Modelling the effect of market forces on the impact of introducing human immunodeficiency virus pre-exposure prophylaxis among female sex workers
Abstract
Pre-exposure prophylaxis (PrEP) to prevent human immunodeficiency virus (HIV) enables female sex workers (FSWs) to protect themselves from HIV without relying on clients using condoms. Yet, because PrEP reduces HIV risk, financial incentives to not use condoms may lead to risk compensation: reductions in condom use and/or increases in commercial sex, and may reduce the price of unprotected sex. In this analysis, we integrate market forces into a dynamic HIV transmission model to assess how risk compensation could change the impact of PrEP among FSWs and clients. We parameterise how sexual behavior may change with PrEP use among FSWs using stated preference data combined with economic theory. Our projections suggest the impact of PrEP is sensitive to risk compensatory behaviors driven by changes in the economics of sex work. Condom substitution could reduce the impact of PrEP on HIV incidence by 55%, while increases in the frequency of commercial sex to counter decreases in the price charged for unprotected sex among PrEP users could entirely mitigate the impact of PrEP. Accounting for competition between PrEP users and nonusers exacerbates this further. Alternative scenarios where increases in unprotected sex among PrEP users are balanced by decreases in non-PrEP users have the opposite effect, resulting in PrEP having much greater impact. Intervention studies need to determine how HIV prevention products may change the economics of sex work and provision of unprotected sex to enable a better understanding of their impact.
1 INTRODUCTION
Female sex workers (FSWs) face a multitude of health risks including high rates of sexually transmitted infections (STIs) and human immunodeficiency virus (HIV) (Bekker et al., 2015). Globally, FSWs are around 11 times more likely to be HIV infected than women in the general population (Baral et al., 2012), and are seen as a key population that require enhanced HIV testing, treatment, and prevention programs (Bekker et al., 2015). The economic context of sex work means that FSWs can face strong price competition from other FSWs, alongside client resistance to condom use, including threats and use of violence (Beattie et al., 2010, Deering et al., 2014, Pronyk et al.; Wojcicki & Malala, 2001). In many circumstances, FSWs are financially dependent on sex work to support themselves and their families (Beattie et al., 2012), which increases the potential influence of economic factors on sexual behaviors.
A large body of economic research on sex work has shown that higher prices are associated with the provision of riskier sex; anecdotal evidence of compensating differentials in sex work has existed for years (Wojcicki and Malala, 2001), but it was not until the early-2000s when Rao, Gupta, Lokshin, & Jana (2003) first empirically estimated a price premium of 79% for condomless sex among Indian FSWs, terming this the condom differential. Subsequent studies have estimated a condom differential of between 7% (Belgium and the Netherlands) and 81% (Bangladesh) among FSWs in different settings (Arunachalam and Shah, 2013; de la Torre, Havenner, Adams, & Ng, 2010; Gertler, Shah, & Bertozzi, 2005; Rao et al., 2003; Robinson and Yeh, 2011; Levitt and Venkatesh, 2007; Muravyev and Talavera, 2013). Similar patterns have been seen in data from male sex workers, although risks and market factors can differ substantively from FSWs, for example, there is a greater prevalence of non-penetrative sex among male sex workers and penetrative sex is riskier through receptive anal sex (Galarraga et al., 2014).
Recent technological developments have led to the development of antiretroviral-based HIV prevention products, for use as pre-exposure prophylaxis (PrEP) (AVAC, 2015). PrEP products currently exist in oral tablet and intravaginal ring form, and when used as prescribed can offer HIV protection for women (Fonner et al., 2016). Yet PrEP effectiveness—a function of product efficacy and adherence—varies across population groups and settings, with current products not offering any protection against STIs or pregnancy (ibid.). As such, condoms remain a crucial part of the HIV prevention armory, and clinical guidelines encourage PrEP users to use condoms consistently alongside antiretroviral-based products (Department of Health South Africa, 2016).
In a standard supply model, agents respond to technologies that reduce the risk of a utility-providing behavior by increasing levels of this behavior (Duncan & Holmlund, 1983). In other words, if PrEP reduces the risk associated with condomless sex, then FSWs may increase the quantity of condomless sex provided to increase the money earned per sex act. This response may result in the anticipated HIV-impact of PrEP being smaller than predicted, and may have other unintended consequences such as increasing STI transmission (Wilson, Xiong, & Mattson, 2014).
Risk compensation (also known as behavioral disinhibition) refers to an increase in risky behaviors (e.g., condomless sex) due to a preventive intervention (e.g., PrEP) reducing an individual's perception of risk. In recent years, developments in HIV prevention have been met with concerns that risk compensation may mitigate the impact of interventions (Cassell, Halperin, Shelton, & Stanton, 2006, Eaton and Kalichman, 2007), though it has been argued that the potential benefits of PrEP in reducing HIV incidence may outweigh the costs of reduced condom use (Blumenthal and Haubrich, 2014). However, if individuals overestimate the effectiveness of interventions, and because there are externalities associated with condomless sex (most notably HIV and STI transmission), risk compensatory behaviors may mean that PrEP has a reduced or even negative impact. This study explores this hypothesis.
In a previous study, a stated preference discrete choice experiment (DCE) was used to show that PrEP is likely to substantively impact the economics of sex work (Quaife et al., 2018c). DCEs are robust health economic tools, widely used to understand health-related behaviors by asking respondents to choose their preferred alternative from two choices over around 10 choice tasks (Clark, Determann, Petrou, Moro, & de Bekker-Grob, 2014). Studying how respondents choose across repeated scenarios allow us to quantitatively elicit the key drivers of decision-making. DCEs have been commonly applied in health to elicit preferences for products or services before they are introduced (de Bekker-Grob, Ryan, & Gerard, 2012), and have been shown to have reasonable predictive accuracy (Quaife, Terris-Prestholt, di Tanna, & Vickerman, 2018a). Specifically, in a previous study we found that condoms became less influential and price became more influential with PrEP use. Behavioral simulations from the DCE suggest that the condom differential would reduce with PrEP use from ZAR 467 (∼USD $32) to ZAR 179 (∼USD $12), whilst the amount of condomless sex supplied would increase by over two-fold.
Although useful, these DCE findings do not tell us how the impact of PrEP could be affected by these changes to the economics of sex work. Therefore, in this study we combine these results with existing theory from classical and behavioral microeconomics to explore how the impact of PrEP may be affected by changes in the economics of commercial sex. We use observational behavioral, epidemiological and stated preference data to parameterise a mathematical dynamic transmission model of HIV infection among FSWs and clients. We parameterise the transmission model to represent a high prevalence HIV epidemic among FSWs and their clients, based on South African data. To get an understanding of how the impact of PrEP use could be affected by economic effects, we take a stepwise approach including five scenarios, with each scenario incorporating additional assumptions around the economics of sex work.
Outside of FSW populations, there is evidence that PrEP use is associated with condomless sex and STI incidence (Holt et al., 2018; Lal et al., 2017; Ong et al., 2019; Traeger et al., 2018a). However, there have been very few studies that have assessed risk compensation outside of high-income country populations of men who have sex with men (MSM) (Quaife et al., 2019), whilst existing studies are not designed (i.e., there is rarely a reliable counterfactual) to examine if PrEP causes risk compensation. Although risk compensation does not seem to reduce the impact that PrEP can have on HIV incidence among MSM due to high levels of efficacy (Molina et al., 2017; Traeger et al., 2018b), this may not be the case in FSWs because women require higher adherence for PrEP to be efficacious (Wahl et al., 2017) and so usually experience lower efficacy.
