Financial burden of seeking diabetes mellitus care in India: Evidence from a Nationally Representative Sample Survey
Abstract
Background
Diabetes mellitus (DM) is a major public health concern in India, and entails a severe burden in terms of disability, death, and economic cost. This study examined the out-of-pocket health expenditure (OOPE) and financial burden associated with DM care in India.
Methods
The study used data from the latest round of the National Sample Survey on health, which covered 555,115 individuals from 113,823 households in India. In the present study, data of 1216 individuals who sought inpatient treatment and 6527 individuals who sought outpatient care for DM were analysed.
Results
In India, 10.04 per 1000 persons reported having DM during the last 15 days before the survey date, varying from 6.94/1000 in rural areas to 17.45/1000 in urban areas. Nearly 38% of Indian households with diabetic members experienced catastrophic health expenditure (at the 10% threshold) and approximately 10% of DM-affected households were pushed below the poverty line because of OOPE, irrespective of the type of care sought. 48.5% of households used distressed sources to finance the inpatient costs of DM. Medicines constituted one of the largest proportion of total health expenditure, regardless of the type of care sought or type of healthcare facility visited. The average monthly OOPE was over 4.5-fold and 2.5-fold higher for households who sought inpatient and outpatient care, respectively, from private health facilities, compared with those treated at public facilities. Notably, the financial burden was more severe for households residing in rural areas, those in lower economic quintiles, those belonging to marginalised social groups, and those using private health facilities.
Conclusion
The burden of DM and its associated financial ramifications necessitate policy measures, such as prioritising health promotion and disease prevention strategies, strengthening public healthcare facilities, improved regulation of private healthcare providers, and bringing outpatient services under the purview of health insurance, to manage the diabetes epidemic and mitigate its financial impact.
Abbreviations
-
- CHE
-
- catastrophic health expenditure
-
- DALYs
-
- disability-adjusted life years
-
- DM
-
- diabetes mellitus
-
- GDP
-
- gross domestic product
-
- LMICs
-
- low and middle-income countries
-
- NCDs
-
- noncommunicable diseases
-
- OBCs
-
- other backward classes
-
- OOPE
-
- out-of-pocket health expenditure
-
- OR
-
- odds ratio
-
- PHCs
-
- primary health centres
-
- PMJAY
-
- Pradhan Mantri Jan Arogya Yojana
-
- SCs
-
- scheduled castes
-
- STs
-
- scheduled tribes
-
- UHC
-
- universal health coverage
1 INTRODUCTION
Diabetes mellitus (DM) is a growing public health concern and is ranked among the top-10 causes of mortality and disability-adjusted life years (DALYs) worldwide [1]. In 2021, 537 million people globally had DM, and this number is expected to increase to 783 million by 2045 [2]. Notably, over 80% of individuals with DM reside in low and middle-income countries (LMICs) [2]. India has been described as the ‘Diabetes Capital of the World’ [3], accounting for one in every seven adults living with DM globally [2]. In 2021, India was ranked second in terms of the number of adults living with DM, and third in terms of DM-related mortality worldwide [2]. Between 1990 and 2016, India experienced a 29.3% increase in age-standardised prevalence of DM and 39.6% increase in age-standardised DALYs rate for DM, the highest increase among major non-communicable diseases (NCDs) [4, 5]. The economic consequences of DM are dire, resulting in substantial medical and nonmedical expenses as well as productivity losses in LMICs such as India [6-10]. As per the International Diabetes Federation, the total DM-related health expenditure in India was USD 8.5 billion in 2021 and is projected to rise to USD 10.3 billion by 2030 [11]. Moreover, India has one of the lowest public health expenditure (1.15% of GDP) [12], and one of the highest out-of-pocket health expenditure (OOPE) (58.7% of total health expenditure) in the world [13]. Heavy dependence on OOPE impedes access to healthcare services, as well as exposes households to financial catastrophe and falling into or intensifying poverty.
The rising burden of DM in India [2, 14], accompanied by dismally low health insurance coverage [15], a significant reliance on OOPE, and the dominant presence of the fee-for-service private health sector [16], highlights the substantial economic burden imposed on DM-affected households. To mitigate this economic impact, it is crucial to conduct a comprehensive examination of the financial strain associated with diabetes care in the country. However, limited evidence is available regarding the financial impact of seeking DM care in India. Previous studies were restricted to specific geographical areas [17-21] or relied on older data sets [22, 23], focusing on a few aspects such as assessing the OOPE and associated financial burden due to DM only across economic quintiles [23] or only for inpatient care [22].
