Cost-effectiveness analysis of public health interventions with impacts on health and criminal justice: An applied cross-sectoral analysis of an alcohol misuse intervention
Abstract
Cost-effectiveness analyses of health care programs often focus on maximizing health and ignore nonhealth impacts. Assessing the cost-effectiveness of public health interventions from a narrow health care perspective would likely underestimate their full impact, and potentially lead to inefficient decisions about funding. The aim of this study is to provide a practical application of a recently proposed framework for the economic evaluation of public health interventions, evaluating an intervention to reduce alcohol misuse in criminal offenders. This cross-sectoral analysis distinguishes benefits and opportunity costs for different sectors, makes explicit the value judgments required to consider alternative perspectives, and can inform heterogeneous decision makers with different objectives in a transparent manner. Three interventions of increasing intensity are compared: client information leaflet, brief advice, and brief lifestyle counseling. Health outcomes are measured in quality-adjusted life-years and criminal justice outcomes in reconvictions. Costs considered include intervention costs, costs to the NHS and costs to the criminal justice system. The results are presented for four different perspectives: “narrow” health care perspective; criminal justice system perspective; “full” health care perspective; and joint “full” health and criminal justice perspective. Conclusions and recommendations differ according to the normative judgment on the appropriate perspective for the evaluation.
1 INTRODUCTION
1.1 Economic evaluation of public health interventions
Cost-effectiveness analysis (CEA) methods widely used for the evaluation of health care interventions often focus on the goal of health maximization and fail to capture nonhealth benefits (Edwards, Charles, & Lloyd-Williams, 2013; Kelly, McDaid, Ludbrook, & Powell, 2005). However, public health interventions may generate wider consequences in the economy than those relating to health alone, and they often involve multiple decision makers with different objectives (Claxton, Sculpher, & Culyer, 2007; Claxton, Walker, Palmer, & Sculpher, 2010; Sculpher, Walker, Hinde, & Claxton, 2014; Walker, Griffin, Asaria, Tsuchiya, & Sculpher, 2019). For example, in the context of alcohol misuse, a focus on health maximization may be too narrow because an intervention to reduce alcohol consumption may affect criminal behavior (Coast, Smith, & Lorgelly, 2008). Similarly, an intervention to reduce reoffending may also improve offenders' health, through improved mental health and reduced substances misuse (Perry et al., 2009), and prevent negative impacts on crime victims' health (Dinisman & Moroz, 2017). Assessing the cost-effectiveness of a public health intervention from a narrow health care perspective would likely underestimate its full impact (Claxton et al., 2007), and potentially lead to inefficient decisions about funding (Coast et al., 2008).
Alternative methods, such as cost-benefit analysis (CBA) and social return on investment (SROI), could in principle incorporate broader societal benefits and costs of public health interventions (NICE, 2012). However, these approaches have potential limitations (Edwards et al., 2013; Muyambi et al., 2017). Even though the adoption of a “societal perspective” is recommended in the literature (Jonsson, 2009; Weinstein, 1990), the interpretation and operationalization of a “societal” economic evaluation is subjective; analyses conducted from a societal perspective often merely include productivity costs in addition to health effects and costs (Drost, van der Putten, Ruwaard, Evers, & Paulus, 2017). Moreover, even if a clear societal perspective was defined, a cost-benefit analysis conducted from a single societal perspective could only assist a hypothetical decision maker responsible for allocating resources to public health interventions. By contrast, in reality, different stakeholders are involved in and affected by the delivery of these programs, and each has particular remits and outcomes of interest. Such analyses would ignore objectives and responsibilities of decision makers (Walker et al., 2019), and it would be unclear how to use their results to inform resource allocation choices (Claxton et al., 2010).
Furthermore, economic evaluations that address a singular decision maker with a societal perspective may struggle to capture appropriately the implications in terms of value forgone from alternative activities in each sector. CBAs and SROIs, but also other approaches such as multicriteria decision analyses, typically ignore that resources required to deliver a public health program may be provided by diverse sources, and may come from multiple sectors (Sculpher & Claxton, 2012). Stakeholders in different sectors have different budgetary and resource constraints. Therefore, opportunity costs (i.e., what could have been obtained if the resources would have been used for other activities) are different in different sectors (Sculpher et al., 2014). Lastly, applied CBAs and SROIs frequently lack in transparency about the details of the analysis (Hutchinson et al., 2019), obscure the methods used to value and combine outcomes (Culyer & Chalkidou, 2019), and ignore distributional concerns across population groups (Vining & Weimer, 2010). However, despite these issues, the single sector CEA is still the dominant approach for NICE public health evaluations (Owen, Pennington, Fischer, & Jeong, 2018). Further research is thus still required particularly in areas such as: investigating appropriate perspectives for economic evaluations of public health interventions, considering outcomes across different sectors, and valuing externalities of changes in health (Neumann et al., 2018; Sanders et al., 2016).
1.2 Assessing the impact of alcohol use disorder in the United Kingdom
In the United Kingdom, alcohol use disorder is not only a main public health issue (WHO, 2014), but also a major factor in crime and antisocial behavior. Around three-quarters of those who come into contact with the UK's criminal justice system (i.e., those in police custody, probation settings and the prison system) have a problem with alcohol, and over a third are dependent on alcohol (Hansard, 2016). In England and Wales, in 39% of violent incidents committed in 2017/18, the victim believed the offender to be under the influence of alcohol (Office for National Statistics, 2019). In 35.8% of sexual assault cases recorded in 2016/17, the offender was under the influence of alcohol (Office for National Statistics, 2018). Alcohol imposes significant costs on the NHS and the criminal justice system with alcohol related crime and social disorder estimated to cost the UK tax payers £11bn per year (Institute of Alcohol Studies, 2016). As such, there is a need for cost-effective interventions to reduce the harmful effects on health and criminal justice of alcohol misuse.