Importantly for this study, there is little evidence of how PrEP use may affect the behavior of nonusers. For example, if nonusers feel safer due to widespread use of PrEP, this might lead to lower levels of condom use regardless of PrEP use. Alternatively, if demand for unprotected sex is fixed, an increase in provision of unprotected sex among PrEP users would reduce provision among non-PrEP-users. To-date, just one study has investigated this community-level risk compensation, finding a 35% reduction in condom use among MSM not using PrEP in Australia following the scale up of PrEP (Holt et al., 2018; Holt and Murphy, 2017). However, condom use data are generally self-reported and subject to acceptability biases (Prah et al., 2014; Lowndes et al., 2012; Treibich and Lepine, 2017); it is unclear how misreporting may affect the ability to observe the effects of PrEP on changing condom use.
This paper makes three contributions to the economic and epidemiological literatures on risk compensation in HIV prevention. First, this is the first study to explicitly integrate economic behaviors into a HIV transmission model. Specifically, we assume that the amount of supplied condom-protected and condomless sex is dependent on economic choices of act-price and income targeting using stated preference data. Second, we model community-level risk compensation for the first time, and account for competition between PrEP-using and non-using FSWs. In the absence of data, we assume that PrEP-using FSWs are willing to provide it at a lower price so causing the FSWs not using PrEP to adjust their willingness to accept risk to remain competitive. We extend this approach to consider what would happen if the increase in unprotected sex acts among PrEP users is balanced by decrease in non-PrEP users. Thirdly, this is the first study to explicitly model risk compensation among FSWs based on empirical (albeit stated preference) data.
Mathematical models are widely used to estimate the potential impact and cost-effectiveness of HIV treatment and prevention interventions among FSWs, including PrEP (e.g. Hallett et al., 2011; Mitchell et al., 2015; Shannon et al., 2015; Vassall et al., 2014). However, to-date only a handful of models have explicitly accounted for individual-level condom substitution or other forms of risk compensation, and in these the magnitude of condom substitution due to PrEP has not been based on empirical data. Foss, Vickerman, Heise, Watts, (2003) and Grant et al. (2017) predicted that condom substitution could occur without increasing HIV risk among FSWs with lower levels of condom use, or if the effectiveness of PrEP was higher than currently estimated (>75%). Mitchell et al. (2016) found that a 50% reduction in condom use by PrEP users would negate the beneficial impact of PrEP among FSWs. Among MSM in the UK, Punyacharoensin et al. (2016) estimated that PrEP effectiveness would be significantly reduced if the amount of condomless sex or number of sexual partners increased by 50%.
2 METHODS
We developed and parameterized a dynamic HIV transmission model using a system of ordinary differential equations to model HIV transmission among FSWs and their male clients to match the characteristics of a generic HIV epidemic in South Africa. The model is described in Section 2.1 and parameterized in Section 2.2. This model is used to consider the impact of PrEP being introduced among FSWs, considering five scenarios that account for how market factors of increasing complexity may affect the economics of commercial sex and so the behavior of FSWs during commercial sex (Section 2.3 onwards). We further explore the impact of PrEP if the additional unprotected acts provided by non-PrEP users are instead provided by PrEP users.
Scenario S1.: Base case PrEP use, no condom substitution.
S1 makes the same assumption as most current mathematical models, assuming no risk compensation due to PrEP use, that is, no change in the quantity or type of protected or condomless sex supplied.
Scenario S2.: Condom substitution among PrEP users.
S2 uses simulations from our DCE to predict the degree of condom substitution (28-percentage point reduction in condom use, from 78% to 50%) that would occur among PrEP users, holding all other sexual behaviors and condom use in non-PrEP users constant.
Scenario S3.: Target income assumption—adjusting quantity supplied.
S3 uses the DCE predictions to estimate that PrEP users will accept a (73%) lower price for providing condomless sex compared to nonusers. We then use the target income hypothesis to assume that FSWs on PrEP will increase their frequency of commercial sex to keep their income constant.
Scenario S4.: A competitive market—Non-PrEP users either change the amount of sex supplied., and
Scenario S5.: Change the amount of sex and levels of condom use.
S4 and S5 explore the effects of community-level risk compensation by taking a whole-market perspective to acknowledge that the behavior of FSWs not using PrEP may be affected by the behavior of PrEP users, depending on the extent of PrEP coverage, due to competition in supply for a limited client base.
2.1 HIV transmission model
The model stratifies the FSW and client population into HIV negative FSWs on or off PrEP and HIV negative clients, and HIV positive clients and FSWs in the acute, chronic, or AIDS state of infection either on or off antiretroviral therapy (ART). New clients and FSWs enter the model at a rate to balance natural mortality (from all compartments) and cessation of commercial sex by FSWs and clients. In addition, individuals leave the modeled population due to AIDS-related mortality from the AIDS compartments. ART initiation is assumed to occur in the chronic and AIDS stages of HIV infection, with ART users having a lower rate of disease progression. ART dropout is modeled, with re-initiation assumed to occur at the same rate as for ART-naive individuals.
Clients and FSWs enter the HIV negative or chronic compartments according to estimates of HIV prevalence in the general population (Simbayi et al., 2018). When someone becomes infected with HIV, they enter the acute stage of infection for around three months; during which they are more infectious than individuals with chronic infection. After the acute stage of infection, FSWs and clients enter the chronic stage where they remain until they begin ART or progress to AIDS. Individuals with AIDS are more infectious than people with chronic infection.
FSWs and clients form commercial sex partnerships, through which HIV transmission occurs. The risk of HIV transmission per act (i.e., the force of infection) depends on the per sex act probability of HIV transmission from a HIV positive client to a FSW, or vice versa; the number of commercial sex acts that clients and FSWs have; the likelihood that a condom is used in a given act; and the likelihood that a given partner is HIV positive, which is a weighted average of the number of the potentially HIV positive partners they could have who are on ART (and therefore less infectious), chronically infected or have acute or AIDS infection (and therefore more infectious). PrEP is only available to FSWs, not male clients, with FSWs being recruited on to using PrEP at a specified rate, and ceasing to use PrEP at a constant rate. FSWs who stop using PrEP can start using PrEP again at the same uptake rate as other FSWs. PrEP use decreases the per-sex act probability of HIV transmission for any FSW using PrEP.
