The Failure Rate of Internal Fixation Increases With Sagittal Displacement of the Femoral Head: A Retrospective Study
Lei Shi and Chen Chen contributed equally to this study.
ABSTRACT
Background
The risk of internal fixation failure remains relatively high in stable femoral neck fracture (FNF) (Garden I or II). Preoperative sagittal displacement of the femoral head has been proposed as a potential influencing factor. This study aimed to evaluate the impact of sagittal displacement on the outcomes of cannulated screw internal fixation (CSIF) in patients with stable FNF (Garden I or II) by reconstructing the axial sagittal oblique plane of the fracture using preoperative computed tomography (CT) imaging.
Methods
This study included 167 patients with FNF who underwent CSIF. The sagittal tilt angle of the femoral head (STAFH) was evaluated using three-dimensional CT (3D-CT). The distribution of preoperative STAFH was analyzed, and its independent association with treatment failure was assessed. Treatment failure was defined as the need for revision surgery within 2 years postoperatively due to avascular necrosis, nonunion, or internal fixation failure.
Results
Among the 167 patients, 9 (5.4%) exhibited anterior tilt (AT) of the femoral head, 158 (94.60%) presented with posterior tilt (PT). A total of 50 patients (29.9%) demonstrated excessive sagittal displacement (AT ≥ 10° or PT ≥ 20°). In the failure group, 80.0% of patients had excessive sagittal displacement compared to 28.1% in the healed group. Excessive sagittal displacement was significantly associated with an increased risk of surgical failure (odds ratio: 11.953, 95% CI: 3.656–39.083, p < 0.05).
Conclusions
In patients with Garden I or II FNF, greater preoperative sagittal displacement of the femoral head was correlated with a higher likelihood of CSIF failure. AT ≥ 10° or PT ≥ 20° were identified as independent predictors of CSIF failure in FNF patients. Nevertheless, these findings still require confirmation through prospective, multi-center clinical trials with large sample sizes.
Abbreviations
-
- 3D-CT
-
- three-dimensional computed tomography
-
- ASA
-
- American Society of Anesthesiologists
-
- AT
-
- anterior tilt
-
- BMI
-
- body mass index
-
- CI
-
- confidence interval
-
- CSIF
-
- cannulated screw internal fixation
-
- FNF
-
- femoral neck fracture
-
- GAI
-
- Garden Alignment Index
-
- MCL
-
- mid-collum line
-
- OR
-
- odds ratio
-
- PT
-
- posterior tilt
-
- RCL
-
- radius collum line
-
- STAFH
-
- sagittal tilt angle of the femoral head
1 Introduction
Femoral neck fracture (FNF) are common injuries among middle-aged and elderly individuals, accounting for 3.58% of all fractures [1] and 54% of hip fractures [2, 3]. Owing to the anatomical and biomechanical properties of the femoral neck, these fractures frequently lead to severe complications, such as osteonecrosis of the femoral head, nonunion, or internal fixation failure, which eventually result in surgical failure and contribute to notable disability and mortality rates. Postoperative complications following FNF have been reported in up to 40%–43% of cases [4-6]. As the global population ages, the incidence of FNF continues to rise, posing an increasing public health challenge. The Garden classification is widely utilized for categorizing FNF [6, 7], primarily based on anteroposterior X-ray imaging of the hip joint. Garden Types I and II fractures are generally deemed stable [8]. However, despite being classified as “stable,” many of FNF (Garden Types I and II) still experience internal fixation failure, necessitating revision surgery or conversion to arthroplasty. Reported failure rates for internal fixation in stable FNF range from 8% to 56% [7, 9], raising concerns regarding the reliability of the Garden classification as the sole criterion for treatment selection.
