventional myeloid DC numbers are decreased in MDS patients and correlate with worse overall survival (OS).21 Functionally, MDS DCs have reduced T-cell priming capacities, with clear T helper 1 skewing,48 together with a reduction of their endocytic ability.43 These functional defects are accompanied by a reduction of HLA-DR, CD11c, and costimulatory molecule expression after activation.47, 49
Myeloid-derived suppressor cells (MDSC)
The fundamental MDSC function is to secrete immunomodulatory molecules (arginase-1, indoleamine 2,3-dioxygenase, NADPH-oxidase-2), which suppresses T-lymphocyte proliferation while transforming growth factor-β (TGF-β) and IL-10 promote NK-cell energy and the development of suppressive Treg.116, 117
HR-MDS patients have increased MDSC numbers that correlate with increased Treg levels.10 Consistently, levels of TGF-β and IL-10 are elevated in HR-MDS patients.52 MDSC from MDS patients also display an aberrant chemokine receptor profile with increased CXCR4 and CX3CR1 expression.118
Monocytes and macrophages
While an increase in classical monocytes ≥94%119 is highly suggestive of chronic myelomonocytic leukemia,120 monocyte subset composition in the context of MDS remains controversial. Velegraki et al. reported a higher proportion of CD14+/CD16+ intermediate monocytes in MDS patients,55 while Talati et al. reported increased CD14+/CD16− classical monocytes in SF3B1-mutated MDS.62 Further studies may help elucidate the role of monocyte repartition in MDS and its distinction from chronic myelomonocytic leukaemia, especially in light of the most recent international classifications.2, 3
In MDS, macrophages exhibit an altered phenotype characterized by reduced levels of CD206 and SIRPα,53 along with heightened expression of CD68, CD86, and CD163.121 Functionally, Meers et al. demonstrated an increase in the CD40 (on monocytes)/CD40L (on T Lymphocytes) axis in MDS patients, resulting in elevated TNF-α secretion by monocytes and subsequent hematopoiesis suppression.56 Furthermore, MDS monocytes display impaired ability to differentiate in macrophages and reduced in vitro phagocytic abilities.53, 55
CHANGES IN ADAPTIVE IMMUNITY
T cells
The current body of literature strongly indicates the presence of clonal or oligoclonal T-cell expansion as a distinctive feature in MDS.122, 123 These observations support the hypothesis of a dominant clonal T lymphocyte population suppressing hematopoietic precursors, ultimately leading to BM failure.
In one of the largest studies conducted on T cells in MDS patients,61 the numbers of peripheral blood (PB) CD4+ and CD8+ T cells in MDS patients did not significantly differ from those in age-matched healthy individuals. However, there appeared to be a reduction in CD8+ T cells in patients with high-risk (HR) disease. Additionally, the authors verified that most T cells exhibited an activated phenotype, both in PB and BM. This activation was characterized by heightened expression of HLA-DR and CD57, coupled with diminished expression of CD28 and CD62L. Importantly, the presence of this activated phenotype did not appear to influence symptoms, prognosis, or risk of disease progression.61 Furthermore, T cells derived from MDS patients exhibited elevated expression of chemokine receptors CCR3, CCR5, and CX3CR1, while showing reduced expression of CCR7. This pattern suggests that T cells in MDS tend to possess a more mature chemokine receptor profile.124 Hypocellular MDS seem to be characterized by clonal T and NK cell expansions, respectively in HR and LR MDS.125
Cytotoxic CD8+ T cells
Multiple studies have consistently depicted a cytotoxic environment in low and intermediate-risk MDS. This is evidenced by several factors, including the expansion of mature effector CTLs (CD8+, CD28−, CD57+), heightened expression of granzyme B and perforin, alterations of TCR-Vβ repertoire, and reduced frequencies of Tregs when compared to healthy individuals.63-65 This augmented cytotoxicity has a dual impact: first, it suppresses BM hematopoiesis and contributes to cytopenias; second, CTLs exhibit heightened activity against MDS cells, underscoring their role in restraining the malignant clone.71