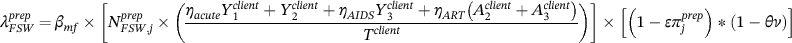
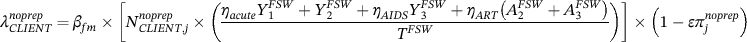
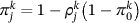
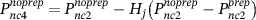
 refers to the total number of acts for FSWs using PrEP, which is different for each scenario j. The parameter
refers to the total number of acts for FSWs using PrEP, which is different for each scenario j. The parameter  denotes condom use, which also varies by scenario j, and
denotes condom use, which also varies by scenario j, and  denotes condom efficacy. We define
denotes condom efficacy. We define  as the overall effectiveness of PrEP at an adherence level of ν,
as the overall effectiveness of PrEP at an adherence level of ν,  the per act transmission probability from a HIV positive male to a HIV negative female and vice versa for
the per act transmission probability from a HIV positive male to a HIV negative female and vice versa for  . The force of infection for FSWs using PrEP
. The force of infection for FSWs using PrEP  and FSW or clients not using PrEP
and FSW or clients not using PrEP 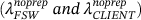 in scenario j are given in Equations (7-9), where Tclient and TFSW represent the total number of clients and FSWs,
in scenario j are given in Equations (7-9), where Tclient and TFSW represent the total number of clients and FSWs,  , and
, and  represent the heightened transmissibility of HIV positive persons in acute and AIDS stages, respectively, while
represent the heightened transmissibility of HIV positive persons in acute and AIDS stages, respectively, while  is the reduced transmissibility attributable to ART use. A schematic of the model structure and the system of differential equations for the model are given in Supplementary Data S1. Compartments X refer to HIV negative persons, Yi HIV positive but not on ART, and Ai HIV positive and on ART, where the subscript i denotes the stage of HIV infection (i = 1 refers to acute infection, i = 2 refers to chronic infection and i = 3 refers to AIDS; i can only take values 2 and 3 for those on ART Ai).
is the reduced transmissibility attributable to ART use. A schematic of the model structure and the system of differential equations for the model are given in Supplementary Data S1. Compartments X refer to HIV negative persons, Yi HIV positive but not on ART, and Ai HIV positive and on ART, where the subscript i denotes the stage of HIV infection (i = 1 refers to acute infection, i = 2 refers to chronic infection and i = 3 refers to AIDS; i can only take values 2 and 3 for those on ART Ai).
 (10)
(10) (11)
(11) (12)
(12)2.2 Baseline model parameterization and calibration
The model was parameterized using data from South Africa, where the size of the FSW population was assumed to be 132,000 as estimated for South Africa in 2013 (South African National AIDS Council, 2013). Most FSW behaviors in the model were parameterized using a DCE survey that was undertaken in 2015, which recruited 203 FSWs through respondent driven sampling (Quaife et al., 2018b), 122 of whom self-reported as HIV negative. The DCE sample was demographically comparable to a cohort of HIV negative FSWs who were enrolled into the TAPS PrEP demonstration project in Johannesburg 2015/6 which recruited FSWs exhaustively from Johannesburg (Eakle et al., 2017). Although not all demographic characteristics were measured in comparable ways, similarities were present in those that were, including mean age (DCE 29.5, TAPS 29.8 years); the proportion in a steady relationship (DCE 63%, TAPS 53%); and the proportion who entertained in a hotel or brothel (DCE 80%, TAPS 77%).
Data on the client population size are uncertain, and so we estimated it by balancing the number of commercial sex acts reported by clients and FSWs, which suggested the client population size was between seven and eight times greater than the FSW population. FSWs were assumed to cease sex work at a rate of 14% per year  which gives an average duration of sex work of seven years, the third quartile of the self-reported time in sex work in a 2015 cross-sectional survey of FSWs in South Africa (Quaife et al., 2017a). We assume that clients cease buying sex at a rate of 10% per year
which gives an average duration of sex work of seven years, the third quartile of the self-reported time in sex work in a 2015 cross-sectional survey of FSWs in South Africa (Quaife et al., 2017a). We assume that clients cease buying sex at a rate of 10% per year  , implying that they buy sex for on average 10 years.
, implying that they buy sex for on average 10 years.
Self-reported estimates of condom use from face-to-face surveys can be higher than reality due to acceptability bias (Treibich and Lepine, 2017). The DCE survey in South Africa (Quaife et al., 2018b) asked FSWs a number of questions on condom use during commercial sex (see supplementary Data S2), producing estimates ranging between 60% and 96%. However, this is likely to be biased, with a study of FSWs from Senegal finding estimates for condom use to be 97% when using standard face-to-face survey methods, reducing to 78% when a list randomization method was used to reduce reporting biases (Treibich and Lepine, 2017). Clients also report lower levels of condom use than FSWs, while polling booth surveys of FSWs find lower levels of condom use than face-to-face surveys (Lowndes et al., 2012; Prah et al., 2014; Treibich and Lepine, 2017). In the DCE dataset, the proportion of FSWs who did not report any condomless acts was 78%, and so we used this as our central estimate for the consistency of condom use. For the simplest PrEP scenario modeled (S1), we assume this remains unchanged among both PrEP users and non-PrEP users, that is, there is no condom substitution. In later scenarios (S2 to S5), we model the impact of condom substitution.
The DCE survey also estimated that FSWs engaged in a mean of 33 commercial sex acts per month (Quaife et al., 2018b), which is within the interquartile range of estimates from other FSW surveys in South Africa (Richter, Luchters, Ndlovu, Temmerman, & Chersich, 2012). The number of commercial sex acts per client was assumed two per month. Biological parameters and the efficacy of condoms and ART in preventing HIV transmission were obtained from published literature (Hughes et al., 2012). Multiplicative cofactors for the probability of HIV transmission during the AIDS and acute stages of HIV came from meta-analyses (Boily et al., 2009). The effectiveness of ART in reducing HIV transmission was assumed to be 92% (Cohen et al., 2011, Donnell et al., 2010). Details of the model parameters are included in Table 1.
| Parameter | Symbol | Value | Source |
|---|---|---|---|
| FSW population size | TFSW | 132,000 | (South African National AIDS Council, 2013) |
| Client population size | TClient | 1,000,000 | Estimated through balancing the number of commercial sex acts reported by FSWs and clients |
| PrEP uptake rate |  |
15% | (Quaife et al., 2017a) |
| PrEP dropout rate |  |
20% | Assumed, based on (Eakle et al., 2017) |
| PrEP efficacy | θ | 71% | (Baeten et al., 2012) |
| PrEP adherence |  |
75% | Assumed, based on (Eakle et al., 2017) reporting 70%–85% in South African FSWs |
| Baseline condom use |  |
78% | Taken from (Quaife et al., 2017a). See Table S1. |
| Condom efficacy |  |
80% | (Hughes et al., 2012) |
| Condom use after substitution | 50% | DCE analyses suggests condomless sex increases 2.3-fold from 22% to 50% | |
| ART initiation rate |  |
11% | Calibrated to fit to 2019 coverage. |
| ART dropout rate |  |
4% | (Fox et al., 2012) |
| Relative rate of progression to AIDS due to ART treatment |  |
0.33 | (Johansson, Robberstad, & Norheim, 2010) |
| Natural death rate (FSWs and clients) |  |
0.016 | 1/life expectancy of 62.4 years (STATS SA, 2011) |
| Exit rate from sex work |  |
7% | Assumption from duration (Quaife et al., 2017a) |
| Exit rate from being a client |  |
10% | Assumption |
| Duration of acute HIV stage (years) |  |
0.242 | (Hollingsworth, Anderson, & Fraser, 2008) |
| Duration of chronic stage (years) |  |
10.05 | (Hollingsworth et al., 2008) |
| Duration of AIDS stage (years) |  |
0.83 | (Hollingsworth et al., 2008) |
| Multiplicative transmission factor in the acute stage |  |
11.65 | (Boily et al., 2009) |
| Multiplicative transmission factor in the AIDS stage |  |
8.15 | (Boily et al., 2009) |
| Multiplicative transmission factor due to treatment |  |
0.08 | (Cohen et al., 2011; Donnell et al., 2010) |
| Female to male per act transmission probability |  |
0.0055 | (Centers for Disease Control, 2015), varied in model fitting from 0.008 to 0.0022 |
| Male to female per act transmission probability |  |
0.8  |
Varied to fit epidemic from 0.5 to 2 |
| Initial FSW HIV prevalence | 60% | Multiple sites in South Africa (UCSF, 2015). | |
| Initial client HIV prevalence | 9.6% | South Africa (Simbayi et al., 2018), twice that of males aged 20–24 | |
| HIV prevalence among men entering client pool | 4.8% | South Africa (Simbayi et al., 2018), males aged 20–24 | |
| HIV prevalence among women entering sex work | 21.55% | South Africa (Simbayi et al., 2018), assuming average age of starting sex work of 25 (Quaife et al., 2017a), midpoint in prevalence between females aged 20–24 and 25–29 | |
| Monthly clients seen by FSW | 33 | (Quaife et al., 2017a) | |
| Monthly FSWs seen by clients | 2 | Median from survey of FSWs and clients in Port Elizabeth (unpublished) | |
| Price of condom protected sex act (ZAR) | 72 | (Quaife et al., 2017a) | |
| Price of condomless sex act (no PrEP) (ZAR) | 467 | (Quaife et al., 2017a) | |
| Competition coefficient | Ω | 0.5 | Assumption |
- Abbreviations: ART, antiretroviral therapy; FSW, female sex worker; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis; STI, sexually transmitted infection.