The current Garden classification has certain limitations, particularly its inability to accurately evaluate sagittal displacement of the femoral head, especially the extent of anterior-posterior tilt caused by fracture impact. Some scholars have suggested using lateral X-ray films to assess sagittal displacement, as studies indicate that sagittal displacement may significantly influence surgical outcomes in FNF [9-11]. In a retrospective analysis, Palm et al. [12] identified a “PT ≥ 20°” as an important predictor of failure in FNF treated with cannulated screw fixation. Sjöholm et al. [13] even proposed a threshold classification, defining “PT ≥ 20°” and “anterior tilt (AT) ≥ 10°” as significant parameters associated with fixation failure. However, other study has suggested that larger sagittal displacements of the femoral head do not necessarily increase the risk of internal fixation failure [14]. These discrepancies may arise from differences in displacement angle measurement methods, variations in outcome parameters, implant selection, and heterogeneity among study populations.
Currently, there is inconsistency in the measurement parameters for hip joint frog or lateral X-ray imaging across different hospitals. Patients with fracture pain often have difficulty in cooperating with positioning, which makes it challenging for orthopedic surgeons to obtain standard X-ray images. Compared to X-ray imaging, 3D-CT has higher precision in capturing subtle fracture changes. 3D-CT scans have lower requirements for the position of the affected limb, effectively reducing examination errors caused by patients' painful forced positions. Through three-dimensional reconstruction technology, ideal reconstruction planes can be easily obtained, enabling precise angle measurement.
This study was conducted to assess the association between STAFH, assessed via 3D-CT reconstruction, and the failure rate of internal fixation, using three cannulated screws in patients with FNF. In this single-center, large-sample retrospective study, we sought to ascertain whether STAFH is an independent predictor of internal fixation failure, thereby providing insights for clinical decision-making.
2 Materials and Methods
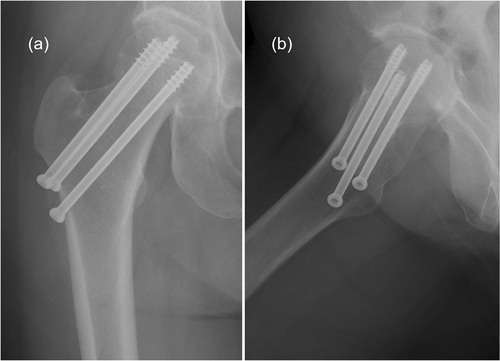
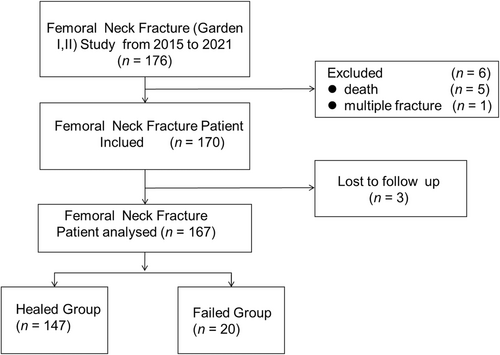
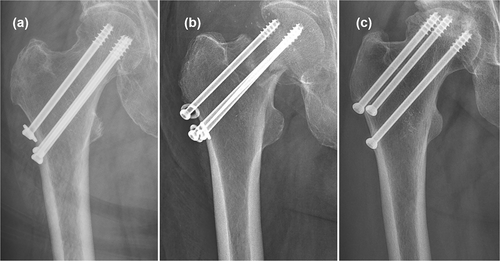
This retrospective cohort study analyzed data from 167 patients with acute FNF who underwent internal fixation with three cannulated screws at the Department of Orthopedics, Chinese PLA General Hospital, China, between January 2015 and December 2021 (Figure 1). The patient selection flowchart is shown in Figure 2. Demographic and clinical parameters were collected, including age, sex, body mass index (BMI), history of smoking and alcohol consumption, and diabetes status. Additionally, perioperative indicators such as the American Society of Anesthesiologists (ASA) classification, fracture type, STAFH, and Garden Alignment Index (GAI) were recorded. Postoperative outcomes were assessed, including fracture healing, nonunion, femoral head necrosis, internal fixation failure (Figure 3), and Harris hip score (HHS). In patients with surgical failure, the treatment failure time when internal fixation failed was documented. Definitions of outcomes: Internal fixation failure was defined as screw breakage, loosening, or cut-out occurring within 24 months postoperatively. Fracture nonunion was defined as the absence of fracture healing within 24 months post-surgery. Femoral head necrosis was diagnosed based on Steinberg grade ≥ 2 [8] characterized by cystic and sclerotic changes on imaging. Motor function recovery was evaluated using the HHS [15], which ranges from 1 to 100. HHS scores were categorized as excellent (≥ 80 points) or poor (< 80 points). The ASA classification was used to assess patients' preoperative physical status: Grade I: healthy individuals with normal organ function; Grade II: patients with mild systemic disease; Grade III: patients with severe systemic disease but retaining functional independence; Grade IV: patients with severe systemic disease and significant disability affecting daily activities; Grade V: moribund patients with a life expectancy of less than 24 h, with or without surgery; Grade VI: patients declared brain death, with organs preserved for transplantation. The treatment failure time point was the date when radiographic evidence of surgical failure was first identified during follow-up examinations. The duration between the initial surgery and this failure detection was subsequently calculated as the “survival time.”