With the progression of MDS alterations in the immune microenvironment hinder effective anti-tumor responses. Yang et al. revealed that PD-1 and its two ligands, PD-L1 and PD-L2, along with CTLA-4, were aberrantly upregulated in BM cells from patients with myeloid disorders. This upregulation predisposes individuals to an exhausted CTL phenotype, allowing the malignant clone to evade immune surveillance.67 This finding aligns with another study that reported reduced cytotoxic capacity in high-risk MDS patients.65
CD4+ T helper cells (Th)
In MDS, there is an elevation in the Th1/Th2 ratio, characterized by a Th1 bias in patients with LR-MDS. Two studies have demonstrated a correlation between Th1 bias and the presence of proapoptotic cytokines, such as IFN-γ and TNF-α. This suggests that Th1 cells may contribute to nucleated cell apoptosis, and therefore BM failure, by overproducing proapoptotic cytokines.72, 82
Th17 cells represent a distinct subset of CD4+ T cells, characterized by the production of IL-17. Kordasti et al. found a significantly elevated Th17 population in LR-MDS compared to HR-MDS and controls, together with elevated proinflammatory cytokines and a higher apoptotic index.8 Similarly, Zhang et al. showed elevated levels of IL-17/IL-17R as well as increased levels of the potentially pathogenic cytokines IFN-γ and TNF-α in BM supernatants. Li et al. found a positive correlation between the percentage of Th17 cells, neutrophils, and hemoglobin levels, and a negative correlation with morphologic blast percentage, as well as a significantly lower Th17 frequency in unfavorable karyotype groups. The authors speculate that Th17 may have a protective role in MDS that contributes to malignant clone inhibition as well as sustaining normal hematopoiesis.84
Th22 cells, which mainly secrete IL-22, TNF-α, and IL-13, are markedly elevated in MDS compared with healthy donors, especially in HR-MDS.24 There may be a role of Th22 cells in the immune evasion of MDS clone(s) and disease progression. However, their role may be more complex. Current studies on Th22 in autoimmunity and cancer show a potential biphasic activity, with both inflammatory and immunosuppressive activity, based on the focal microenvironment.24
Regulatory T cells (Tregs)
In HR-MDS, Tregs are increased compared to LR-MDS and controls.7, 73, 126, 127 The expansion is typically polyclonal and involves a predominantly naïve subset.7 High levels of Tregs have been significantly correlated with MDS with excess blasts, high IPSS score, and disease progression.7 In early-stage disease, published results are inconclusive. Some studies show normal or near-normal Treg frequencies,7 whereas others show an increased number compared to healthy controls.77, 78 This may indicate that even LR disease can harbor a dysregulation of immune tolerance, which can negatively affect OS.79 Kotsianidis et al. showed that early and advanced-stage diseases are associated with differential Treg activity.74 In early-stage MDS, Tregs' anti-inflammatory potential is compromised by a suppressed CXCL12/CXCR4 axis due to CXCR4 downregulation and impaired BM homing. As a result, the authors showed a reduction of Tregs in the BM microenvironment, which could be a significant mechanism supporting the autoimmunity and BM failure observed in LR-MDS. In late disease stages, Tregs retain their function and homing and can expand locally and systemically.74 In both early and late-stage disease Tregs show an inverse correlation with the numbers of Th17 and CTL,8, 75 which could permit the emergence of the autoimmune responses observed in the context of LR-MDS.