Our study aims to fill the gap in the existing literature by comprehensively examining the OOPE and financial burden associated with DM care in India. For this purpose, we employed the latest nationally representative survey data conducted by the National Sample Survey Organisation (NSSO). Specifically, our study was guided by the following objectives. First, we estimated the number of people who reported having DM in India. Second, we estimated OOPE and determined the proportion of various components (e.g., doctors' fees, the cost of medicines, diagnostic tests) of total health expenditure. Third, we estimated the financial burden of OOPE using three metrics: incidence of experiencing catastrophic health expenditure (CHE), percentage of households falling below the poverty line because of OOPE, and the incidence of relying on distressed sources. Fourth, we estimated the percentage of diabetic individuals who did not seek treatment, and the percentage of diabetic individuals who did not seek treatment on medical advice and their reasons for doing so. Finally, we assessed the loss of household income resulting from seeking hospitalisation and outpatient care due to DM. All measures were estimated separately by the type of care sought (inpatient and outpatient) and type of healthcare facility visited (public and private) to facilitate a nuanced and detailed analysis. Examining the financial burden of DM care is crucial from a policy standpoint to ameliorate the financial hardships experienced by diabetic patients and their families. Our analysis using nationally representative estimates of costs and financial impact are expected to assist in designing strategies to enhance financial risk protection for Indian households.
2 DATA AND METHODOLOGY
2.1 Overview of data source
The study employed data from the 75th round of the National Sample Survey on health, named ‘Household Social Consumption: Health’. The survey was conducted by the NSSO during 2017–2018 and covered 555,115 individuals from 113,823 households in India. The survey used a stratified multistage sampling design, with villages and urban blocks as the first stage units in rural and urban areas, respectively, and households as the second stage units. In addition to collecting information about socioeconomic and demographic characteristics, the survey gathered extensive information about the nature of ailments, utilisation patterns of healthcare facilities, and expenses incurred on inpatient and outpatient treatment. In this study, we analysed data of 1216 individuals (from 1215 households) who sought inpatient treatment for DM and 6527 individuals (from 5719 households) who sought outpatient care for DM.
2.2 Outcome variables
2.2.1 Out-of-pocket health expenditure (OOPE)
The NSSO survey collected detailed information about the total health expenditure under three subcategories: medical, nonmedical, and transportation expenses. To calculate the OOPE, we subtracted any reimbursements received from the total health expenditure. The survey recorded inpatient and outpatient expenses incurred during the last 365 days and 15 days, respectively, which were converted into monthly figures.
2.2.2 Catastrophic health expenditure (CHE)
In the existing literature, there is no consensus regarding the threshold. Hence, we computed the CHE at three thresholds: 10%, 20%, and 40% [26].
2.2.3 Poverty headcount ratio
2.2.4 Distressed financing
We defined a household as using distressed financing if it relied on borrowings, sale of physical assets, contributions from friends and relatives, or other sources to pay for OOPE [29]. In the case of inpatient care, the NSSO survey grouped sources of finance into major and second major categories, as households might have used more than one source. Therefore, if a household used borrowings and contributions as its major and second major sources of finance, respectively, we included such household in both categories [29]. Hence, the total incidence of all sources of finance could be greater than 100% for inpatient care.
2.3 Statistical analysis
Descriptive statistics and multivariable logistic regression were employed in the study.
In the above equation, is the probability of occurrence of a binary outcome variable, that is, incurring CHE, impoverishment, and distressed financing for the household. represent variables, namely economic quintiles, social group1 (i.e., Scheduled Tribes [STs], Scheduled Castes [SCs], Other Backward Classes [OBCs], and Others), household's principal source of income, religion (i.e., Hinduism, Islam, Others), place of residence (i.e., rural or urban areas), gender and educational status of household head, any elderly member in household, health insurance status, and type of healthcare facility visited.
Sample weights provided by the NSSO were applied as applicable. All analyses were performed using Stata Version 14.1.