2.1 Criteria for Including Patients
Patients were eligible for inclusion if they met the following criteria: (1) Aged ≥ 60 years with acute FNF resulting from low-energy trauma. (2) Availability of complete imaging data, including preoperative anteroposterior radiographs, preoperative 3D-CT images, and postoperative anteroposterior and lateral radiographs of the affected hip. (3) FNF classified as Type I or II. (4) Underwent CSIF as the treatment modality. (5) Patients and their families expressed willingness and demonstrated the ability to comply with treatment and follow-up protocols.
2.2 Exclusion Criteria
Patients were excluded if they met any of the following conditions: (1) Presence of pathological FNF on the affected side. (2) FNF resulting from high-energy trauma. (3) History of hip surgery on the affected side. (4) Pre-existing osteonecrosis of the femoral head. (5) FNF accompanied by vascular or nerve injuries. (6) Chronic or pre-existing FNF. (7) Presence of mental disorders or severe consciousness disturbances that could affect treatment adherence. (8) Patients whose families refused or were unable to cooperate with treatment and follow-up.
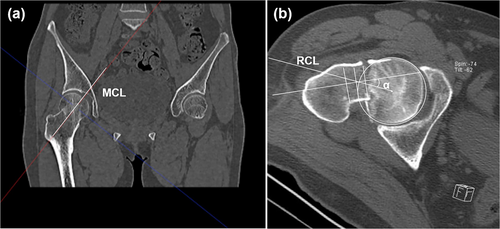
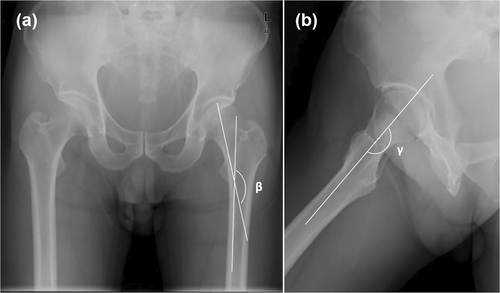
2.3 Imaging Examination and Measurement
All X-ray and CT scans were conducted by experienced radiographers. Two trauma orthopedic surgeons independently assessed the Garden classification of fractures and the STAFH. In cases of disagreement regarding the Garden classification, a third senior orthopedic surgeon provided the final diagnosis. The STAFH was measured five times by two trauma orthopedic surgeons, and the average value was calculated to ensure accuracy. Image analysis was performed using hospital imaging software. The STAFH measurement method followed the approach recommended by Tiee et al. [16], which involved reconstructing the axial sagittal oblique plane on the CT images (Figure 4a). The STAFH was then assessed using the method described by Palm et al. [12]: the mid-collum line (MCL) was marked along the femoral neck; a circle centered at the midpoint of the femoral head was drawn; the radius collum line (RCL) was extended from the center of the circle, intersecting both the MCL and the circumference of the circle; and the STAFH was defined as the angle α between the MCL and RCL (Figure 4b). Following the recommendations of Sjöholm et al. [13], STAFH was categorized into two risk levels: low risk: 0° ≤ PT < 20° or 0° ≤ AT < 10°; high risk: PT ≥ 20° or AT ≥ 10°. Fracture reduction quality was assessed via the Garden alignment index (GAI). As shown in Figure 5, this assessment involved measuring the angle β, formed between the shaft margin (Figure 5a) and the pressure trabecula of the femoral head, and the angle γ, defined by the axis of the femoral head and neck (Figure 5b). Reduction quality classification: Good reduction (GAI: I or II) was defined as 155° ≤ β ≤ 160° and γ = 180°, whereas poor reduction (GAI: III or IV) was defined as β < 155° or γ > 180°. To assess measurement reliability, the intraclass correlation coefficient (ICC) was calculated based on the imaging measurements independently performed by the two trauma orthopedic surgeons.