B lymphocytes
Literature on the role of B cells in MDS pathogenesis is limited. Meers et al. showed that MDS patients had lower B cell counts compared to age-matched controls.61 B-cell progenitors are reduced in MDS patients compared with healthy controls,90 and BM B cells display increased apoptosis. The increase of B progenitors has been shown to correlate with adverse prognosis in LR-MDS.79
CHANGES IN BONE MARROW MICROENVIRONMENT
Smoldering inflammation, particularly driven by NLRP3 inflammasomes and damage-associated molecular pattern (DAMP) molecules (e.g., S100A8/A9) via Toll-like receptors (TLR), is a main feature in MDS.128, 129 Constitutively activated TLR-signaling with downstream mitogen-activated protein kinase (MAPK) and nuclear factor kappa B (NF-κB) activation further induces the release of proinflammatory cytokines propagating the vicious inflammatory loop, increasing pyroptosis and consequently cytopenias.129 TLR activation promotes the secretion of several proinflammatory cytokines, including IL-1, IL-6, IL-8, TNF-α, INF-γ, and GM-CSF, and leads to the priming of inflammasome components and ASC (apoptosis-associated speck-like protein containing a caspase-recruitment domain) protein aggregation into large cytoplasmic aggregates (ASC specks). These large complexes act as adaptors to promote pro-caspase1 activity leading to the conversion of pro-IL1β and pro-IL18 into their active form, further amplifying the inflammatory loop.129 As a result, pyroptosis, a proinflammatory lytic form of cell death, participates in ineffective hematopoiesis.
Kornblau et al. found several upregulated (CSF3, IL-1RA, IL-8, IL-12, IL-15, and CXCL10) and downregulated (IL-4, IL-6, IL-7, IL-10, IFN-γ, CCL3, PDGF-BB) cytokines in PB from MDS patients compared to age-matched controls130 (Table 2). This points toward a profound cytokine dysregulation in MDS patients, which differs according to the MDS risk group. Kordasti et al. reported higher serum levels of proinflammatory molecules, including IL-7, IL-12, RANTES, and IFN-γ in LR-MDS patients, whereas HR-MDS showed higher levels of suppressive cytokines IL-10 and soluble IL2R.8 Feng et al. also observed differential cytokine profiles according to IPSS risk stratification, with decreased levels of CCL5, CXCL5, CD40L, VEGF, and EGF in HR-MDS compared to LR-MDS.131
| Proinflammatory | Anti-inflammatory | Growth factors | Outcome | |
|---|---|---|---|---|
| Cytokines | In all MDS: ↑ IL-1RA, IL-15, TNFα, IL-6,130, 131 IL-8,130, 132 CCL2, CXCL10132; ↓ CCL3,130 CCL4131 (PB + BM) In LR-MDS: ↑ IL-7, IL-12, CCL5, INF-γ,8 IL-178, 133 (PB + BM) In HR-MDS: ↓ IL-1870 (BM) |
In all MDS: ↑ TGF-β,130 IL-27132; ↓ IL-4130 (PB + BM) In HR-MDS: ↑ IL-10, soluble IL-2R8 (PB) |
In all MDS: ↑ G-CSF131 (PB) ↑ VEGFA130 (PB) |
↑ TGF-β correlated with higher BM blasts %54 (BM) ↑ TNF-α correlated with higher BM blasts %, adverse prognosis134 (PB) ↑ IL-6, IL-7, and CXCL10 correlated with adverse prognosis135 (PB) |
- Abbreviations: BM, bone marrow; PB, peripheral blood.