However, incorporating the broader impacts of alcohol interventions into an economic evaluation presents various methodological challenges. Most studies identified in a recent systematic review of economic evaluations of alcohol prevention interventions conducted their analysis from a narrow health care perspective. Furthermore, in some of the studies claiming to have considered a societal perspective, there was a discrepancy between the stated and inferred perspectives, and generally they considered only a very narrow range of costs. Some studies considered costs falling on other sectors, such as education, or cost-savings to the criminal justice sector as a result of reducing violence levels and thus avoiding resultant costs to the judicial system. Nevertheless, none of these studies adopted the same broader perspective for the outcomes, and included nonhealth outcomes relevant to the general use of non-health care resources (Hill, Vale, Hunter, Henderson, & Oluboyede, 2017).
1.3 Applied cross-sectoral analysis of an alcohol intervention
The aim of this work is to illustrate how to conduct an economic evaluation of an alcohol misuse intervention to inform decision makers in health care and in criminal justice in a transparent manner using a case study of a public health intervention to reduce alcohol consumption among offenders. To investigate cost-effectiveness, a cross-sectoral economic evaluation based on recently proposed analytical framework was conducted (Walker et al., 2019). The framework was developed to inform the economic evaluation of policies with costs and outcomes falling on different sectors (e.g., health, criminal justice, and education) and involving different decision makers. It extends the “impact inventory” developed by the Second Panel on Cost-Effectiveness in Health and Medicine (Sanders et al., 2016) by considering all affected individuals and reflecting how outcomes attributed to an intervention can be compared with outcomes forgone as a result of resources not being available for other purposes. Further, it makes explicit the valuation used to combine outcomes across individuals and dimensions, and allows for the incorporation of distributional concerns across population groups.
Following the proposed framework, the program is described in terms of its impacts on a set of dimensions of interest to decision makers. Direct effects and the opportunity costs (Sculpher, Claxton, & Pearson, 2017) in each sector of the economy are distinguished, and cataloged in a structured table (extended impact inventory; Walker et al., 2019). Various perspectives for the analysis are considered and measurable facts and value judgments required to consider alternative perspectives are made explicit. An economic evaluation based on this framework can take into account the different objectives, remits, and budget constraints of the stakeholders. However, this framework is not proposed as an alternative to a CBA or SROI type of approach, indeed both such approaches can be captured within this framework. It outlines a step by step process that ensures that the economic evaluation is conducted and reported in a way that makes explicit value judgments and that takes account of the opportunity costs.
This is the first applied economic evaluation conducted alongside a randomized controlled trial using the approach proposed by Walker et al. (2019). For this, the Screening and Intervention Program for Sensible drinking (SIPS) trial was selected. This trial, conducted in probation services looked at screening and brief interventions for reducing hazardous and harmful alcohol use (Newbury-Birch et al., 2014).
2 METHODS
2.1 SIPS trial
SIPS trial was a prospective factorial pragmatic cluster randomized control trial. The target population is constituted by offenders on probation. Individuals on probation are serving their sentence, but are not in prison and are being observed and managed within the criminal justice system by offender managers. While on probation, they may have to: do unpaid work; complete an education or training course; get treatment for addictions, like drugs or alcohol; have regular meetings with an offender manager (Government of the United Kingdom, 2020). Therefore, they can access the same health services as others in the general population, but may be required to utilize additional health services prescribed under the terms of their probation. Offender managers were randomized to provide one of three interventions to offenders under their management who had been identified as having issues with alcohol. The three interventions were of increasing intensity (and associated resource requirement): (i) a client information leaflet (CIL); (ii) CIL and brief advice (BA); and (iii) CIL, BA, and brief lifestyle counseling (BLC). Two hundred and twenty-seven offender managers and 525 offenders were included in the trial and outcomes measures included health-related quality of life and reconvictions of the offenders. Resource use information was also available, including for the intervention and any health care resource use of the offenders. Further details of the trial can be found elsewhere (Newbury-Birch et al., 2009, 2014) and in Supporting Information 1.
2.2 Direct effects
The effects of the intervention on the health-related quality of life of the offenders were measured by the EQ-5D-3L instrument at baseline, 6 and 12 months. The EQ-5D-3L is a 5 dimension, 3 level questionnaire which describes 245 health states, each of which has an associated score based on the UK general population preferences, with 1 representing perfect health and 0 death (Kind, Hardman, & Macran, 1999; Oemar & Oppe, 2013). Quality-adjusted life years (QALYs) were calculated for each individual using linear interpolation and the area under the curve method over the 12 month period (Drummond, Sculpher, Claxton, Stoddart, & Torrance, 2015). The effects of the intervention on criminal justice outcomes were recorded in terms of numbers of reconvictions. Two alternate sources of information for criminal events were available; evidence from the Police National Computer database, which contained evidence on reconvictions, and self-reported details on the types of crimes committed by the offenders. The primary analysis used the number of reconvictions by each offender, as measured in the Police National Computer database. Because no details about each reconviction episode were available, information on the number and type of self-reported crimes was used to estimate the prevalence of specific crimes underlying the database recorded reconvictions. It was assumed that the criminal events leading to reconvictions measured in the Police National Computer database followed the same distribution of the criminal events self-reported by the offenders in the trial (Supporting Information 2). The number of reconvictions was not adjusted to match the number of self-reported crimes. QALY loss estimates for specific crimes in the literature (Dolan, Loomes, Peasgood, & Tsuchiya, 2005; Dolan & Peasgood, 2007) were used to estimate impacts on crime victims' health.