2.4 Surgical Procedure
Patients underwent continuous epidural anesthesia and were placed in the supine position on an orthopedic lower limb traction bed. A C-arm X-ray machine was placed between the thighs to obtain anteroposterior and lateral radiographic images of the femoral neck. Fracture reduction was achieved by precisely adjusting the magnitude and direction of traction, combined with adduction and pronation of the affected limb. The reduction quality was confirmed through fluoroscopic assessment using the C-arm X-ray machine. Once satisfactory reduction was achieved, standard skin disinfection and aseptic procedures were performed.
A longitudinal incision (approximately 3–5 cm) was made on the lateral aspect of the proximal femur, aligned with the lesser trochanter. Blunt dissection was carried out through the subdermal tissue and deep fascia to expose the inferior margin of the lesser trochanter. Under C-arm fluoroscopic guidance, three 2.5-mm guide pins were inserted from the lower border of the lesser trochanter, advancing along the femoral neck axis. The appropriate direction and length of the guide pins were verified using fluoroscopy. Subsequently, three cannulated screws were introduced along the guide pins, forming an inverted triangular configuration within the femoral neck for optimal stability. If closed reduction was unsuccessful, open reduction was performed. The anterior Smith‒Peterson approach was utilized, providing direct exposure of the anterior joint capsule. A T-shaped capsulotomy was performed to allow direct visualization of the fracture site, facilitating precise reduction. The internal fixation procedure for open reduction followed the same technique as that for closed reduction.
On postoperative Day 1, patients initiated isometric quadriceps exercises on the affected side and engaged in active or passive flexion-extension training of the ipsilateral hip joint. Precautions were taken to avoid compression, excessive external rotation, and adduction of the affected limb during rehabilitation. Postoperative antithrombotic prophylaxis was achieved through subcutaneous administration of enoxaparin sodium at a standardized dosage of 2000 AXaIU once daily for a duration of 1 month.
2.5 Postoperative Follow-Up Program
Patients underwent scheduled follow-ups at 6 weeks, 3 months, 6 months, 1 year, and 2 years postoperatively, with annual outpatient follow-ups thereafter. Each follow-up visit included a clinical assessment and imaging evaluation, with the HHS used to assess functional recovery of the affected hip joint. Radiographic assessment was performed using anteroposterior and lateral X-rays of the hip joint to monitor fracture healing and detect potential osteonecrosis of the femoral head. In cases where osteonecrosis was suspected, MRI was recommended for further evaluation. As osteonecrosis of the femoral head typically develops within 2 years post-surgery, follow-up was conducted for more than 2 years [17, 18].
2.6 Statistical Analysis
All statistical analyses were conducted using SPSS 21.0 software (IBM, Armonk, New York, USA). Continuous variables were expressed as the means ± standard deviations. The Shapiro‒Wilk test was employed to evaluate the normality of data distribution, whereas the Bartlett test was used to evaluate homogeneity of variance. For normally distributed data, comparisons were performed using independent sample t-tests, whereas non-normally distributed data were analyzed using the Mann‒Whitney U test. Categorical variables were presented as frequencies (percentages, %) and compared using the χ2 test or Fisher's exact test, depending on the distribution. p < 0.05 was considered statistically significant.