Interestingly, some studies reported a correlation between cytokine levels with clinical outcomes. Tsimberidou et al. found that higher TNF-α levels (>10 pg/mL) were associated with lower rates of responses and significantly lower event-free survival and OS.134 Additionally, increased serum CXCL10, IL-7, and IL-6 levels were independently associated with adverse OS in a retrospective series of 79 patients.135
Mesenchymal stromal cells (MSC)
Numerous reports found that MDS MSC exhibit functional defects in vitro,91 such as increased senescence, a decline in proliferation ability,136, 137 and a decreased osteogenic potential.91, 138, 139 Perhaps most importantly, MDS MSC showed altered capacities to sustain HSPC maintenance both in MDS animal models140 and in in vitro cocultures.91 This could be partly attributed to the reduced expression of essential HSPC ligands, including CXCL12, ANGPT1, and KITL,141 coupled with higher production of the proinflammatory cytokines IL-6 and TNF-α.59
There is very little data regarding the dysregulation of other stromal and vascular niche cells in the context of MDS, however, BM stromal fibroblasts of MDS patients have also shown altered cytokine expression, including IL-6, TNF-α, IFN-y, and TGF-β.142
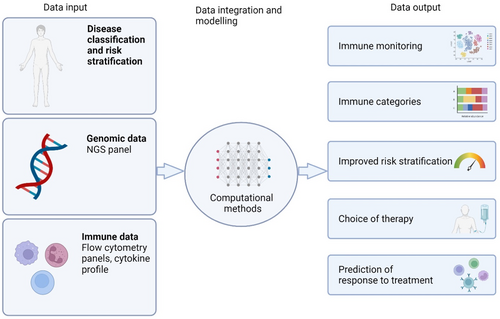
In summary, MDS is characterized by a multitude of intricated and interconnected dysregulations within cellular immunity and the BM microenvironment. These dysregulations exhibit heterogeneity across MDS subtypes, genetic mutations, and disease stages. This diversity underscores the importance of establishing standardized FCM panels and cytokine measurements for in-depth exploration of immunity in MDS and for risk stratification (Figure 3).
RECOMMENDATIONS FOR IMMUNE PROFILING IN MDS PATIENTS
Guided by current knowledge and expert consensus, the i4MDS consortium presents the following recommendations as an initial step toward standardizing the assessment of immune parameters in patients with MDS.
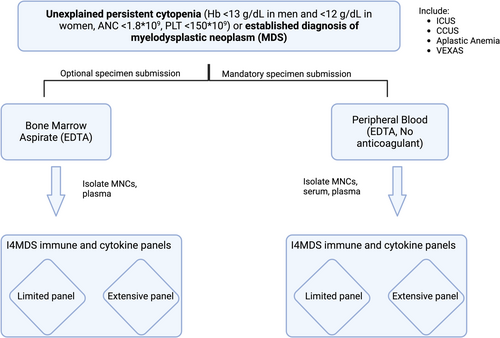
All patients, whether they are under evaluation due to suspicion of MDS or have a confirmed diagnosis, should be requested to provide prescreening consent. This consent allows for the collection of the necessary samples for local or centralized immune profiling and the ongoing storage of research samples for future evaluations. Besides patients with suspected/diagnosed MDS, patients who are currently undergoing evaluation for persistent unexplained cytopenias (Hb <13 g/dL in men and <12 g/dL in women, ANC <1.8 × 109, PLT <150 × 109) as well as those who have already received a diagnosis of immune aplastic anemia, clonal cytopenia of undetermined significance (CCUS), VEXAS syndrome, or idiopathic cytopenia of undetermined significance (ICUS) are considered eligible for participation (Figure 4). When possible, patients will be part of registries where central diagnosis screening is not prohibited.
Concomitant clinical data to be collected should include coexisting conditions (especially autoinflammatory and autoimmune disorders) and immunomodulatory drugs (especially systemic steroids >10 mg/day). Laboratory data should include CRP and autoimmunity-related tests if indicated and available. Molecular sequencing (standard MDS NGS panels) should also be performed in all patients, to complement both molecular and immune data.
We recommend the collection of PB and, if feasible, BM aspirates to monitor the immune signature. Notably, significant variations in the innate and adaptive cell composition and status between peripheral and BM samples can provide valuable insights into the mechanisms underlying defective immune surveillance. Aspirates should be performed at the time of diagnosis and before initiating any new therapies.
We strongly encourage sequential assessments in accordance with institutional guidelines to monitor the dynamic evolution of the immune response during treatment. This is particularly crucial for patients undergoing treatment with hypomethylating agents (HMA) for a minimum of three cycles, given the potential immunomodulatory properties of this therapy.
When feasible, a portion of the PB and BM mononuclear cells and serum samples should be biobanked to enable more advanced multiparameter technologies, such as cytometry by time of flight or spectral flow cytometry, which can facilitate more in-depth immune profiling. Thus, the collection of these important immunological and clinical/demographic data will enable advanced analyses to answer outstanding research questions to improve the experience and outcomes of patients with MDS.