2.3 Costs
Costs considered included costs of the interventions, NHS resource use by trial participants, costs to the criminal justice system associated with reconvictions, and NHS resource use resulting from treating victims of crimes. Intervention costs included staff time, staff training costs, and costs of materials (including screening tools). Intervention costs vary by the intervention delivered, the screening method, and the staff grade delivering the intervention. These costs were considered to fall on the criminal justice sector. Trial participants completed NHS resource use questionnaires at baseline, 6 and 12 months that included: accident and emergency visits, inpatient nights, outpatient visits, day case visits, ambulance use, GP visits (in practice and home visits), nurse visits (in practice and home visits), community mental health worker and social worker visits. The use of these services was combined with unit costs to estimate costs to the NHS (Curtis, 2013; Department of Health, 2010). Reconviction episodes were combined with unit costs to estimate costs falling on the criminal justice system budget. Unit costs included all the costs in response to crime, namely: police activity, prosecution, magistrates’ court, crown court, jury service, legal aid, non-legal-aid defense, probation service, prison service, other criminal justice system costs, criminal justice system overhead, and Criminal Injuries Compensation Authority costs (Akhtar et al., 2011; Brand & Price, 2000; Dubourg, Hamed, & Thorns, 2005; Leontaridi, 2003). An average cost of £976 per reconviction episode was estimated; this was obtained as a weighted average of the costs associated with each specific crime committed, using the frequency of events self-reported by offenders enrolled in the trial as weights. Further, the NHS also incurs different costs to treat victims of various types of crimes (Dubourg et al., 2005). Each crime committed was thus linked with the appropriate unit costs of treating a victim of that particular type of crime to estimate the additional costs falling on the health care budget resulting from treating victims of crimes. Costs falling on health care and criminal justice budgets were kept separate and not aggregated. On the basis of surveys’ date of completion, 2010 was used as reference year for the analysis, and all costs are presented in 2010 pounds.
2.4 Opportunity costs
Additional costs falling on NHS or criminal justice budgets result in resources not being available for other activities which produce health or reduce crime, respectively (the opportunity costs). Conversely, any cost savings free up resources to be used for other activities. The health opportunity cost of NHS expenditure is based on recent estimates of the marginal productivity of the health sector (Claxton et al., 2015). Similar estimates of the marginal productivity of the criminal justice sector in preventing reconvictions are unavailable. Therefore, it was assumed that at the margin a pound spent in any public sector of the economy at the margin generates the same benefit as a pound spent in another, with benefits based on estimates of individual willingness-to-pay for that sector's outcomes. In other words, the health care and criminal justice sectors are equally funded with regard to the “consumption” value of a pound spent in each (Claxton et al., 2019). The marginal productivity of the criminal justice system was thus calculated based on estimates of the willingness to pay for health and the marginal productivity of the health care sector and the willingness to pay for avoided crimes. Estimates have shown that a QALY is valued at approximately £60,000 in “consumption” terms and the marginal productivity of the NHS is approximately £13,000 per QALY (Claxton et al., 2015) while the consumption value of a crime avoided is roughly £51,000, based on contingent valuation estimates from the US weighted by the types of crime committed in the United Kingdom (see Supporting Information 3 for further details; Chaplin, Flately, & Smith, 2011; Cohen, 2015; Cohen, Rust, Steen, & Tidd, 2004). Assuming that the value is the same for a crime and a reconviction averted, the marginal productivity of the criminal justice sector in preventing reconvictions was estimated to be approximately £11,000 per reconviction averted. Opportunity costs in criminal justice system resulting in reconvictions avoided also generate health consequences in terms of impacts on victims of crime. When the resources for their programs are displaced, unidentifiable “generic” offenders might commit crimes. The distribution of types of crimes associated with additional reconvictions that occur as a result of displaced criminal justice costs was estimated using frequencies of criminal events committed in the United Kingdom (Chaplin et al., 2011; Supporting Information 2). Resulting consequences from crimes on victims were obtained by linking reconvictions to QALY losses (Dolan et al., 2005) and health services costs (Dubourg et al., 2005).
2.5 Perspectives for the analysis
The economic evaluation was based on the framework by Walker at al. (2019), which captures the impact of SIPS on individuals in terms of health and criminal justice. Estimated direct effects and opportunity costs falling on different groups of individuals and dimensions were categorized in an extended impact inventory. The information in the extended impact inventory was collated and summarized for alternative perspectives. To aggregate the impacts across dimensions and individuals, a within-dimension approach was adopted. Net impacts for each dimension were calculated by aggregating direct effects and opportunity costs across individuals within the dimension; impacts were then aggregated across dimensions at the population level. If direct effects net of opportunity costs were positive from all relevant perspectives, the intervention was described as beneficial. If some dimensions improve while other worsen following the introduction of an intervention, consideration was given to whether compensation or transfers could create a scenario with positive net impacts in each dimension.