The relationships between surgical failure and various factors, including age, sex, comorbidities, BMI classification, femoral head tilt angle, quality of fracture reduction, and final HHS grade, were analyzed via independent sample t-tests, χ2 tests, or Fisher exact tests, as appropriate. Patients were stratified based on the STAFH, and a univariate logistic regression model was employed to examine the correlation between the STAFH categories and surgical failure.
| Healed FNF (n = 147) | Failed FNF treatment (n = 20) | p | |
|---|---|---|---|
| Age (years) | 66.06 ± 4.56 | 65.45 ± 3.67 | 0.567 |
| Female | 75 (51) | 9 (45) | 0.613 |
| Garden alignment index (III and IV) | 136 (93) | 16 (80) | 0.066 |
| BMI (kg/m2) | 24.74 ± 2.06 | 23.20 ± 2.79 | 0.218 |
| Harris Hip Joint Function Scale (< 80) | 38 (25.9) | 20 (100.0) | < 0.001 |
| Smoking | 17 (11.6) | 2 (10.0) | 0.596 |
| Alcohol | 10 (6.8) | 2 (10.0) | 0.435 |
| Diabetes | 18 (12.2) | 2 (10.0) | 0.560 |
| Length of stay (days) | 4.88 ± 3.23 | 4.45 ± 2.37 | 0.563 |
| Sagittal tilt angle of femoral head | 14.64° ± 7.64° | 25.10° ± 7.41° | < 0.001 |
- Note: We defined the Garden alignment index (III and IV) as poor reduction quality. Data are presented as mean ± SD and n(%).
- Abbreviations: ASA, American Society of Anesthesiologists; BMI, body mass index; FNF, femoral neck fracture; SD, standard deviation.
| Group | OR | p | 95% confidence interval |
|---|---|---|---|
| 10° ≤ PT < 15° | 0.799 | 0.683 | 0.272–2.345 |
| 15° ≤ PT < 20° | 0.594 | 0.391 | 0.181–1.951 |
| 20° ≤ PT < 25° | 1.151 | 0.364 | 0.649–3.241 |
| 25° ≤ PT | 1.129 | 0.409 | 0.846–1.508 |
- Abbreviations: AT, anterior tilt; OR, odds ratio; PT, posterior tilt.
According to the classification of the risk of the STAFH by Sjöholm et al. [13], all patients were divided into a low-risk group and a high-risk group. Multivariate logistic regression was used to identify potential confounding factors influencing the association between femoral head tilt angle and surgical failure. p < 0.05 was considered significant difference.
| Healed FNF (n = 147) | Failed FNF treatment (n = 20) | p | |
|---|---|---|---|
| Low risk | 113 (76.9) | 4 (20) | |
| High risk | 34 (23.1) | 16 (80) | |
| Crude odds ratio | Reference | 13.294 (95% CI: 4.164–42.441) | < 0.05 |
| Adjusted odds ratio | Reference | 11.953 (95% CI: 3.656–39.083) | < 0.05 |
- Note: Low risk: 0° ≤ PT < 20° or 0° ≤ AT < 10°; hight risk: PT ≥ 20° or AT ≥ 10°.
- Adjusted factors: BMI, age, and GAI.
- Abbreviations: BMI, body mass index; FNF, femoral neck fracture; GAI, Garden alignment index.
3 Results
The patient enrollment process for the 176 cases of FNF (Garden I/II) is depicted in Figure 2. Two experienced trauma orthopedic surgeons independently classified all cases, reaching diagnostic agreement in 150 patients, while discrepancies arose in 23 cases. These discrepancies were resolved by a senior trauma surgeon. A total of three patients were lost to follow-up, one patient with a Garden II fracture was excluded because of multiple fractures, and five patients died from causes unrelated to surgery. Ultimately, 167 patients with Garden I or II FNF were included in the final analysis.
The mean age of the cohort was 66.01 ± 4.56 years (range: 60–84 years), comprising 83 males (49.7%) and 84 females (50.3%). The mean BMI was 23.39 ± 2.75 kg/m2 (range: 16.77–32.05 kg/m2). A history of smoking was reported in 19 patients (11.38%), and 12 patients (7.19%) had a history of alcohol consumption. The ASA classification distribution was as follows: Grade I (14 patients, 8.38%), Grade II (140 patients, 83.83%), Grade III (12 patients, 7.19%), and Grade IV (1 patient, 0.60%). Reduction quality, as assessed by the GAI, indicated good fracture reduction in 152 cases (91.02%) and poor reduction quality in 15 cases (8.98%). At the final follow-up, the mean HHS was 83.19 ± 5.74, with 109 patients (65.27%) classified as having excellent hip function, while 58 patients (34.73%) had poor outcomes. The STAFH measurements demonstrated high interobserver agreement between the two trauma orthopedic surgeons (ICC = 0.97, 95% CI: 0.96–0.98). Of the 167 patients, 9 had femoral head anteversion (mean: 6.74° ± 4.16°), while 158 had femoral head retroversion (mean: 16.58° ± 7.61°). According to Sjöholm's risk classification [13], 117 cases (70.06%) were classified as low risk, while 50 cases (29.94%) were considered high risk.