Using parameter values in Table 1 (except PrEP related parameters), the model was calibrated to the HIV prevalence and ART coverage of FSWs in South Africa. An HIV prevalence of 60% was firstly seeded into the FSW population in 2004 with no ART, 13 years before the assumed introduction of PrEP. To fit the model we varied the per sex act probability of male to female HIV transmission  , and the ratio of this to female to male transmission to give a modeled epidemic with a stable HIV prevalence of around 55% among FSWs and 14% among clients over 2004 to 2017 (see Figure S1:1). There are few robust estimates of HIV prevalence among FSWs, and none published for clients, however the central prevalence estimate from a three city study of FSWs in South Africa found a HIV prevalence of 54% in 2013/14 (UCSF, 2015). This gave a calibrated HIV prevalence in clients of between 13 and 15%. With these fitted values for the transmission probabilities, the model was then rerun to calibrate the ART coverage among FSWs and clients to the observed scale-up of ART in South Africa from zero coverage in 2004 to around 54% coverage among general population women and 44% among men in 2017, as shown in supplementary Data S1.
, and the ratio of this to female to male transmission to give a modeled epidemic with a stable HIV prevalence of around 55% among FSWs and 14% among clients over 2004 to 2017 (see Figure S1:1). There are few robust estimates of HIV prevalence among FSWs, and none published for clients, however the central prevalence estimate from a three city study of FSWs in South Africa found a HIV prevalence of 54% in 2013/14 (UCSF, 2015). This gave a calibrated HIV prevalence in clients of between 13 and 15%. With these fitted values for the transmission probabilities, the model was then rerun to calibrate the ART coverage among FSWs and clients to the observed scale-up of ART in South Africa from zero coverage in 2004 to around 54% coverage among general population women and 44% among men in 2017, as shown in supplementary Data S1.
2.3 Incorporating economics into a transmission model
 (1)
(1) represents the total income from sex work,
represents the total income from sex work,  and
and  are the number of condomless and condom protected sex acts supplied, respectively, and
are the number of condomless and condom protected sex acts supplied, respectively, and  and
and  are the price paid for condomless and condom protected sex acts, respectively. We divide FSWs into those that use PrEP (k = prep) or do not use PrEP (k = noprep) for each scenario of how PrEP effects condom use and frequency of commercial sex (j = 0, 1, 2, 3, 4, 5), where j = 0 refers to the baseline scenario where PrEP has not been introduced.
are the price paid for condomless and condom protected sex acts, respectively. We divide FSWs into those that use PrEP (k = prep) or do not use PrEP (k = noprep) for each scenario of how PrEP effects condom use and frequency of commercial sex (j = 0, 1, 2, 3, 4, 5), where j = 0 refers to the baseline scenario where PrEP has not been introduced. and
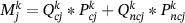
and  . However, the important parameters for an HIV transmission model are not the price but the quantity and relative supply mix of protected and condomless sex acts in the market, so we integrate the economic and modelling frameworks as follows. If we assume the level of condom use for PrEP users (k = prep) and nonusers (k = noprep) is
. However, the important parameters for an HIV transmission model are not the price but the quantity and relative supply mix of protected and condomless sex acts in the market, so we integrate the economic and modelling frameworks as follows. If we assume the level of condom use for PrEP users (k = prep) and nonusers (k = noprep) is  for each scenario of how PrEP use effects condom use (j = 1,…,5), then the number of protected and condomless sex acts can be defined as follows:
for each scenario of how PrEP use effects condom use (j = 1,…,5), then the number of protected and condomless sex acts can be defined as follows:
 (2)
(2) (3)
(3) is the number of sex acts for PrEP users and nonusers in each scenario. Substituting (2) and (3) into (1) and factorizing give the following expression for the total income of FSW:
is the number of sex acts for PrEP users and nonusers in each scenario. Substituting (2) and (3) into (1) and factorizing give the following expression for the total income of FSW:
 (4)
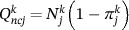
(4) , is either unaffected or related to that of PrEP users. Parameter
, is either unaffected or related to that of PrEP users. Parameter  denotes the relative change in condomless sex acts for each PrEP scenario j compared to the baseline scenario without PrEP (j = 0), which is used to adjust how baseline condom use,
denotes the relative change in condomless sex acts for each PrEP scenario j compared to the baseline scenario without PrEP (j = 0), which is used to adjust how baseline condom use,  , is affected in each scenario.
, is affected in each scenario.
 (5)
(5)2.4 Predicting price changes under PrEP use
The DCE study (Quaife et al., 2018b) estimated that without PrEP, the mean reported (revealed preference) price of condom protected  and condomless sex
and condomless sex  was ZAR 72 (USD $5.41) and ZAR 467 (USD $35), respectively, implying a large condom differential of ZAR 395 (549%). However, the DCE also projected that fully effective PrEP would reduce this condom differential by 73%. Therefore, when using PrEP we assume that this premium is reduced by 73% (ZAR 395 × 0.27 = ZAR 107), and so the price of condomless sex
was ZAR 72 (USD $5.41) and ZAR 467 (USD $35), respectively, implying a large condom differential of ZAR 395 (549%). However, the DCE also projected that fully effective PrEP would reduce this condom differential by 73%. Therefore, when using PrEP we assume that this premium is reduced by 73% (ZAR 395 × 0.27 = ZAR 107), and so the price of condomless sex  is ZAR 72 + 107 = ZAR 179.
is ZAR 72 + 107 = ZAR 179.