The cost-effectiveness of the interventions was considered from four different perspectives. First, a “narrow” health care perspective, to inform decision makers solely focused on health, where only health effects on the recipients of the intervention (direct effects) and health effects on the general population resulting from health care costs incurred by the recipients of the intervention (opportunity costs) are captured. Second, a criminal justice system perspective, to inform decision makers solely focused on criminal justice, where only effects on reconvictions of the recipients of the intervention (direct effects) and change in other crimes resulting from impacts on criminal justice system costs (opportunity costs) are captured. Third, a “full” health care system perspective, where decision makers are solely focused on health, but impacts on health outcomes and health care costs via criminal justice are also captured. Additional impacts include the direct health effects on victims of crime harmed by trial participants (direct victims), and health effects on the general population resulting from additional NHS costs to treat the victims. Furthermore, health effects resulting from the criminal justice system occur because the intervention impacts criminal justice resources that could be used for other activities that would have reduced crime. These additional impacts are on other unidentifiable victims' health, and on their associated NHS costs which impact the general population. In the schematic presented in Figure 1, full impacts on health care budget and health are described by the dashed rectangles A and B, respectively. Additional components comprise: direct impacts on the health of victims harmed by trial participants (C); additional health care costs due to the treatment necessary to assist the direct victims (D); health impacts on unidentifiable victims harmed by unidentifiable offenders and associated health care costs (E).
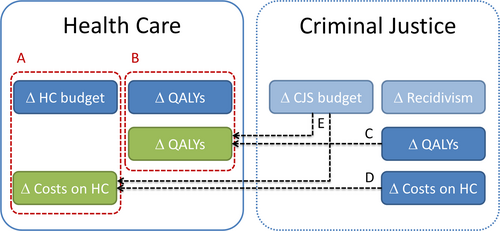
Schematic of the “full” health care system perspective. CJS, criminal justice system; HC, health care; A, full impacts on HC budget; B, full impacts on health; C, D, E, Additional components
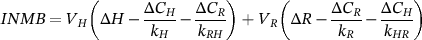 (1)
(1)Equation (1) includes the following measurable values: direct effect on health, including impacts on direct victims (∆H); direct effect on criminal justice (i.e., avoided reconvictions; ∆R); costs falling on health care budget, including those resulting from direct victims (∆C H ); costs falling on criminal justice system budget, including costs resulting from crimes (∆C R ); marginal productivity of the health care sector in generating health (k H ), marginal productivity of the criminal justice system in preventing reconvictions (k R ); marginal productivity of the criminal justice system in generating health (kRH); marginal productivity of the health care sector in preventing reconvictions (k HR). Value judgments included in Equation (1) are: (i) the decision to use only impacts on QALYs and reconvictions; (ii) the social valuation of a health outcome (V H); and, (iii) social valuation of a criminal justice outcome (V R).
It was assumed that no impact on reconvictions is generated from the health care sector (i.e., health care expenditure does not impact crime). By contrast, it was estimated that, on average, for each reconviction avoided, the criminal justice system prevents 0.0081 QALYs being lost by victims, and generates NHS cost savings of approximately £59, which generates an additional 0.0045 QALYs for the general population. Therefore, at the margin, with an investment of £11,000, the criminal justice system can prevent one reconviction and generate 0.0126 QALYs. The marginal productivity of the criminal justice system in generating health was therefore estimated to be £ 870,000 per QALY.
Table 1 summarizes the main components and input values used for the analysis. Additional details about health care unit costs are provided in Supporting Information 4.
3 RESULTS
Results of the economic evaluation are presented for the four different perspectives including through extended impact inventories.
3.1 “Narrow” health care system perspective
From a “narrow” health care perspective, health produced by CIL, BA, and BLC is 0.864 QALYs (95% CI: 0.839; 0.890), 0.854 QALYs (0.830; 0.878), and 0.846 QALYs (0.821; 0.871), respectively. Costs falling on health care budget are £849 (447; 1251), £1223 (844; 1602), and £622 (228; 1017) for CIL, BA, and BLC, respectively. BA and BLC are therefore less effective than CIL (i.e., they result in the offender experiencing less QALYs). BA is more costly than CIL, and is thus dominated (more expensive and less effective). In contrast, BLC is less costly than CIL, and consideration would need to be given to whether the resource savings justify the lower health for the offenders.
Table 2 contains the extended impact inventory for BLC compared to CIL. If the decision maker is solely focused on health, they can compare the direct health effects of the intervention with the health opportunity costs. On average, BLC would result in the offenders receiving 0.018 QALYs less (ΔH). However, the health care savings of £227 (ΔCH) would generate health of 0.017 QALYs for other NHS users. Consideration then needs to be given to the appropriate method for aggregating the impact across trial participants and other NHS users. If the decision maker is willing to aggregate the impacts across the groups with no weighting for different types of individual (i.e. offenders and other NHS users are treated equally), there is a net health loss of 0.001 QALYs from BLC.