3 RESULTS
In India, 10.04 per 1000 persons reported having DM during the last 15 days before the survey date, varying from 6.94/1000 in rural areas to 17.45/1000 in urban areas (Supporting Information: Table 1). Females reported a slightly higher burden of DM (10.43/1000) compared with males (9.68/1000). Individuals aged 60 years and above reported the highest burden of DM (65.73/1000). The number of individuals reporting DM was higher among those belonging to other social groups (16.35/1000) compared with STs (2.09/1000), SCs (6.62/1000), and OBCs (9.43/1000). Notably, the burden of DM ranged from 3.55/1000 among individuals belonging to the poorest economic quintile to 21.91/1000 among those in the wealthiest economic quintile. The number of persons reporting DM was substantially higher among individuals primarily earning through regular wages or salaries (14.01/1000) and other work (38.98/1000) compared with those working as casual labourers (6.07/1000) and those who were self-employed (8.25/1000).
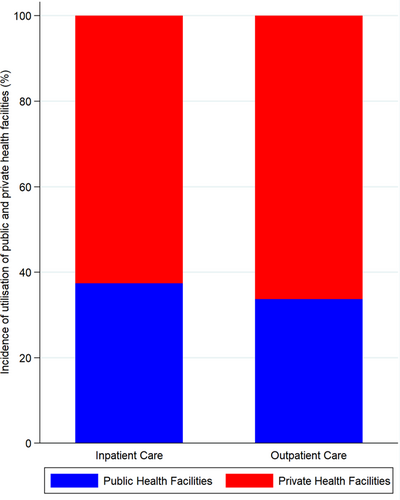
3.1 OOPE and share of various components
Supporting Information: Table 2 shows the average monthly OOPE of households by the type of care sought. The average OOPE was INR 1555.42 for inpatient care and INR 1380.2 for outpatient care. Urban households reported higher OOPE than their rural counterparts, irrespective of the type of care sought. The OOPE was invariably higher for households who sought DM treatment from private facilities compared with those treated in public facilities in the case of both inpatient (INR 2139.6 vs. INR 459.8) and outpatient care (INR 1760.3 vs. INR 690.0) (Supporting Information: Tables 3–6). 62.6% of inpatient cases and 66.3% of outpatient cases were sought at private health facilities (Figure 1; Supporting Information: Table 7). The key reasons for not choosing the public health facilities (by those who chose private health facilities) were nonavailability of doctors or the quality of public health facilities being unsatisfactory, and a preference for a trusted doctor or hospital, regardless of the type of care sought (Supporting Information: Figure 1).
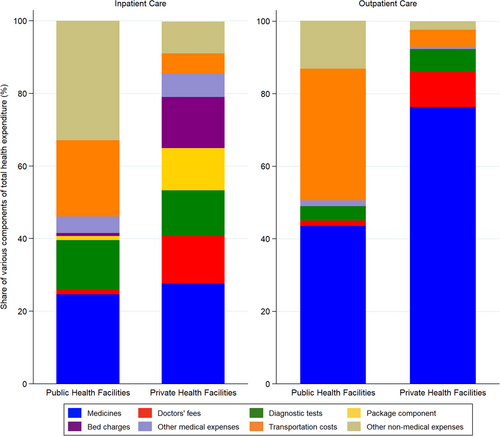
Medicines constituted one of the largest share of expenses in the case of both inpatient care (private facilities: 27.6%; public facilities: 24.7%) and outpatient care (private facilities: 76.3%; public facilities: 43.5%) (Figure 2). Notably, the relative burden of nonmedical expenses was higher at public facilities compared with private facilities, both for inpatient (32.9% vs. 8.8%) and outpatient care (13.2% vs. 2.4%). Likewise, the share of transportation expenses was over 3.5 times (7.5 times) higher for public facilities compared with private facilities in the event of inpatient (outpatient care). Conversely, when hospitalisation was sought at private facilities, bed charges (14.1%) and doctors' fees (13.1%) were the leading contributors to the total health expenditure after medicines.