IMMUNE CELL MONITORING USING FLOW CYTOMETRY
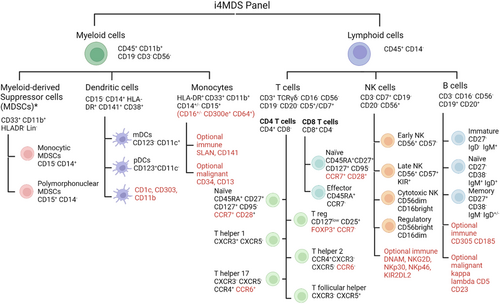
Table 3 summarizes the primary antigens the i4MDS panel recommends for the identification, characterization, and functional assessment of immune cells during clinical care. For each type of immune cell lineage, we have devised a suggested panel along with optional markers. The selection of these additional markers should be guided by local protocols, equipment availability, available resources, and the source of aspirates.
| Panel | Immune subsets | Recommended markers | Optional (immune) | Optional (malignant) |
|---|---|---|---|---|
| A | T cell | CD45, CD45RA, CD3, CD4, CD8, CD5, CD7, CD16/56, CD27, TCRγδ | HLADR, CD38, CD95, CD62L, CD45RO, PD1/CTLA4/TIM3 | TRBC1, CD26 |
| B | B cell | CD45, CD20, CD19, CD10, CD27, CD38, IgD, IgM, CD25, CD22 | CD305, CD185 | kappa, lambda, CD5, CD23 |
| C | Monocyte/MDSC | CD45, CD14, CD16, CD64, CD300e, CD56, HLADR, CD11b, CD33, CD15, Lin | SLAN, CD141, CD45RO | CD34, CD13 |
| D | NK cell | CD7, CD56, CD8, CD94, CD57, CD161, CD16, CD3, KIR3DL1/DL2, CD45RO | DNAM1, NKG2D, NKp30, NKp46, KIR2DL2 | |
| E | T cell subset − 1 | CD3, CD4, CD8, CD19, CD25, CD127, CXCR5, CXCR3, CCR4, CCR6 | CD95, CD28, CCR7 | |
| F | T cell subset − 2 | CD45RA, CD3, CD4, CD25, CD127, CD194 (CCR4), CD95, CD28, CCR7, CD8 | FOXP3, CXCR5, CXCR3, CCR6, CD45RO | |
| G | Dendritic cells | CD45, Lin, CD123, CD88, HLADR, CD5, CD11C, CD141, CD163, CD11B, CD14 | CD1c, CD303, CD11b. CD45RO |
- Note: Each panel explores a specific immune subset with a set of core markers and additional extra-markers to explore their status and function (immune) or known to be dysregulated in the context of cancer (malignant).
This approach has been designed to facilitate effective and routine immune cell assessment in clinical laboratories, particularly in secondary and tertiary centers.
In the case of BM, hemodilution should be prevented, if possible, by using the first aspirate pull. Samples can be collected in ethylenediaminetetraacetic acid tubes and processed up to 72 h after collection. Nevertheless, if high dimensional flow cytometry is to be performed, we would generally recommend citrate collection tubes as they allow both genomic and flow cytometry analysis from the same sample. We recommend ammonium chloride (homemade or commercially available) lysis of mature RBC before antibody staining and suspension in paraformaldehyde for data acquisition.143
The panels of marker combinations in Table 3 have been constructed based on 10 colors FCM, CD45 hematopoietic marker, and a viability stain.132 Optional markers are proposed for exploring cell type-specific functions (immune-related) or those known or suspected to be dysregulated in the context of MDS (malignancy-related).
In the case of BM aspirates, we also recommend the addition of a combination that includes CD34 and other appropriate markers to distinguish hematopoietic stem and progenitor cells (HSPC). Based on the current level of evidence regarding alterations in cell types in MDS (as outlined in Table 3), we strongly recommend performing, at a minimum, the T- and B-cell panels. The choice to implement additional panels may be influenced by the intended treatment strategy.