2.5 PrEP impact analyses
Previous studies have sought to predict demand for PrEP among FSW, giving a 15% annual uptake of PrEP (Quaife et al., 2017). Assuming PrEP is introduced in 2017, and a 20% annual PrEP dropout rate based on lower bounds from a South African FSW demonstration project (Eakle et al., 2017), this results in a 28% coverage of PrEP among HIV-negative FSW after 5 years and 34% coverage after 20 years of PrEP use (2037). We assumed the efficacy of PrEP if highly adherent was 71%, the highest estimated among female groups in PrEP trials to-date (Baeten et al., 2012), and assumed a baseline adherence (ν) of 75%. The impact of PrEP is quantified by our model as the relative change in new HIV infections over 20 years (prevented fraction) following the rollout of PrEP compared to a counterfactual scenario of no rollout. We model the impact of PrEP for the five following scenarios of how PrEP use could affect the dynamics of commercial sex. Table 2 shows how the economic parameters vary across these scenarios.
| Scenario 0 Baseline or counterfactual | Scenario 1 PrEP with no behavior change | Scenario 2 Condom substitution among PrEP users | Scenario 3 Target income assumption—PrEP users increase the quantity supplied | Scenario 4 Competition—Non-PrEP users increase the amount of sex supplied | Scenario 5 Competition—Non-PrEP users change the amount and type of sex supplied | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PrEP users | Non-PrEP users | PrEP users | Non-PrEP users | PrEP users | Non-PrEP users | PrEP users | Non-PrEP users | PrEP users | Non-PrEP users | PrEP users | Non-PrEP users | |
| Condom use | N/A | 78% | 78% | 78% | 49% | 78% | 49% | 78% | 49% | 78%a | 49% | 78%a |
| Number of commercial sex acts per month | N/A | 33 | 33 | 33 | 33 | 33 | 42 | 33 | 42 | 33 | 42 | 32–33 a |
| Price of condomless act | N/A | 467 | 467 | 467 | 179 | 467 | 179 | 467 | 179 | Mean: 464 a | 179 | Mean: 464 |
| Range: 459–467 | Range: 459–467 | |||||||||||
| Price of protected act | N/A | 72 | 72 | 72 | 72 | 72 | 72 | 72 | 72 | 72 | 72 | 72 |
| Monthly income from sex work (ZAR) | N/A | 5243 | 3152 | 5243 | 4131 | 5243 | 5243 | 5243 | 5243 | 5243 | 5243 | 5243 |
- Abbreviation: PrEP, pre-exposure prophylaxis.
- a Dependent on H = Ω*PrEP coverage. Parameters in bold signify changes in each scenario as compared to the previous, moving from left to right. ZAR 5243 = USD $355, ZAR 4131 = USD $280, ZAR 3152 = USD $214.
2.5.1 Scenario 1: Base case PrEP use, no condom substitution
Scenario 1 is the current approach used in many PrEP impact models that assume no change in sexual behaviors due to PrEP and do not account for potential economic influences on behavior.
2.5.2 Scenario 2: Condom substitution among PrEP users
The DCE predicted that among PrEP users, the condom differential will fall by 73% to ZAR 179 (∼USD $12) per condomless sex act and the quantity of condomless sex will increase 2.3-fold. Substituting ρjk = 2.3 into Equation (5) suggests that among PrEP users, condom use  will decrease from 78% to 49%.
will decrease from 78% to 49%.
In this scenario, we assume that PrEP use only affects the condom use of FSWs using PrEP and hold the level of condom use for non-PrEP users constant at 78% (i.e., assuming that there is no competition between FSWs). We also assume no change in the total number of sex acts provided, that PrEP use has no effect on the price charged for sex with a condom, and that prices do not change among non-PrEP users. This means that FSWs using PrEP will bear an 11% income reduction of ZAR 555 (USD $42) per month, whereas FSWs not using PrEP will see no reduction in income.
2.5.3 Scenario 3: Target income assumption—adjusting quantity supplied
This scenario extends scenario 2 by incorporating evidence from behavioral microeconomics, the target income hypothesis which suggests that when suppliers are faced with an exogenous shock to wages, they adjust their quantity of labor supplied to keep income constant. The target income hypothesis, popularized in the seminal study by Camerer, Babcock, Loewenstein, & Thaler (1997), demonstrated that taxi drivers in New York City make supply decisions with a reference-dependent income target, ceasing working when it is reached and working fewer hours when wages are higher. Similar results, indicative of a backward-bending supply curve, have been found in studies among Singaporean taxi drivers (Chou, 2002) baseball stadium vendors (Oettinger, 1999), and Swiss bicycle messengers (Fehr and Goette, 2007).
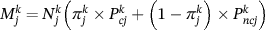
 . However, we assume that PrEP users increase their overall frequency of commercial sex to ensure the same income. We therefore want to find the new frequency of sex
. However, we assume that PrEP users increase their overall frequency of commercial sex to ensure the same income. We therefore want to find the new frequency of sex  which gives the same income, which we obtain through rearranging Equation (4):
which gives the same income, which we obtain through rearranging Equation (4):
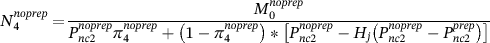
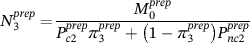 (6)
(6) is 49% of acts, as in scenario 2, but set monthly income as fixed to the same level as before the introduction of PrEP (
is 49% of acts, as in scenario 2, but set monthly income as fixed to the same level as before the introduction of PrEP ( = ZAR 5160 or USD $387), meaning FSWs on PrEP need to provide 27% more commercial sex acts, increasing from 396 to 502 per year. As before, we assume that FSWs using PrEP have no effect on the level of condom use of non-PrEP users and do not affect the price they can charge for condomless sex.
= ZAR 5160 or USD $387), meaning FSWs on PrEP need to provide 27% more commercial sex acts, increasing from 396 to 502 per year. As before, we assume that FSWs using PrEP have no effect on the level of condom use of non-PrEP users and do not affect the price they can charge for condomless sex.2.5.4 Scenario 4: A competitive market—Non-PrEP users change the amount of sex supplied but not levels of condom use
The previous scenarios assume that only FSWs using PrEP respond to changing market conditions caused by the introduction of PrEP. A more realistic assumption would be that the dynamics of the commercial sex market would shift to some extent for all FSWs, not just those using PrEP, as they are working in a competitive market. For example, non-PrEP users would also face pressures to charge lower prices for condomless sex and potentially increase their supply of condomless sex as a result.
We model the impact of such competition in scenarios 4 and 5. Scenario 4 assumes that non-PrEP users face pressure to reduce the price of condomless sex due to the reduction in price by PrEP users. However, we assume that this will be related to the uptake of PrEP; when PrEP uptake is low, non-PrEP users will only see a small effect of competition, whereas if PrEP use is higher, then nonusers are more likely to feel the effect of competition.