| Item | Average cost (in 2010 £) a | Discounted QALY loss | |
|---|---|---|---|
| Health care system | Criminal Justice system | ||
| Health care unit costs | |||
| Drinkline calls | 5 | - | - |
| Counseling | 40 | - | - |
| Day care | 87 | - | - |
| Detoxification | 142 | - | - |
| Outpatient treatment for drinking problems | 87 | - | - |
| Overnight hospital detoxification | 142 | - | - |
| A&E visits leading to not admitted | 97 | - | - |
| A&E visits leading to admitted | 131 | - | - |
| Inpatient nights | 477 | - | - |
| Outpatient visits | 152 | - | - |
| Day case visits | 637 | - | - |
| Emergency ambulance travels | 246 | - | - |
| Ambulance travels | 32 | - | - |
| GP visits | 71 | - | - |
| Nurse visits | 12 | - | - |
| Social worker visits | 53 | - | - |
| Home visit: GP | 147 | - | - |
| Home visit: Nurse | 20 | - | - |
| Home visit: Community psychiatric nurse | 27 | - | - |
| Home visit: Others (e.g., dietitian) | 57 | - | - |
| Home visits: Social worker | 53 | - | - |
| NHS Direct | 28 | - | - |
| NHS Walk in | 37 | - | - |
| Criminal justice unit costs | |||
| Homicide | 950 | 177,859 | 17.791 |
| Wounding | 1662 | 2189 | 0.111 |
| Sexual offences | 1129 | 4067 | 0.160 |
| Rape | 2567 | 4067 | 0.561 |
| Common assault | 152 | 314 | 0.007 |
| Violence | 152 | 314 | 0.007 |
| Robbery | 596 | 3207 | 0.028 |
| Burglary in a dwelling | 0 | 1402 | 0 |
| Theft - not vehicle | 0 | 371 | 0 |
| Theft of vehicle | 0 | 245 | 0 |
| Criminal damage | 0 | 155 | 0 |
| Theft from a shop | 0 | 27 | 0 |
| Drug offences | 0 | 2601 | 0 |
| Driving offences b | 0 | 4231c | 0 |
| Other fines | 0 | 283 | 0 |
| Reconviction episode [CR] | - | 976 | - |
| Intervention costs per person | |||
| CIL | - | 1.04 | - |
| BA | - | 8.55 | - |
| BLC | - | 32.45 | - |
| Marginal productivities | |||
| Marginal productivity of the health care sector in generating QALYs [kH] | £13,000 per QALY | ||
| Marginal productivity of the criminal justice system in preventing reconvictions [kR] | £ 11,000 per reconviction averted | ||
| Marginal productivity of the criminal justice system in generating QALYs [kRH] | £870,000 per QALY | ||
| Value judgments | Consumption value (in 2010 £) | ||
| Social valuation of a QALY [VH] | 60,000 | ||
| Social valuation of a reconviction episode [VR] | 51,000 | ||
- Abbreviation: QALYs, quality-adjusted life years.
- a Unit costs reported in years different from the reference year (2010) were adjusted using the Bank of England Inflation Calculator.
- b No direct impact on health was associated with driving offences because it was assumed that their impacts were already included in the estimate of generic wounding (car accidents were categorized as “serious” wounding).
- c Includes: drink driving arrests, magistrates' courts, and crown courts (including sentencing).
3.2 Criminal justice system perspective
If a criminal justice system perspective is adopted, total incremental costs falling on the criminal justice system budget are given by the sum of intervention costs and cost (saving) per (avoided) reconvictions. Intervention costs (Cint) were estimated to be £1.04, £8.55, £32.45 for CIL, BA, and BLC, respectively. Reconvictions associated with CIL, BA, and BLC are 1.57 (1.15; 1.99), 1.06 (0.74; 1.38), and 0.91 (0.62; 1.21), respectively. Therefore, BA and BLC are associated with 0.51 and 0.66 avoided reconvictions (ΔR) on average, compared to CIL. Given the estimated average cost of £976 per reconviction episode (CR), BA and BLC result in cost savings of £490 and £613 compared to CIL, respectively, including intervention costs (see Supporting Information 5 for further details).
BA and BLC reduce both crime and costs to the criminal justice system compared to CIL (i.e. both dominate CIL). BLC results in a greater reduction in reconvictions and a greater cost saving than BA, and hence dominates BA as well. Table 3 contains the extended impact inventory for BLC compared to CIL. As BLC save costs compared to CIL, if implemented, it would free resources that can be used for other crime averting activities. BLC would reduce criminal justice costs by £613 (negative opportunity costs), resulting in 0.056 reconvictions being averted elsewhere. If the decision maker is willing to aggregate the impacts across different offenders equally there is a net reduction in reconvictions of 0.72.
| Group affected | Direct effects | Opportunity costs |
|---|---|---|
| Trial participants | ΔH = −0.018 QALYs | - |
| Other NHS users | - | ΔCH/kH = −0.017 QALYs |
| Net impact on health | −0.001 QALYs | |
- Abbreviations: BLC, brief lifestyle counseling; CIL, client information leaflet; QALYs, quality-adjusted life years.
3.3 “Full” health care system perspective
BLC results in 0.66 avoided reconvictions compared to CIL, reducing QALYs losses to the victims and the associated health care costs (direct effects). Furthermore, BLC is associated with cost savings for the criminal justice system; therefore, if BLC is implemented, more resources are available and additional crimes can be avoided. These costs savings result in 0.056 avoided reconvictions compared to CIL. Table 4 details the additional impacts of BLC compared to CIL on health and health care costs. Further details on the calculation of QALY impacts and health care costs associated to reductions in crime for both BA and BLC are reported in Supporting Information 6.
| Group affected | Direct effects | Opportunity costs |
|---|---|---|
| Trial participants | ΔR = 0.660 R | - |
| Other offenders | (−CR*ΔR+ΔCint)/kR = −0.056 R | |
| Net impact on crime | 0.716 R | |
- Abbreviations: BLC, brief lifestyle counseling; CIL, client information leaflet; QALYs, quality-adjusted life years.