3.2 Catastrophic health expenditure
Of all the households who sought inpatient care for DM, 37.9%, 20.3%, and 8.8% of households experienced CHE at the 10%, 20%, and 40% thresholds, respectively (Table 1). The CHE incidence in the case of outpatient care for DM was 37.9%, 20.7%, and 8.9% at the 10%, 20%, and 40% thresholds, respectively. Rural households experienced higher CHE incidence compared with their urban counterparts, regardless of the type of care sought and across all thresholds. Households belonging to marginalised social groups (STs and SCs) reported higher CHE incidence compared with those belonging to OBCs and other social groups across all thresholds for both inpatient and outpatient care. In the case of outpatient care for DM, households belonging to the bottom two economic quintiles reported higher CHE incidence at the 10% threshold (Quintile 1: 59.7%; Quintile 2: 41.9%) than those belonging to the wealthiest quintile (Quintile 5: 30.8%), with a similar pattern observed across all thresholds. Furthermore, households whose principal source of earnings was from regular wages or salaries reported the lowest CHE incidence at all thresholds for inpatient care. The CHE incidence (at all thresholds) was over 3-fold and 2-fold higher for households who sought DM care from private health facilities compared with those who were treated in public facilities in the event of inpatient and outpatient care, respectively (Supporting Information: Tables 3–6).
| Inpatient care | Outpatient care | |||||
|---|---|---|---|---|---|---|
| Socioeconomic characteristics | At 10% threshold (%) | At 20% threshold (%) | At 40% threshold (%) | At 10% threshold (%) | At 20% threshold (%) | At 40% threshold (%) |
| Region | ||||||
| Rural | 44.7 (40.5–48.8) | 22.6 (19.2–26.1) | 9.8 (7.3–12.3) | 42.9 (40.9–44.9) | 25.7 (23.9–27.5) | 11.2 (9.9–12.5) |
| Urban | 29.6 (26.1–33.1) | 17.4 (14.4–20.3) | 7.6 (5.5–9.6) | 33.0 (31.4–34.6) | 15.8 (14.6–17.0) | 6.6 (5.8–7.4) |
| Social group | ||||||
| Scheduled tribes | 60.1 (51.2–69.0) | 41.9 (32.9–50.9) | 16.3 (9.6–23.0) | 60.8 (54.3–67.3) | 36.7 (30.3–43.1) | 18.6 (13.4–23.8) |
| Scheduled castes | 43.2 (35.6–50.9) | 27.4 (20.5–34.3) | 11.2 (6.3–16.1) | 40.3 (36.7–43.9) | 24.2 (21.0–27.3) | 8.3 (6.3–10.4) |
| Other backward classes | 32.1 (28.0–36.1) | 20.2 (16.7–23.7) | 9.4 (6.9–11.9) | 36.0 (34.1–38.0) | 19.5 (17.8–21.1) | 8.7 (7.5–9.8) |
| Other | 41.9 (37.2–46.6) | 14.8 (11.4–18.2) | 5.9 (3.7–8.2) | 38.0 (36.1–39.9) | 20.2 (18.6–21.7) | 8.8 (7.7–10.0) |
| Major source of household income | ||||||
| Self-employment | 42.4 (38.2–46.6) | 23.8 (20.1–27.4) | 10.2 (7.6–12.7) | 38.8 (36.9–40.7) | 21.4 (19.8–23.1) | 10.0 (8.8–11.2) |
| Regular wage or salary | 23.8 (19.3–28.4) | 12.7 (9.1–16.2) | 3.7 (1.7–5.7) | 33.9 (31.6–36.2) | 18.2 (16.3–20.0) | 6.0 (4.8–7.1) |
| Casual labour | 40.7 (33.4–47.9) | 18.5 (12.8–24.3) | 8.7 (4.5–12.9) | 33.8 (30.4–37.2) | 16.4 (13.8–19.1) | 6.3 (4.6–8.0) |
| Other | 43.0 (35.7–50.4) | 26.2 (19.6–32.7) | 14.0 (8.8–19.2) | 45.6 (42.2–48.9) | 26.8 (23.8–29.8) | 12.9 (10.7–15.1) |
| Economic quintiles | ||||||
| Quintile 1 | 55.3 (47.4–63.2) | 18.4 (12.3–24.6) | 8.9 (4.4–13.4) | 59.7 (55.1–64.3) | 42.5 (37.9–47.2) | 16.1 (12.7–19.6) |
| Quintile 2 | 35.6 (28.7–42.5) | 21.0 (15.1–26.9) | 8.8 (4.8–12.9) | 41.9 (38.5–45.4) | 24.1 (21.2–27.1) | 14.9 (12.5–17.4) |
| Quintile 3 | 36.6 (30.0–43.2) | 25.1 (19.2–31.0) | 12.1 (7.7–16.6) | 39.5 (36.3–42.7) | 21.6 (18.9–24.3) | 7.8 (6.0–9.5) |
| Quintile 4 | 39.7 (33.6–45.8) | 23.8 (18.5–29.1) | 6.7 (3.6–9.8) | 41.7 (38.9–44.5) | 22.6 (20.2–24.9) | 9.5 (7.8–11.2) |
| Quintile 5 | 31.7 (27.2–36.2) | 15.3 (11.9–18.8) | 8.4 (5.7–11.0) | 30.8 (28.9–32.7) | 15.0 (13.5–16.4) | 5.9 (5.0–6.9) |
| Total | 37.9 (35.2–40.6) | 20.3 (18.0–22.5) | 8.8 (7.2–10.4) | 37.9 (36.7–39.2) | 20.7 (19.7–21.8) | 8.9 (8.2–9.6) |
- Note: () 95% confidence interval.