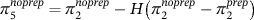
We account for this by using a parameter to mediate the extent to which non-PrEP users face the same change in condom differential as PrEP users. This factor 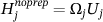 describes the extent to which overall PrEP coverage Uj (among all FSWs) affects price among non-PrEP users according to a competition coefficient,
describes the extent to which overall PrEP coverage Uj (among all FSWs) affects price among non-PrEP users according to a competition coefficient,  bounded by [0,1]. For example, if PrEP coverage is 20% and
bounded by [0,1]. For example, if PrEP coverage is 20% and  is set to 1, then the price of condomless sex among non-PrEP users would be 20% closer to what it is among PrEP users compared to before PrEP. If
is set to 1, then the price of condomless sex among non-PrEP users would be 20% closer to what it is among PrEP users compared to before PrEP. If  is reduced to 0.5, then the impact of competition would be halved to 10%. In the base case,
is reduced to 0.5, then the impact of competition would be halved to 10%. In the base case,  is set to 0.5 with variation explored in the sensitivity analyses.
is set to 0.5 with variation explored in the sensitivity analyses.
 = 0.49), but they will increase their total number of commercial sex acts to maintain their current income, while assuming a lower price for condomless sex (but the same for protected sex). To calculate the new price of condomless sex among non-PrEP users, we relate the price of condomless sex among non-PrEP users to the reduced price among PrEP users (
= 0.49), but they will increase their total number of commercial sex acts to maintain their current income, while assuming a lower price for condomless sex (but the same for protected sex). To calculate the new price of condomless sex among non-PrEP users, we relate the price of condomless sex among non-PrEP users to the reduced price among PrEP users ( as estimated by the DCE and applied in scenario 2) and the baseline price before PrEP was introduced
as estimated by the DCE and applied in scenario 2) and the baseline price before PrEP was introduced  also estimated in the DCE) by using the factor Hj:
also estimated in the DCE) by using the factor Hj:
 (7)
(7) (8)
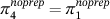
(8)2.5.5 Scenario 5: A competitive market—Non-PrEP users change the amount of sex supplied and levels of condom use
 changes) according to the behaviors of PrEP users. We assume that they also increase their frequency of condomless sex acts based on the same competition coefficient that we hypothesized would affect the price of condomless sex. Extending (5) we assume that:
changes) according to the behaviors of PrEP users. We assume that they also increase their frequency of condomless sex acts based on the same competition coefficient that we hypothesized would affect the price of condomless sex. Extending (5) we assume that:
 (9)
(9) = 0.78 and
= 0.78 and  = 0.49 as given by the DCE. We then substitute
= 0.49 as given by the DCE. We then substitute  from Equation (9) into the equivalent of Equation (8) to give the adjusted number of sex acts for non-PrEP users as follows:
from Equation (9) into the equivalent of Equation (8) to give the adjusted number of sex acts for non-PrEP users as follows:
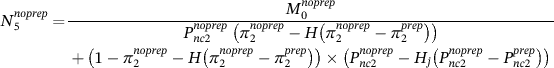 (10)
(10)2.6 Substitution effects assuming constant demand for unprotected sex
We extend the above scenarios to acknowledge that PrEP and non-PrEP users may instead differentially adjust their share of the unprotected sex market. Specifically, we assume that the demand for unprotected sex remains constant and therefore risk compensation among PrEP users results in them capturing a greater share of the unprotected sex market. We adapt scenarios S2, S3, and S4 to assume that unprotected acts among non-PrEP users reduce by the same amount as they increase among PrEP users due to risk compensation. This assumes that demand—defined as the total number of unprotected acts demanded per client—remains constant despite a lower price for unprotected sex among PrEP users, allowing us to explore an alternative hypothesis for how condomless sex could change with PrEP use. We keep all other behavioral and price assumptions the same, including the constant income assumption for PrEP users in Scenario S3, and the influence of reductions in the price of condomless sex among PrEP user on the price charged for condomless sex among non-PrEP-users in S4.
2.7 Sensitivity analyses
We undertook univariate sensitivity analyses on base case scenarios to assess how uncertainty or variation in important parameters may affect the percentage of infections prevented by PrEP over 20 years for all scenarios, and present those for scenarios 1, 3 and 5 in the main text. We varied assumptions relating to the prevention products (PrEP efficacy, uptake, and retention, and condom use and efficacy), parameters for the frequency and type of sex supplied, and parameters that determine how the economics of sex work affect these (condom differential, competition coefficient, condom substitution). A full list of parameters varied, and their range is provided in supplementary Data S3 in Table S3:1.
3 RESULTS
3.1 Baseline prevalence and incidence trends
In Figure 1, the model predicted a relatively stable HIV epidemic for a scenario without PrEP, with prevalence declining slowly due to ART up to 2037. Supplementary Data S1 shows model outputs with and without ART. The 2037 HIV prevalence in FSW was predicted to be 73% without ART and 53% with ART. Client HIV prevalence increased to a stable prevalence of around 22% without ART, reducing to 13% with ART.
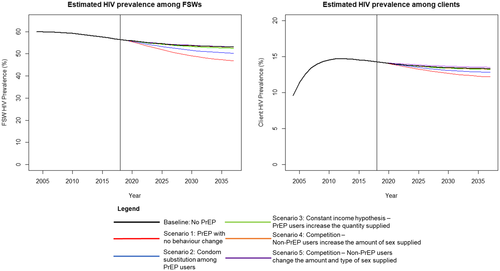
Impact of PrEP use on HIV prevalence among FSWs and their clients for different scenarios of how PrEP use affects frequency of commercial sex acts and levels of condom use. Vertical line in each figure signifies when PrEP intervention is initiated. Vertical axes differ; Abbreviations: FSW, female sex worker; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis
3.2 PrEP impact projections
If we assume condom use remains constant among PrEP users (Scenario S1), then our model projects that introducing PrEP in 2017 to reach 35% coverage by 2037 could prevent 3.9% of new HIV infections among FSWs and clients over the 20 years following introducing PrEP (Figure 2). Alternatively, if PrEP users increase the frequency of condomless sex 2.27-fold (but do not increase the number of acts supplied—Scenario S2), the model suggests that the proportion of infections prevented by PrEP would reduce by 55%, resulting in 1.7% of new HIV infections being prevented over 20 years compared to if PrEP had not been introduced (Figure 2). If PrEP users also increase their frequency of commercial sex to maintain the same income (Scenario S3), we now project that introducing PrEP only prevents a marginal proportion of the number of HIV infections over 20 years (0.4%), with prevalence and incidence only decreasing very slightly by 2037 compared to the no PrEP scenario in 2037.

Percentage of HIV infections averted by PrEP among FSWs and clients over 20 years of PrEP use (from 2017) for different scenarios of how PrEP use affects frequency of commercial sex acts and levels of condom use; Abbreviations: FSW, female sex worker; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis
If the price for condomless sex also decreases among non-PrEP users and they increase their frequency of commercial sex to maintain the same income (Scenario S4), then the impact of PrEP decreases further, only resulting in 0.2% of HIV infections being prevented over 20 years. If non-PrEP users also reduce their level of condom use as well as frequency of commercial sex (Scenario S5) then the introduction of PrEP now causes a small increase in HIV transmission, increasing the number of HIV infections by 0.7% compared to if PrEP had not been introduced.