Table 5 displays the impact inventory for BLC compared to CIL, accounting for the additional impacts on health via criminal justice. BLC results in direct QALY losses for the offenders receiving the intervention, but QALY gains for the direct victims of those offenders. Cost savings for the NHS would result in QALY gains to the general population. Similarly, cost savings to criminal justice would result in other crimes being averted, and QALY gains to the victims of those crimes (unidentified victims). If the decision maker is willing to aggregate the impacts across individuals with no weighting for different types of individual (i.e., offenders, victims and other NHS users are treated equally), there is a net health gain of 0.048 QALYs.
| Additional impacts of BLC compared to CIL | Avoided reconvictions | Impacts on victims' health | Impacts on health care cost |
|---|---|---|---|
| Via direct effects of reduced crime | ΔR = 0.660 | ∆HV = 0.021 QALYs | ∆C Hv = -336.5 £ |
| Via cost savings in the criminal justice system | (−CR*ΔR+ΔCint)/kR =0.056 | ∆H Vu = 0.0005 QALYs | ∆C Hvu = -3.3 £ |
- Abbreviations: BLC, brief lifestyle counseling; CIL, client information leaflet; QALYs, quality-adjusted life years; ∆HV, Health impacts on victims of crimes committed by offenders in the trial; ∆CHv, Additional costs falling on the health care system to treat victims of offenders in the trial; ∆HVu, Health impacts on unidentifiable victims of unidentifiable “generic” offenders; ∆CHvu, Additional costs falling on the health care system to treat unidentifiable victims.
3.4 Joint health and criminal justice perspective
Table 6 provides the impact matrix for BLC compared to CIL, capturing the impact on both dimensions: health and criminal justice. If the decision maker weights all individuals equally, BLC results in both a net health gain and a reduction in crime: as such, BLC improves outcomes for both sectors compared to CIL. Cross-sectoral incremental net monetary benefits (calculated using Equation (1)) are positive and amount to £ 39,056.
| Group affected | “Narrow” health care system perspective | Additional component | “Full” health care system perspective | |||
|---|---|---|---|---|---|---|
| Direct effects | Opportunity costs | Direct effects | Opportunity costs | Direct effects | Opportunity costs | |
| Trial participants | −0.018 QALYs | - | - | - | −0.018 QALYs | - |
| Direct victims | - | - | ∆HV = 0.021 QALYs | - | 0.021 QALYs | - |
| Unidentifiable victims | - | - | - | ∆H Vu = −0.0005 QALYs | - | −0.0005 QALYs |
| Other NHS users | - | −0.017 QALYs | - | (∆CHv+∆CHvu)/kH = −0.026 QALYs | - | −0.044 QALYs |
| Net impact on health | −0.001 QALYs | 0.048 QALYs | 0.048 QALYs | |||
- Abbreviations: BLC, brief lifestyle counseling; CIL, client information leaflet; QALYs, quality-adjusted life years.
| Group affected | Health care system | Criminal justice system | ||
|---|---|---|---|---|
| Direct effects | Opportunity costs | Direct effects | Opportunity costs | |
| Trial participants | −0.018 QALYs | - | 0.66 R | - |
| Other offenders | - | - | - | −0.06 R |
| Direct victims | 0.021 QALYs | - | - | - |
| Unidentifiable victims | - | −0.0005 QALYs | - | - |
| General population | - | −0.044 QALYs | - | - |
| Net impact | 0.048 QALYs | 0.72 R | ||
- Abbreviations: BLC, brief lifestyle counseling; CIL, client information leaflet; QALYs, quality-adjusted life years.
4 DISCUSSION
4.1 Main findings
This cross-sectoral analysis considered the cost-effectiveness of alternative interventions for reducing hazardous and harmful alcohol use in criminal offenders from alternative perspectives reflecting health and criminal justice. From a “narrow” health care system perspective, CIL offered the greatest net health, and BA and BLC should not be introduced. By contrast, from a criminal justice system perspective, BLC was found to be the least costly and most effective, suggesting that BLC should be introduced. From a “full” health care system perspective, BLC offered the greatest net health and should be introduced. From a joint health and criminal justice perspective, BLC resulted in both a net health gain and a net reduction in crime and should be recommended for implementation.
This analysis showed that conclusions and recommendations differ according to the perspective adopted for the evaluation. Furthermore, even when a narrower perspective of health is taken, failing to account for the effects on health via criminal justice results in a failure to consider the full implications for the outcome of interest, and potentially wrong recommendations, as was the case in this analysis.
4.2 Policy implications
The importance of economic evaluation to support decision-making in public health is widely acknowledged, and local authorities showed support for methods that incorporate multiple sector costs and benefits (Frew, 2016). However, in the practice of decisions related to public health, the use of economic evidence is limited. This may be partly due to economic evidence typically not addressing the priorities of multiple stakeholders and not reflecting local authorities' needs of capturing wider non-health outcomes (Frew & Breheny, 2019).
The main objective of this economic evaluation was not to provide a conclusive recommendation specifically about the implementation of SIPS. Instead, SIPS was used as a vehicle to show how to conduct cross-sectoral economic evaluation of an intervention to reduce alcohol misuse that can help to inform multiple heterogeneous decision makers. The applied cross-sectoral analysis demonstrated how a recently proposed analytical framework (Walker et al., 2019) can be used to inform decision making when considering the impacts on both health and criminal justice.
As the purpose of an economic evaluation is to inform decision makers, they should be consulted at study design stage to ensure appropriate information is captured to meet their needs. Their remits and preferences should determine the appropriate outcomes to consider in the analysis. This applied analysis considered QALYs and reconvictions because these are the outcomes that decision makers in health care and criminal justice regularly base their decisions on (Fox & Albertson, 2011; NICE, 2012). Alternatively, singular outcome measures broader than QALYs, such as well-being or capabilities, or potential additional outcomes, such as productivity, could have been used. However, these outcomes may not reflect the decision makers need as they extend beyond their individual purviews.