Treatment failure occurred in 20 of the 167 patients (11.98%), with femoral head necrosis being the most common cause (13 patients, 7.78%), predominantly diagnosed via X-ray imaging. Nonunion was observed in four patients (2.4%), while internal fixation failure occurred in three patients (1.80%). Among the 15 patients who experienced surgical failure, revision surgery was successfully performed.
A comparison of demographic characteristics between the surgical success and failure groups is shown in Table 1. Significant differences were observed in BMI (p = 0.218), the STAFH (p < 0.01), and the HHS at the last follow-up (p < 0.001). The failure group had a significantly higher BMI (24.74 ± 2.06) kg/m2 than the success group (23.20 ± 2.79) kg/m2, indicating a potential association between overweight/obesity and surgical failure. The failure group exhibited a significantly higher STAFH (25.10° ± 7.41°) compared to the success group (14.64° ± 7.64°). None of the patients (0%) in the failure group achieved excellent or good HHS, compared to 74.1% in the success group, highlighting a significant decline in hip function due to postoperative complications. No statistically significant association between the survival time and the degree of femoral head sagittal tilt was found (Supporting Information S1: Tables 1 and 2). Although some previous studies have suggested a relationship between fracture reduction quality and treatment failure, our findings did not identify a statistically significant association (p = 0.086). However, we retained reduction quality as a confounding factor in multivariate analysis.
Given the limited number of cases with AT > 0° and PT < 10°, patients with PT ≥ 10° were stratified into groups based on 5° increments in STAFH. As indicated in Table 2, no significant differences were observed between patients who achieved fracture healing and those who experienced surgical failure across these STAFH groups. According to Sjoholm's risk classification [13], the proportion of high-risk STAFH cases in the failure group (80.0%) was significantly higher than in the success group (28.1%), with an odds ratio (OR) of 13.294 (95% CI: 4.164–42.441, p < 0.05). After adjusting for BMI, age, and reduction quality in a multivariate logistic regression model, the adjusted OR was 11.953 (95% CI: 3.656–39.083) (Table 3).
4 Discussion
This study aimed to identify potential factors contributing to the failure of internal fixation surgery in patients with stable FNF (Garden Types I and II). Additionally, it established a correlation between the preoperative STAFH, as determined on reconstructed CT images, and the risk of treatment failure following CSIF in patients with Garden Types I and II FNF. The reoperation rate for patients with stable FNF (Garden I or II) after internal fixation is reported to range between 8% and 21% in certain trauma centers [19], with some studies suggesting rates as high as 56% [7]. Consequently, the reliability of the Garden classification as a guiding tool for FNF treatment has been widely questioned. In 1992, Alho et al. proposed a potential association between posterior femoral head displacement in the sagittal plane and internal fixation failure, although their findings were based on a limited sample of 13 cases [20]. Subsequently, Conn and Parker conducted a retrospective analysis of 375 cases of FNF without displacement, demonstrating that an increased femoral head posterior tilt was associated with a higher risk of fracture nonunion following internal fixation [21]. More recently, in 2013, Clement et al. analyzed 162 patients with stable FNF, and reported that an excessive PT angle was associated with an increased risk of fixation failure and postoperative mortality [22].