3.3 Poverty headcount ratio
Table 2 shows that 10.4% and 9.9% of all DM-affected households who sought inpatient and outpatient care, respectively, were pushed below the poverty line because of OOPE. The poverty headcount ratio was substantially higher among rural households (inpatient care: 13.6%; outpatient care: 13.6%) compared with their urban counterparts (inpatient care: 6.6%; outpatient care: 6.2%). Households belonging to STs (20.5%), SCs (15.8%), and OBCs (11.0%) reported higher poverty headcount ratios than those belonging to other categories (6.1%) in the case of inpatient care. The percentage of households falling below the poverty line was higher among lower economic quintiles compared with wealthier quintiles, regardless of the type of care sought. Furthermore, households primarily earning from regular wages or salaries reported the lowest poverty headcount ratio for inpatient care. The poverty headcount ratio was higher among households who sought DM care from private facilities compared with those treated in public facilities in the case of both inpatient (13.1% vs. 4.7%) and outpatient care (11.3 vs. 8.1%) (Supporting Information: Tables 3–6).
| Socioeconomic characteristics | Inpatient care (%) | Outpatient care (%) |
|---|---|---|
| Region | ||
| Rural | 13.6 (10.8–16.5) | 13.6 (12.2–15.0) |
| Urban | 6.6 (4.7–8.5) | 6.2 (5.4–7.0) |
| Social group | ||
| Scheduled tribes | 20.5 (13.2–27.9) | 7.8 (4.2–11.4) |
| Scheduled castes | 15.8 (10.1–21.5) | 12.7 (10.3–15.2) |
| Other backward classes | 11.0 (8.3–13.7) | 10.0 (8.8–11.3) |
| Other | 6.1 (3.8–8.4) | 9.0 (7.8–10.1) |
| Major source of household income | ||
| Self-employment | 12.0 (9.3–14.8) | 11.7 (10.4–12.9) |
| Regular wage or salary | 4.6 (2.3–6.8) | 8.0 (6.7–9.3) |
| Casual labour | 11.5 (6.7–16.2) | 7.7 (5.8–9.6) |
| Other | 13.8 (8.6–18.9) | 10.2 (8.2–12.2) |
| Economic quintiles | ||
| Quintile 1 | 7.8 (3.5–12.0) | 19.6 (15.9–23.4) |
| Quintile 2 | 20.3 (14.5–26.1) | 24.2 (21.2–27.2) |
| Quintile 3 | 16.4 (11.3–21.5) | 14.2 (11.9–16.5) |
| Quintile 4 | 8.2 (4.8–11.6) | 9.4 (7.8–11.1) |
| Quintile 5 | 4.6 (2.6–6.6) | 2.4 (1.8–3.0) |
| Total | 10.4 (8.7–12.2) | 9.9 (9.1–10.6) |
- Note: () 95% confidence interval.