The common practice of measuring the outcomes of health care interventions using QALYs offers the potential to compare programs in different areas of health care. However, QALYs are often criticized for their lack of sensitivity to capture small changes in specific diseases (Drummond et al., 2015). In public health, a further issue is that QALYs do not capture the broader set of non-health benefits generated by public health interventions (Marsh, Phillips, Fordham, Bertranou, & Hale, 2012; Squires, Chilcott, Akehurst, Burr, & Kelly, 2016; Weatherly et al., 2009), and may not include all the aspects that may matter to decision makers, especially when evaluating interventions with impacts on several dimensions (Brazier & Tsuchiya, 2015). However, this does not negate their value in allowing comparability, which can permit comparison of public health investments with investments in other health care programs. Furthermore, the proposed framework allows wider nonhealth outcomes of public health activities to be brought into consideration in a clear and transparent manner.
The proposed economic evaluation can provide better support for decision making by offering assessments of the benefits and opportunity costs for those dimensions which are considered most important by decision makers. Facts and value judgments required to combine multiple perspectives are made explicit. In the presence of winners and losers (i.e., some sectors benefit from the intervention while others bear the negative consequences), consideration can be given to whether compensation or transfers could create a scenario with only winners. Results of the economic evaluation can be used to suggest a resource allocation scheme based on adequate compensations among decision makers; if the sector that benefits from the intervention is able to compensate the loss in the other sector, then the intervention can be implemented and can generate an overall positive benefit (Claxton et al., 2007). Alternatively, decision making criteria based on dominance could be employed, where a new program is introduced only if all the components of the overall net impact (i.e., the net impacts for each sector) are positive. The framework can be thus used to show explicitly the missed investment opportunities (in terms of potential overall positive net impact not realized) due to due to political constraints and budgetary rigidities, and emphasize the importance of breaking down silos between decision makers' budgets.
A within-sector approach has been followed (Walker et al., 2019). Different results may have been obtained if the analysis would have considered a within individual approach that aggregated outcomes across sectors first. Such an approach could have potentially allowed for differences in individual preference over the relative importance of health versus other outcomes. In this analysis, only the criminal justice outcome was deemed relevant to the social decision maker in criminal justice, rather than an aggregate individual level measure which reflected both health and criminal justice, because health falls outside of their purview. Therefore, the within-sector approach appeared to be the more suitable for this analysis compared to the within-individual approach.
The aggregation was hence first additive across individuals within dimensions. The distribution of impacts across the population subgroups was not considered. The analysis was underpinned by the assumption that “a QALY is a QALY”, irrespectively of who is the beneficiary, and overlooked that health impacts of alcohol interventions fall on different groups of individuals which might raise equity concerns. Population-level health gain hence corresponded to the unweighted sum total of all individual health gains (Cookson et al., 2017; Drummond et al., 2015). However, alcohol interventions usually target groups on the edges of society (Bramley et al., 2015), benefit mostly groups with lower socio-economic status (Burton et al., 2017), and have wide impact across a range of issues related to (potentially unfair) health inequalities (Smith & Foster, 2014). Therefore, a distributional cost-effectiveness analysis (Asaria, Griffin, & Cookson, 2016; Asaria, Griffin, Cookson, Whyte, & Tappenden, 2015) could be included in the cross-sectoral analysis to incorporate health equity concerns in the evaluation.
As both health and criminal justice dimensions were associated with a positive net benefit, no aggregation across sectors was necessary and so none was performed. However, in principle the aggregation across sectors could be performed, but consideration would be required on the suitability of the assumption of non-overlapping outcomes to avoid issues of double counting (Sanders et al., 2016). For example, it might be argued that the consequences on victims' health were in fact indirectly included in the value associated with reducing crime. A potential cross-sectoral aggregation was investigated in an alternative cross-sectoral analysis. To ensure that potential double counting was avoided, the analysis did not consider the adjustment for the health impacts on victims of crime. Results are provided in Supporting Information 7. Results showed that the overall cost-effective intervention would still be BLC. However, it would be more problematic for decision makers to find a consensus on whether BLC should be introduced or not. Even though BLC would appear to be cost-effective from criminal justice perspective and from a joint health and criminal justice perspective, from the health care perspective it would result in a net loss of health and it would not be cost-effective.
A situation where an intervention appears to be cost-effective from an integrated perspective, but results in a negative net impact from a narrower perspective can lead to a conflict between the decision makers. For example, in this alternative scenario, the implementation of BLC would require the decision maker in the criminal justice system to renounce to a share of the benefits and compensate the negative impact of the intervention on health care. Nevertheless, the proposed cross-sectoral analysis can only show the potential cost-effectiveness of an intervention. To actually implement the intervention, the compensation across-sectors would need to be real (Remme, Martinez-Alvarez, & Vassall, 2017). In reality, such a compensation mechanism currently does not exist. Furthermore, if compensation schemes across sectors were created, incentives to prevent gaming of the system would be necessary (Remme, Vassall, Lutz, Luna, & Watts, 2014).
4.3 Limitations
This economic evaluation is based on a relatively small trial of a brief alcohol intervention, conducted over a short period of time. Treatments for alcohol use disorder have the potential to improve alcohol-related mortality and long-term morbidity (Barbosa, Godfrey, & Parrott, 2010; Hoang et al., 2016) and may produce long-term cost savings (Latimer, Guillaume, Goyder, Chilcott, & Payne, 2009). The short-term horizon of the trial may explain the non-statistically significant differences between arms. Further results of this economic evaluation are based on mean estimates and should be interpreted with caution. To assess the robustness of the results, sensitivity analyses reflecting the uncertainty about estimates should be conducted. Moreover, the reduction in criminal recidivism was found in the absence of significant differences in drinking consumption between the groups. Nevertheless, even in absence of differences in alcohol consumption across interventions, increased awareness might have resulted in a change in offending behavior rather than consumption per se, or offending might be linked to particular patterns of drinking rather than overall consumption (Newbury-Birch et al., 2014).