Recent research has challenged the assumption that “anteroposteriorly” stable FNF are always truly stable, as fractures that appear undisplaced on anteroposterior radiographs may, in fact, exhibit sagittal instability. Studies have shown that up to 79% of FNF classified as stable on anteroposterior hip radiographs demonstrate significant sagittal displacement of the femoral head on lateral radiographs [23, 24]. Notably, our study found an even higher proportion, approaching 100%. This discrepancy is likely attributed to the complex three-dimensional (3D) structure of FNF and the biomechanical stress distribution at the time of injury. A study by Wu et al. [25], involving 3D reconstructions of CT images from 256 FNF patients, revealed that bone defects in the superior and posterior regions of the femoral neck were prevalent. They concluded that the lack of structural support due to these bone defects was a primary cause contributing to sagittal displacement of the femoral head. As awareness of sagittal femoral head displacement has increased, orthopedic surgeons have increasingly focused on the impact of anterior and posterior femoral head tilt angles on surgical outcomes [26].
Several studies have emphasized the clinical significance of the sagittal femoral head inclination angle in predicting internal fixation failure. Some scholars have reported that when the posterior inclination angle exceeds 20°, the internal fixation failure rate reaches 56%, compared to 13.6% when the angle is less than 20° (OR = 4.1) [8]. Similarly, Slullitel et al. [17] observed that approximately 48.9% of FNF patients with posterior femoral head tilt angles ≥ 20° required revision surgery, whereas only 5.5% of those with a tilt less than 20° required reoperation. Supporting this, Dolatowski et al. [27], in a prospective study of 230 FNF patients, reported a significant increase in surgical failure risk when the posterior femoral head tilt angle was ≥ 20°. Additionally, their findings highlighted an AT of ≥ 10° as an independent risk factor for surgical failure, with internal fixation failure rates reaching 56%. Sjöholm et al. [13] further confirmed that a PT ≥ 20° or an AT ≥ 10° served as strong predictive indicators of reoperation incidence in FNF (Garden Types I and II) [8].
Several studies have recommended evaluating sagittal femoral head displacement using lateral hip radiographs [11, 16, 22, 27], with Palm's method [12] being the most widely adopted approach in clinical practice. However, concerns [28] have been raised regarding the accuracy and reliability of Palm's method, particularly in cases of significant sagittal femoral head deformity, which can lead to misclassification of fractures. There are several challenges associated with using X-ray imaging for sagittal tilt angle measurement: initially, due to fracture-related pain, the affected hip is often held in a forced posture of flexion, adduction, and external rotation, making it challenging for patients to cooperate during standardized anteroposterior and lateral radiographs. Second, at the fracture site, the superimposition of the femoral head and neck on X-ray images can overlap and obscure anatomical landmarks, leading to distorted measurements. This issue is particularly pronounced in cases with greater sagittal deformity, potentially resulting in erroneous assessments of STAFH by orthopedic surgeons. Tiee et al. [16] reported that X-ray-based measurements frequently underestimated femoral head tilt angles compared to CT-based measurements. Furthermore, differences in X-ray projection centers, exposure angles, distances, and patient positioning across hospitals and radiologists contribute to measurement inconsistencies, making it difficult to obtain standardized lateral hip radiographs. Given these limitations, an increasing number of researchers advocate for the use of CT imaging to reclassify complex fractures and guide surgical planning [26, 27]. Compared to X-ray imaging, 3D-CT offers several advantages: 3D-CT enables a detailed evaluation of subtle fracture changes, allowing for a comprehensive assessment of the fracture site and its stability. Unlike X-ray imaging, which requires standardized limb positioning, 3D-CT is less affected by patient posture, minimizing examination errors due to variations in radiation exposure angles. Accurate fracture reduction via 3D-CT provides indirect insights into retinacular vascular damage [29]. In this study, we employed 3D-CT reconstruction to generate axial oblique sagittal planes of the femoral neck, enabling precise measurement of STAFH. By comparing the measurements of the retroversion angle among different physicians within the same cohort, we achieved an ICC of 0.97, which is significantly higher than previously reported values in the literature. These findings suggest that measuring the retroversion angle using 3D-CT reconstruction of the axial oblique sagittal plane offers superior accuracy and reproducibility compared to the widely adopted Palm method.