3.4 Incidence of distressed financing
Of all the households who sought inpatient treatment, 48.5% relied on distressed sources either as the major or second major source to cope with the cost of DM care (Table 3). Borrowings (25.3%) and contributions from friends and relatives (18.5%) were the most common distressed sources for financing inpatient care, whereas outpatient care was predominantly financed through income and savings (94.9%) (Supporting Information: Figure 2). Notably, more than 50% of households residing in rural areas, those belonging to lower economic quintiles, those belonging to OBCs, and those earning from casual work used distressed sources to pay for inpatient-related OOPE (Table 3). The incidence of using distressed sources was higher among households who sought inpatient services from private health facilities (50.9%) than those treated in public facilities (43.3%) (Supporting Information: Tables 3 and 4).
| Socioeconomic characteristics | Inpatient care % | Outpatient care % |
|---|---|---|
| Region | ||
| Rural | 54.4 (50.2–58.5) | 5.5 (4.6–6.5) |
| Urban | 41.4 (37.6–45.2) | 4.7 (3.9–5.4) |
| Social group | ||
| Scheduled tribes | 44.4 (35.3–53.6) | 9.7 (5.5–13.9) |
| Scheduled castes | 47.8 (40.0–55.6) | 3.9 (2.4–5.4) |
| Other backward classes | 50.1 (45.7–54.4) | 6.0 (5.0–7.0) |
| Other | 47.0 (42.3–51.8) | 4.4 (3.5–5.2) |
| Major source of household income | ||
| Self-employment | 43.2 (39.0–47.5) | 2.6 (2.0–3.3) |
| Regular wage or salary | 36.8 (31.5–42.0) | 4.7 (3.7–5.8) |
| Casual labour | 69.9 (63.0–76.7) | 4.4 (2.9–6.0) |
| Other | 42.9 (35.5–50.3) | 12.6 (10.3–14.9) |
| Economic quintiles | ||
| Quintile 1 | 59.0 (51.2–66.8) | 4.8 (2.7–6.8) |
| Quintile 2 | 57.0 (49.8–64.1) | 4.6 (3.1–6.1) |
| Quintile 3 | 61.7 (55.0–68.4) | 5.7 (4.2–7.3) |
| Quintile 4 | 39.1 (33.0–45.2) | 1.8 (1.0–2.6) |
| Quintile 5 | 39.3 (34.6–44.0) | 6.7 (5.7–7.7) |
| Total | 48.5 (45.7–51.4) | 5.1 (4.5–5.7) |
- Note: () 95% confidence interval.
3.5 Proportion of diabetic individuals not seeking treatment
Of all the individuals who reported having DM during the last 15 days before the survey date, 0.8% did not seek treatment (Supporting Information: Table 8). The incidence of not seeking treatment was the highest among individuals belonging to the lowest economic quintile (5.2%), those belonging to OBCs (1.5%), and those residing in rural areas (1.4%). We also found that 2.6% of diabetic individuals did not seek treatment on medical advice during the last 15 days (Supporting Information: Table 8). The primary reasons for not seeking treatment on medical advice were that the ailment was not considered severe (43.0% of cases) and other reasons (50.1% of cases). In only 0.9% of cases, individuals reported financial reasons (i.e., expensive facilities) for not seeking treatment on medical advice, ranging from 0.1% in rural areas to 2.2% in urban areas. In contrast, a considerable proportion of individuals from the lowest economic quintile (20.5%) and OBCs (10.4%) reported the nonavailability of medical facilities in their neighbourhood as one of the reasons for not seeking treatment on medical advice (Supporting Information: Figure 3).
3.6 Loss of household income
Households not only bear the financial cost of healthcare but also experience indirect costs, such as loss of earnings, when the patient or caregiver is unable to work. We found that the average loss of household income caused by hospitalisation for DM was INR 3330.9, and that caused by outpatient care was INR 88.2 (Supporting Information: Table 9). Households belonging to STs (INR 4769.7) and other social groups (INR 4355.6), those in the middle-economic quintile (INR 4226.3), those primarily earning through self-employment (INR 4031.2), and those residing in urban areas (INR 3976.3) reported the highest loss of household income because of inpatient treatment for DM.