The CEA conducted from the ‘full’ health care perspective did not consider health consequences on individuals not directly involved in the crime, but still experiencing health consequences. Furthermore, broader impacts on victims' health, such as mental distress and fear of crime could be also included in the evaluation (Dolan & Peasgood, 2007). Therefore, the full impact on the health of victims of crime might have been underestimated. If these additional components were included in the analysis, the theoretical framework would still be valid, but the health spill-over effects generated in the criminal justice system would be higher. Moreover, the inter-sectoral marginal productivity of the criminal justice system in generating health would be affected.
The CEA conducted from the criminal justice system perspective was grounded on the assumption that a reduction in crime is not only associated with cost savings and positive health consequences, but has a value per se, due to higher safety perceived and less crime experienced. Therefore, when a treatment reduces crime rates, the economic evaluation should not only include the total reduction in criminal justice costs; it should consider also the increase in non-health outcomes, such as feeling safer and experiencing less crime (Neumann et al., 2018). Nevertheless, there are two limitations in the estimation of the valuation of a crime averted used in the analysis. First, contingent valuation estimates were taken from studies conducted in the United States (Cohen, 2015; Cohen et al., 2004) and might not reflect preferences of the UK population. However, selected studies appeared to provide the best estimate available in the literature of the intrinsic value of reducing crime per se (i.e., not including also consequences on victims' health). To our knowledge, no other attempts of revising these estimates have been conducted. Second, the estimated consumption value was referred to a reduction in criminal events. By contrast, the marginal productivity of the criminal justice system had to be estimated in terms of avoided reconvictions. This is because providers base their funding decisions on re-offending and recidivism (Fox & Albertson, 2011) and reconvictions are typically employed as a proxy to measure criminal activity (Griffith, Hiller, Knight, & Simpson, 1999; McCollister et al., 2003; Muser et al., 2015; Pearson, McDougall, Kanaan, Torgerson, & Bowles, 2016). Therefore, it was assumed that the reduction in criminal events corresponds to a reduction in reconvictions. However, the focus of this research was to illustrate how these estimates could be used in order to estimate the marginal productivity of the criminal justice system; if better evidence is provided, estimates can be adjusted accordingly.
4.4 Recommendations for further research
This applied cross-sectoral analysis was based on an actual intervention, and not a stylized or fictional example. The objective was to show what data was available and what further evidence may be needed for the assessment of a public health intervention with impacts on health and criminal justice. The highest priority for further research is to address the lack of marginal productivity estimates within and across public sectors other than health care. These estimates are necessary to assess the opportunity costs of the intervention (Hill et al., 2017; Sculpher et al., 2014). Reliable and valid instruments to measure cross-sectoral costs and benefits use are also pivotal to inform decision makers on how to optimally allocate scarce resources (Drost, Paulus, Ruwaard, & Evers, 2013; Neumann et al., 2018). Analysts should attempt to quantify in the impact inventory as many relevant costs and outcomes as possible within time and resources available, unless these are likely to have a negligible effect on the result of the analysis (Hill et al., 2017; Sanders et al., 2016). Because criminal justice service resource use is particularly important in the field of alcoholism (Mayer et al., 2017), it would be advisable for future trial-based economic evaluations of alcohol interventions to consider the routine adoption of resource-use measurement instruments to measure impacts falling on criminal justice system. Lists of resource-use measurement instruments in the criminal justice sector have been recently proposed (Drost et al., 2013; Mayer et al., 2017). Unit costs estimates for the criminal justice system are available for the United Kingdom (Brand & Price, 2000; Dubourg et al., 2005; Newton, May, Eames, & Ahmed, 2019).
5 CONCLUSIONS
This work illustrates how the cross-sectoral framework proposed by Walker et al. (2019) can inform heterogeneous stakeholders and guide decisions that require collaboration across sectors. The proposed analytical framework is capable of addressing key issues for the economic evaluation of public health interventions, such as considering a broader perspective and multiple-sectors. This case study aims to encourage other cross-sectoral economic evaluations to take transparent approaches, making explicit the assumptions and value judgments underpinning the analysis.
This applied cross-sectoral analysis investigates the impacts of a public health intervention on health and criminal justice. The lessons learned from this case study can be a useful reference for those interested in conducting economic evaluations of similar interventions in health care and criminal justice, or other non-alcohol related interventions with impacts on the same dimensions. For example, the same methods could be used to evaluate programs for the treatment of drug addiction (Byford et al., 2013), which impact on both health and criminal justice, through less crime attributable to drug use (Goranitis et al., 2017; Sculpher et al., 2014). Furthermore, this applied analysis and the lessons learned from it could be of use for the economic evaluation for other public health interventions with impacts on multiple sectors. For example, the approach used to estimate the threshold for the criminal justice sector could be used to facilitate the assessment of value for money in other sectors as well.
ACKNOWLEDGEMENTS
The authors acknowledge Dr. Laura Bojke (Center for Health Economics, University of York) for providing invaluable comments on previous versions of this manuscript. This work was funded and supported by the White Rose network and the Health Economics and Outcome Measurement theme of National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care, Yorkshire and Humber (CLAHRC YH) programme.
CONFLICT OF INTEREST
The authors have no conflicts of interest that are directly relevant to the content of this article.