In this study, we conducted a subgroup analysis of patients based on their preoperatively measured STAFH. Given the low prevalence of cases with an AT angle of more than 0° (AT > 0°) and a posterior tilt of less than 10° (PT < 10°) in the STAFH study, and the absence of treatment failure cases within these categories, we classified patients with PT ≥ 10° into four groups, with 5° increments per group (Table 2). However, our analysis did not reveal a significant correlation between PT degree and treatment failure rate across these subgroups. This lack of significance may be attributed to the heterogeneous distribution of cases within each subgroup and the limited number of surgical failures observed. To further investigate this relationship, we reclassified all patients according to the classification method proposed by Sjöholm et al. (Table 3) [13]. Our analysis demonstrated that the surgical failure rate in the high-risk group was significantly higher than that in the low-risk group, reinforcing that excessive AT and PT of the femoral head serve as major risk factors for internal fixation failure in Garden Types I and II FNF, with an OR of 11.953. These results underscore the importance of considering the STAFH when assessing the stability of FNF and formulating treatment strategies. Although the observed OR value is notably greater than that reported in previous studies, we believe this is reasonable given differences in measurement methods—while most studies have used Palm's method, our measurements were based on 3D-CT—and variations in surgical approaches, such as the use of dynamic locking steel plates versus cannulated screws. Overall, our findings underscore that excessive sagittal femoral head displacement can significantly increase the risk of internal fixation failure in FNF.
However, this study has several limitations. As a retrospective analysis conducted at a single center, there is a potential for selection bias. Additionally, the limited sample size and uneven distribution of cases may reduce the statistical power of our findings. Furthermore, short follow-up periods and loss to follow-up in some patients increase the risk of underestimating reoperation failure rates, particularly in cases of femoral head necrosis, leading to potential data loss. To overcome these limitations, our research team is currently developing a multicenter database that includes osteoporosis and hip fracture cases from eight trauma centers, and we are in the process of updating and expanding this database. In this ongoing project, we plan to systematically incorporate additional clinical parameters, such as bone mineral density measurements and surgical approach variables. In addition, we are working to optimize data collection by refining the categorization and granularity of key variables, such as fracture displacement patterns and angiography results. Future research should include prospective multicenter studies with long-term follow-up, which will provide more robust evidence and enhance the generalizability of the research findings.
5 Conclusions
The traditional Garden classification of FNF primarily assesses displacement solely on anteroposterior radiographs, often overlooking sagittal plane displacement. However, an increase in sagittal femoral head displacement, particularly as described by Sjöholm et al. [13], substantially elevates the risk of internal fixation failure in FNF. Hence, the selection of surgical treatment for FNF should not rely solely on the Garden classification, which is based on X-ray imaging, but should also incorporate 3D-CT scanning to accurately evaluate fracture morphology and measure femoral head tilt angles, especially in stable Garden I/II fractures. In cases with significant sagittal tilt, the treatment options should align with those of unstable fractures. Total hip arthroplasty or hemiarthroplasty should be considered as alternative treatment options to mitigate the risk of surgical failure and avoid the need for secondary procedures.
Author Contributions
Lei Shi: writing – original draft (lead), validation (lead), methodology (equal), investigation (lead), formal analysis (lead), data curation (lead). Chen Chen: software (lead), methodology (equal). Junsong Wang: writing – original draft (supporting), validation (equal), methodology (supporting), formal analysis (equal), data curation (supporting). Jia Li: project administration (lead), methodology (supporting), conceptualization (lead). Peifu Tang: project administration (equal), writing – review and editing (supporting). Yuanhao Wu: project administration (supporting), funding acquisition (equal). Quanyi Guo: writing – review and editing (supporting), methodology (lead). Houchen Lyu: project administration (supporting), funding acquisition (lead).
Acknowledgments
We appreciated Mr. Yu Jiang and Fuqiang Wang from the Chinese PLA General Hospital for data preparation.
Ethics Statement
The study adhered to the principles of the Declaration of Helsinki and received approval from the institutional review board of the Chinese PLA General Hospital (No. S2023-059-01). Follow-up visits were scheduled via email or telephone, with the exclusion of patients who had deceased.
Consent
Informed consent was obtained from all subjects, or their families.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author.