3.7 Multivariable logistic regression
Supporting Information: Table 10 shows the results of multivariable logistic regression to reveal the impact of various socioeconomic and demographic factors on the likelihood of incurring CHE (at the 10% threshold) due to DM. Rural households were significantly more likely to experience CHE for both inpatient (odds ratio [OR]: 2.59 [1.56–4.29]; p < 0.05) and outpatient care (OR: 2.64 [1.92–3.63]; p < 0.05) compared with their urban counterparts. Utilisation of private health facilities significantly increased the likelihood of experiencing CHE, irrespective of the type of care sought (p < 0.05). Households belonging to STs were more likely to experience CHE (OR: 4.32 [1.93–9.70]; p < 0.05) for inpatient care compared with other social groups. In the case of outpatient care, female-headed households (OR: 1.59 [1.07–2.37]; p < 0.05) and households primarily earning from other work (OR: 1.72 [1.11–2.65]; p < 0.05) were significantly more likely to incur CHE. Conversely, the odds of experiencing CHE were significantly lower among households belonging to higher economic quintiles, regardless of the type of care sought (p < 0.05). Insurance coverage significantly decreased the odds of incurring CHE for inpatient care (OR: 0.57 [0.33–0.96]; p < 0.05). Households earning primarily from regular wages or salaries were significantly less likely to incur CHE for inpatient care (OR: 0.46 [0.26–0.81]; p < 0.05) compared with those earning from self-employment. Similarly, place of residence, economic quintile, and type of healthcare facility visited emerged as statistically significant predictors of households' likelihood of falling into poverty and using distressed financing (Supporting Information: Table 10).
4 DISCUSSION
Universal Health Coverage (UHC), which aims to ensure that everyone has access to quality healthcare without facing financial hardship [33], has been adopted as one of the Sustainable Development Goals [34]. Financial protection is only achieved when there is no financial hardship caused by OOPE and no financial barriers to accessing care [35]. The prominent parameters used in the existing literature to capture the undesirable effects of OOPE are CHE and impoverishment [36-38]. Households may even resort to distressed coping strategies, such as borrowing money, sale of assets, and seeking contributions from friends and relatives to finance OOPE [29, 39]. Furthermore, households might forgo necessary healthcare because of financial constraints, thereby exacerbating health problems and putting the concerned families into a downward spiral of ill-health and poverty [39-41]. As per a recent review [39], comprehensive financial risk studies must measure four indicators to provide a holistic picture of the financial hardships experienced by households: (i) CHE, (ii) impoverishment, (iii) adoption of distressed coping strategies and (iv) forgone care due to financial reasons. Therefore, in the current study, we estimated the financial burden by examining all four parameters in respect of DM care in India.
We found that 37.9% of Indian households with diabetic members experienced CHE (at 10% threshold) and nearly 10% of DM-affected households fell below the poverty line because of OOPE, regardless of the type of care sought. Outpatient care was primarily financed through income or savings, whereas 48.5% of households used distressed sources to finance inpatient care for DM. Additionally, 0.8% of individuals with DM did not seek treatment and 2.6% of individuals did not seek treatment on medical advice. Medicines were the main constituent of health expenditure, regardless of the type of care sought and healthcare facility visited. Moreover, OOPE and the associated financial burden were substantially higher for households seeking DM care from private health facilities compared with those treated in the public facilities.
We observed that the number of persons reporting having DM was higher among the elderly, urban residents, individuals belonging to wealthier quintiles, other social groups, those with higher educational status, and those primarily earning from regular wages or salaries and other work. The higher burden of DM among individuals with higher socioeconomic status might reflect greater exposure to risk factors, such as excessive calorie intake, sedentary lifestyles, and low physical activity [42-48]. Additionally, the higher burden could also be attributed to greater awareness and access to healthcare among such individuals [49]. Importantly, knowledge and awareness about DM and its risk factors is very low in India, particularly in rural areas [50, 51]. According to the Indian Council of Medical Research India Diabetes Study [50], only 43.2% of the study population had heard of diabetes, and the level of awareness was significantly lower among rural individuals (36.8%) compared with urban individuals (58.4%). If DM is not detected early and treated adequately, there is an increased risk of developing DM-related complications, increased healthcare use, and associated costs [2, 51].