Lastly, we find that the model is highly sensitive to how the number and distribution of unprotected acts changes across PrEP users and nonusers, reinforcing the finding that behavioral changes are highly influential to the impact of PrEP. For instance, if the number of unprotected sex acts in the market remains constant, then an increase in unprotected acts among PrEP users due to risk compensation reduces the number provided by non-PrEP users. Figure 3 shows that this would make PrEP more effective, averting 6.3% of HIV infections over the 20 years following the introduction of PrEP. This is an increase in infections averted of 253% compared to Scenario S2 without this substitution of unprotected acts to PrEP users, or an increase of 54% compared to Scenario S1. With unprotected acts held constant, HIV prevalence and incidence in Scenario S2 would decrease by 15% and 36%, respectively, compared to no PrEP by 2037.
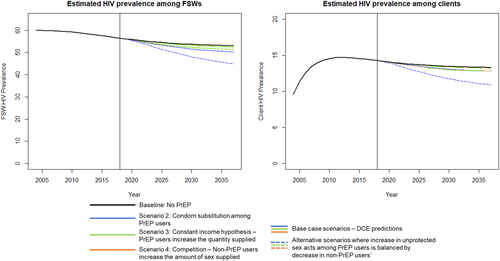
Impact of PrEP use on HIV prevalence among FSWs and their clients for different scenarios of how PrEP use affects frequency of commercial sex acts and levels of condom use. Figure compares baseline scenarios (solid lines) with alternative scenarios (dashed lines) where any increase in condomless sex among PrEP users is balanced by a decrease among non-PrEP users. Vertical line in each figure signifies when PrEP intervention is initiated. Vertical axes differ; Abbreviations: DCE, discrete choice experiment; FSW, female sex worker; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis
The same pattern is observed to a lesser extent when the same substitution of condomless acts from non-PrEP users to PrEP users is assumed in Scenarios S3 (1.5% of infections averted, 208% reduction in infections compared to base case S4) and S4 (1.3% of infections averted, 303% reduction in infections compared to base case S4). Although these scenarios make the strong assumption that the demand for unprotected sex will not increase as the average market price falls, they demonstrate the importance of understanding behavior and market changes which could occur due to the introduction of PrEP.
3.3 Sensitivity analyses
Figure 4 shows one-way sensitivity analyses for baseline scenarios 1, 3 and 5 with the remaining scenarios shown in Data S3. The sensitivity analyses suggest that for all modeled scenarios the impact of PrEP is highly sensitive to assumptions of PrEP efficacy, with more impact being achieved with higher PrEP efficacy. If PrEP has high efficacy (91%), then it almost offsets the detrimental effects of condom migration and the other economic effects included in Scenario S5, with PrEP now preventing 1.7% of HIV infections over 20 years, just under half of what was achieved in Scenario S1 without behavior change. This analysis also demonstrates the impact of different adherence assumptions through considering the effect of different levels of PrEP efficacy on PrEP impact, as PrEP efficacy is related to levels of adherence. Surprisingly, increasing PrEP coverage only has a similar beneficial impact in Scenario S1, with its effect being smaller in the scenarios with risk compensation and other market effects. The condom use assumptions also have a large effect on the impact of PrEP, with increases in condom use, its efficacy, and the level of condom migration all resulting in a large decrease in the impact of PrEP in all scenarios.
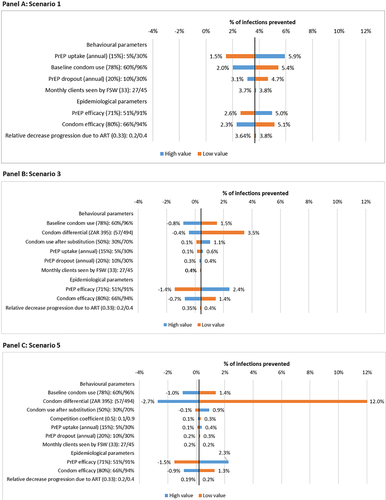
One-way sensitivity analyses showing how the percentage of infections prevented by PrEP for Scenarios S1 (panel A), S4 (panel B) and S5 (panel C) varies under different parameter assumptions. Vertical black line in each figure denotes the baseline impact of PrEP for that scenario; Abbreviations: ART, antiretroviral therapy; FSW, female sex worker; PrEP, pre-exposure prophylaxis
Outside of the condom differential, results are less sensitive to variation in parameters related to the economics of sex work. For example, variations in the competition coefficient  has greatest effect on the results in Scenario S5 (where it affects non-PrEP users' behavior), but still only induces around a third of the variation that results from varying the efficacy of PrEP or condoms.
has greatest effect on the results in Scenario S5 (where it affects non-PrEP users' behavior), but still only induces around a third of the variation that results from varying the efficacy of PrEP or condoms.
4 DISCUSSION
This study investigated if behavior changes in sex work due to market forces arising from the introduction of new prevention products such as PrEP could affect the impact of these products. Results suggest that the impact of PrEP could be highly sensitive to risk compensatory behaviors driven by changes in economic incentives and the prices charged for condomless sex during commercial sex. In addition, externalities of risk compensation among PrEP users could also be important for affecting the impact of PrEP if they also influence the behavior of non-PrEP users, for example through market competition. We find that the impact of PrEP is highly sensitive to relatively small changes in condom use among non-PrEP users as well as changes in the distribution of unprotected acts across PrEP users and nonusers resulting from risk compensation. On one hand, if the demand for unprotected sex is stable and risk compensation leads to PrEP users providing more unprotected acts, then risk compensation results in a higher PrEP impact than if there was no risk compensation. Conversely, if PrEP results in an increase in unprotected and protected sex due to reductions in its price then PrEP may result in little change in HIV transmission.
The model was manually parameterized for the South African setting, and results are unlikely to perfectly predict the impact of PrEP nor behavioral responses to its introduction. However, results are striking in the magnitude and implications of their predictions; specifically, that the impact of PrEP may be negated by simple risk compensation whereby PrEP users are willing to engage in more condomless sex at a lower price, and so may engage in more sex to counteract any loss in earnings. Our analyses show that when the condom differential, and the effect of PrEP use on this premium, is large, the benefits of PrEP are reduced because then there is a large incentive for PrEP users to increase their frequency of condom-protected and condomless sex to maintain the same level of income. Additionally, these economic effects are also likely to be most important in situations where there is a low efficacy of PrEP and/or high consistency of condom use because then any changes in sexual behaviors will rapidly offset the added protection provided by PrEP. Furthermore, when externalities of risk compensation are considered such that behaviors of non-PrEP users are influenced by those of PrEP users, this study suggests that introducing PrEP may actually result in an increase in HIV transmission.
To-date, no studies have considered the effect of PrEP—or other preventative interventions—on the economics of sex work. One study found a condom differential remained after a multifaceted HIV prevention program, but was unable to attribute changes to the program (Quaife et al., 2020). A broad range of data are collected during trials and demonstration projects of HIV prevention products such as PrEP, which offers the opportunity to gather revealed preference data on the extent of risk compensatory behaviors and changes to the condom differential. However, these studies do not generally collect data from FSWs who are not using PrEP and are often dependent on self-reported condom use data which is frequently biased. At an individual level, biomedical prevention programmes need to consider the specific commercial environment in which male and FSWs operate. Further research is needed to assess the real-world impact of interventions on the economics of sex work and how that then affects the behavior of all FSWs, including, but not limited to, the extent that financial incentives for risky behaviors are modified by interventions. The results of this analysis demonstrate the importance of monitoring changes in risk behaviors and the price paid for protected and condomless sex among PrEP and non-PrEP users. In particular, future work should focus on using novel methods for getting less biased estimates for the level of condom use and the condom differential, to ensure that real changes are not masked by reporting biases.