We designed specific tubes for T-cell monitoring (Panel A) and set a core panel of markers to distinguish cytotoxic, Th, and Tregs, as well as their naïve/memory phenotype (Panels E and F). For both Th (CXCR3, CCR4, CCR6, and CXCR5) subsets and Treg (CD25, CD127), cell-surface identifying markers were preferred given their good correlation with intracellular staining and to facilitate routine implementation.144 Panel B explores B cell isotypes, activation status, and repartition. NK cell panel D discriminates CD56bright/dim NK subsets and major activating/inhibitory/licensing NK receptors known to be dysregulated in MDS. Myeloid panel C investigates monocyte (classical, nonclassical, and intermediate) subsets along with M-MDSC and PMN-MDSC based on CD14/15 differential expression, while panel G analyzes plasmacytoid and myeloid DC subsets (Figure 5).
Neutrophils can be individualized based on FSC/SSC scales and assessed for SSC-based granularity. Given the lack of data regarding the immune impact of red cell nucleated progenitors and megakaryocytes in MDS, we do not recommend their monitoring in routine workup of MDS immune profiling.
CYTOKINE MONITORING IN MDS PATIENTS
Cytokine detection has classically used enzyme-linked immunosorbent assays (ELISA), whose routine implementation has been limited by the analysis of one analyte at a time, and a relatively large sample volume to ensure accurate detection.145 Multiplex immunoassays overcome the limitations of single-analyte ELISA allowing simultaneous analysis of multiple cytokines with a reduced sample volume. While routine implementation of cytokine analysis is not yet widespread, we feel these techniques will play an important role in the therapeutic management of many inflammatory diseases, including MDS.
Serum cytokine levels have been shown to robustly reflect BM cytokine concentration8 and there is high agreement between serum and plasma concentrations.146 Peripheral blood serum (5 mL dry tube) should be the preferred source for cytokine analysis, although we also encourage BM supernatant biobanking. Lastly, it is crucial to exercise diligence regarding the patient's clinical condition to prevent sample collection during concurrent inflammatory or infectious episodes that could confound results. Additionally, any ongoing treatments, particularly those involving growth factors, immunomodulators, or novel inflammasome inhibitors, should be documented and reported, as they have the potential to impact result interpretation.
Table 4 summarizes the recommended cytokine panel, ranked in priority order established based on their potential role in disease genesis and their reported altered expression in MDS patients. Multiplex assays may allow simultaneous analysis of both pro-inflammatory (IFN-γ, TNF-α, IL-1β, IL-1RA, IL-2, IL-2R, IL-6, IL-7, IL-8, IL-12, VEGF, GM-CSF, CCL2, CCL3, CCL4, CCL5, CXCL10) and anti-inflammatory (IL-4, IL-10, TGF-β) molecules known to be dysregulated in the context of MDS. We also suggest additional markers: IL-5 and IL-15 for their broad proinflammatory roles in granulocyte stimulation, NK and T cell activation and proliferation, respectively; CXCL9 and CXCL12 for their important function in immune cell migration toward inflamed and BM tissue, respectively.
| Cytokine panel | Recommended Markers (ranked in priority order) | Optional markers |
|---|---|---|
| Cytokines | IFN-γ, IL-6, IL-8, IL-1RA, IL-7, IL-12, CCL5, IL-10, IL-2, IL-2R, TNF-α, IL-17, IL-1β, TGF-β, VEGF, GM-CSF, CXCL10, IL-4, CCL2, CCL3, CCL4, CXCR4 | IL-5, IL-15, CXCL9, CXCL12, CXCR1, CXCR2 |
DISCUSSION AND FUTURE DIRECTIONS
In this work, we offer recommendations to establish a structured framework for evaluating immune cells and monitoring cytokine changes at the time of diagnosis and throughout the course of the disease to standardize the immune profiling of MDS patients. Currently, manual gating and expert analysis remain the conventional practices, but we anticipate that automated gating and cell identification algorithms, currently in development or used in research studies,147 will likely find their place in clinical practice in the near future.