We do not have sufficient information to reliably parameterise changes in the demand side of the market, although we do explore one feasible scenario where total demand for unprotected sex is constant. All scenarios assume perfect substitution among suppliers where changes in individual supply do not affect demand.
Although this study seeks to improve on the majority of mathematical models by accounting for behavior change after the introduction of an intervention, this requires a number of assumptions which may not hold in reality. Firstly, risk compensatory behaviors among FSWs are predicted through the analysis of stated preference DCE data which may suffer from hypothetical bias. Although systematic review evidence suggests that the predictive ability of DCEs is reasonable in health choices (Quaife et al., 2018a), they are thought to over-predict desired behavior changes, and underestimate undesirable behavior (Salampessy et al., 2015; Ryan and Watson, 2009). In this study, we are not able to assess the direction of potential biases which could feasibly under- or overstate FSW responsiveness to price changes.
Secondly, we impose a restrictive model of the market for commercial sex. Demand is assumed to be homogenous. Although PrEP use is likely to be unobserved by clients, FSW revelation of use could signal her HIV negative status alongside a willingness to protect her health. This signal that an act may be safer could increase a client's willingness to pay for condomless sex, increasing incentives in the provision of condomless sex. Furthemorer, FSWs may also exhibit risk compensatory behavior if they are HIV positive and on HIV treatment; a recent study in Senegal found that condom use among persons using ART was appreciably lower than that among HIV negative or HIV positive persons not on treatment (Treibich and Lepine, 2017). Fortunately, the high level of protection provided by ART should mitigate the detrimental effect of this on HIV transmission. A potential limitation of our model is that we assume that no behavior change occurs upon HIV acquisition, treatment initiation or due to disease progression. In addition, we do not explicitly model the role of anal sex in price negotiation nor in the transmission model. This is because the self-reported frequency of anal sex among FSWs in the 2015 sample was extremely low (0.3%), whilst the DCE suggested preferences for anal sex would not change under PrEP use. This omission should not have affected our projections. However, because receptive anal sex has a much greater per-act HIV transmission risk compared to receptive vaginal sex, the negative epidemiological impact of reduced condom use in anal sex acts could have a large effect in other settings with a greater frequency of anal sex.
In addition, if client preferences are augmented by actual or perceived FSW PrEP use, the market may become segmented such that clients prefer to purchase sex from PrEP users, and do not operate in a single market as modeled here. This clustering of risk would reduce the impact of externalities among non-PrEP users, and mean we underestimate the impact of PrEP in scenarios 4 and 5. However, the extent to which FSWs might want to, or could, reliably signal PrEP use to clients is unclear. Indeed, whilst there is evidence of partner sorting by serostatus and biomedical prevention product use among MSM, this has been shown to be an ineffective means of prevention, and can even increase HIV risk in areas with low HIV testing rates (Wilson, Regan, Heymer, Jin, Prestage, & Grulich, 2010). No evidence of serosorting exists among FSWs and clients.
Scenarios 3, 4 and 5 use the target income hypothesis to justify the assumption that FSWs set a weekly income target. This assumption is different to a classic dynamic model of labor supply which predicts that people will work less when wages fall, due to a lower opportunity cost of leisure time, or earning wages from different occupations (Lucas and Rapping, 1969). Using this model would reduce the negative implications for PrEP impact as less risk compensation would occur. Although multiple studies have found evidence of behavior consistent with the target income hypothesis (Camerer et al., 1997; Chou, 2002; Morgul and Ozbay, 2015; Oettinger, 1999), some studies have demonstrated behaviors consistent with the classic model of labor supply (Stafford, 2011). Because 85% of the 2015 DCE sample relied exclusively on sex work for their income, we argue suggesting that other sources of work are not available for many in this population and therefore the target income hypothesis is a better characterization of potential behavior change.
We do not use economic theory when modelling changes in entry to and exit from sex work. Instead we make a standard assumption that ensures a stable population size, other than due to HIV-related mortality. However, if wages fall after the introduction of PrEP, the financial benefits of initiating sex work may be reduced. In this instance, we would expect the number of new entrants to sex work to reduce, or the number of leavers to increase, potentially intensifying demand for services from FSW who remain.
Individuals other than FSWs and clients are not included in the model to make it tractable and to focus on the main implications of changes in the sex work market. However, this may mean we underestimate the impact of PrEP by not accounting for onward transmission to other population groups. Furthermore, we do not consider the potential for drug resistance to emerge because of poor adherence to PrEP. While this was primarily to keep the model tractable in running the stylized behavioral scenarios, evidence suggests that the chance of HIV drug resistance developing due to PrEP use is very low, and in the few cases observed has probably occurred when PrEP is used during undiagnosed acute HIV infection (Gibas, Van Den Berg, Powell, & Krakower, 2019). In addition, because adherence does not vary across the behavioral scenarios modeled, it is unlikely that resistance would have a major impact on the main findings of this study.
Lastly, the model only considers changes to HIV transmission and does not consider the effect of prevention choices on other STIs or unintended pregnancies. New HIV prevention products are single-purpose, only preventing HIV transmission, yet condoms are multipurpose conferring protection from unintended pregnancy and other STIs. Substitution from condoms to a single-purpose product may result in additional health losses, which we did not account for here, highlighting that our projections are likely to be conservative in only considering one harm of reducing condom use. In addition, DCE data have shown that other attributes of HIV prevention products may be more attractive to some FSWs than HIV prevention, including additional protection from unintended pregnancy or STIs (Quaife et al., 2017); introducing products incorporating these characteristics would likely increase overall impact.
5 CONCLUSION
This study raises the question of how new prevention interventions may affect the economics of sex work and so have unintended consequences. It shows how the impact of a new HIV prevention product, PrEP, is highly sensitive to assumptions around the economics of commercial sex. This is the first study to explicitly incorporate economic factors into a dynamic HIV transmission model. Through using stated preference data and behavioral economic theory, we model the possible effect that risk compensation among FSWs may have on the impact of PrEP in reducing HIV infection. We find that existing models may substantially overestimate the impact of PrEP among FSWs if they do not account for how PrEP could increase the frequency of condomless sex while reducing its price, so potentially leading to increases in the frequency of commercial sex. Alternatively, if increases in unprotected sex among PrEP users are balanced by decreases among non-PrEP users then the opposite effect may occur, resulting in PrEP having greater impact.
This study explores a number of hypotheses which merit further investigation, ideally with high-quality observational data collected among both PrEP users and nonusers. In particular, results suggest that economic factors might mitigate the impact of PrEP interventions depending on how the frequency of unprotected sex is affected by PrEP use, yet act-level data on price or other determinants of behavior are rarely collected in PrEP demonstration or implementation projects. Few data are also collected among FSW groups who are not engaged with clinical trials or demonstration projects, yet longitudinal data on economic factors will be crucial for fully exploring their effect on HIV prevention interventions.
ACKNOWLEDGMENTS
This work was funded in part by an ESRC PhD Studentship. PV is also funded by the National Institute of Health Research funded Health Protection Research Unit in Evaluation of Interventions.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.