Looking ahead, more sophisticated technologies, such as mass cytometry or spectral flow cytometry, could become readily available. These advancements have the potential to streamline the monitoring process, potentially reducing the need for multiple tubes and enhancing the efficiency of immune profiling.
We envision the integration of comprehensive immunological data with existing genomic analyses through the setup of a big data consortium. Through advanced statistical analysis, this could lead to improved risk stratification, identification of new prognostic biomarkers and patient subsets most likely to benefit from immunomodulatory treatments, including allogeneic hematopoietic stem cell transplantation and emerging immunotherapies.
AUTHOR CONTRIBUTIONS
Shahram Kordasti, Uwe Platzbecker, Catherine Cargo, Matteo G. Della Porta, and Lionel Adès designed the study and immune panels and supervised the project. Cristina A. Tentori and Lin P. Zhao performed the research, contributed to the panel design, and wrote the manuscript. Benedetta Tinterri, Kathryn E. Strange, Katharina Zoldan, Konstantinos Dimopoulos, Xingmin Feng, Elena Riva, Benjamin Lim, Yannick Simoni, Vidhya Murthy, Antonella Poloni, Eric Padron, Bruno A. Cardoso, Michael Cross, Susann Winter, Aida Santaolalla, Bhavisha A. Patel, Emma M. Groarke, Daniel H. Wiseman, Katy Jones, Lauren Jamieson, Charles Manogaran, Naval Daver, Laura Gallur, Wendy Ingram, P. Brent Ferrell, Katja Sockel, Nicolas Dulphy, Nicolas Chapuis, Anne S. Kubasch, Astrid M. Olsnes, Austin Kulasekararaj, Hugues De Lavellade, Wolfgang Kern, Mieke Van Hemelrijck, Dominique Bonnet, Theresia M. Westers, Sylvie Freeman, Uta Oelschlaegel, David Valcarcel, Marco G. Raddi, Kirsten Grønbæk, Michaela Fontenay, Sanam Loghavi, Valeria Santini, Antonio M. Almeida, Jonathan M. Irish, David A. Sallman, Neal S. Young, AH, and Arjan A. van de Loosdrecht contributed to panel design and critically reviewed the manuscript.
CONFLICT OF INTEREST STATEMENT
Shahram Kordasti: Novartis: Advisory Board, Speakers bureau, Alexion: Speakers bureau, Beckman Coulter: Speakers bureau, MorphoSys: Research Support (none is related to this publication). Wolfgang Kern declares part-ownership of MLL Munich Leukemia Laboratory. Austin Kulasekararaj: Research support (to institution): Celgene/BMS and Novartis. Speaker's fees: Alexion/AstraZeneca, Akari, Apellis, Celgene/BMS, Novartis, Pfizer, Ra Pharma/UCB, Roche, SOBI. Scientific advisory board: Alexion/Astra Zeneca, Apellis, Amgen, Agios, Biocryst, Celgene/BMS, Novartis, Pfizer, Regeneron, Roche, SOBI, Janssen, Samsung and Novo Nordisk (none is related to this publication).
FUNDING
This work was supported by the CRUK City of London Centre Award [CTRQQR-2021/100004] at KCL. C. A. T. is supported by SIE—Società Italiana di Ematologia and the Association “Amici di Beat Leukemia Dr. Alessandro Cevenini ONLUS” (www.beat-leukemia.org). M. G. D. P. is supported by European Union-Next Generation EU-NRRP M6C2 (Investment 2.1 Enhancement and strengthening of biomedical research in the NHS—Project PNRR-MAD-2022-12376695); AIRC Foundation (Associazione Italiana per la Ricerca contro il Cancro, Milan Italy—Project #22053); 5 × 1000 MYNERVA (Myeloid Neoplasms Research Venture AIRC-project #21267). V. S. is supported by AIRC project IG 26537-2021.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in Pubmed at https://pubmed.ncbi.nlm.nih.gov/.