In accord with previous studies [21, 23, 52-54], we found that DM imposes a substantial financial burden on Indian households. We observed that households residing in rural areas, those belonging to lower economic quintiles, those belonging to marginalised social groups (STs and SCs), and those primarily earning through casual, self-employment and other work, experienced higher financial burden caused by DM care. According to a case–control study, individuals with DM reported 2 times more days of inpatient treatment, 1.3 times more outpatient visits, and 9.7 times more medications than nondiabetic individuals; thereby, imposing severe financial strain on DM-affected households [55]. The high cost of DM care forces poor and vulnerable people to delay treatment [56], reduce their medication dosage to make drugs last for a longer period [57] or resort to borrowing or selling assets to finance care [23, 58]. The situation is further complicated by inadequate public healthcare facilities and a scarcity of healthcare workers, particularly specialists (for instance, 80% shortfall of specialists at community health centres) in the Indian rural healthcare system [59]. Additionally, paucity of basic items such as glucometers or test strips for glucometers is a major concern. For instance, a previous study reported that only 20% of primary health centres (PHCs) in the state of Odisha had glucometers [60]. This situation forces people to travel long distances to access medical care [61-63], leading to substantial costs associated with travel and lodging and income loss caused by it. Therefore, it is crucial to strengthen the public healthcare system to ensure timely access to care, improve health outcomes, and reductions in OOPE. In this regard, the creation of 150,000 Health and Wellness Centres by transforming existing subhealth centres and PHCs to provide comprehensive primary healthcare for NCDs is a laudable initiative by the Indian government [64]. Moreover, telemedicine has the potential to overcome barriers and enhance the quality and accessibility of DM care in remote regions, as evidenced by successful programmes such as the Diabetes Tele Management System and the Chunampet Rural Diabetes Prevention Project Model [65-67].
Interestingly, we found that outpatient care was as burdensome as inpatient care, causing 37.9% of DM-affected households to incur CHE (at the 10% threshold) and pushing 9.9% of households below the poverty line. The financial burden caused by outpatient care can be attributed to recurring visits, relatively small but ongoing expenses, and over-dependence on the private healthcare sector [68, 69]. Moreover, in India, the rising prevalence of NCDs, such as DM and cardiovascular conditions, leads to a greater need for outpatient facilities as chronic illnesses demand regular health check-ups, doctors' visits, diagnostic tests, and long-term drug support [69, 70]. Despite this, the majority of the government-sponsored health insurance schemes in India cover only inpatient treatment, leaving outpatient care outside the purview of health insurance [71, 72]. Recently, the government of India launched the largest government-sponsored health insurance scheme, ‘Pradhan Mantri Jan Arogya Yojana (PMJAY)’, with the objective of providing annual cover of INR 500,000 per household for secondary and tertiary care inpatient services to over 100 million poor and vulnerable families [73]. However, it must be noted that the PMJAY scheme does not cover outpatient care, which is a significant contributor to the financial burden in India.
In accord with previous studies [23, 74], we found that medicines are among the largest contributors of healthcare expenses in the case of both inpatient (private facilities: 27.6%; public facilities: 24.7%) and outpatient care (private facilities: 76.3%; public facilities: 43.5%). The poor availability of free or subsidised essential drugs in public health facilities compels individuals to purchase medicines from open markets, leading to higher OOPE or forgone treatments [75]. Previous studies reported that the availability of essential diabetes medicines in both public and private sectors in the state of Kerala and insulin availability in the public sector in Bengaluru fell short of the World Health Organization target of 80% availability of essential medicines for NCDs [76, 77]. A recent study found that 51.4% and 24.6% of Indian households with DM members were unable to afford insulin and metformin, respectively, with the highest unaffordability reported in rural areas and among the lowest income tertile [78]. Moreover, as per a recent study examining the availability and affordability of essential medicines for diabetes in 22 countries, it was found that among the 2972 surveyed DM patients in India, 71.5% did not take any diabetes medicine [78]. The key impediments to accessibility to insulin are unaffordable prices, excessive reliance on foreign-made insulin, and a problematic alliance between Indian doctors and foreign manufacturers, which forces patients to buy expensive insulin instead of cheaper local brands [79, 80]. To curtail expenditure on medicines, the Indian government introduced the Pradhan Mantri Bhartiya Janaushadhi Pariyojana to provide access to quality generic medicines at affordable prices [81]. Adopting generic medicines can significantly reduce the financial burden caused by DM [82]. Furthermore, it is imperative to improve drug procurement and supply chain systems to ensure a steady supply of free medicines in the public health facilities [76, 83].
The current study underscores the crucial role of public health facilities in delivering DM care, as the financial burden was substantially lower among households who sought treatment from public hospitals compared with those treated in private facilities. Nevertheless, we found that the shortcomings in the public health sector, such as unsatisfactory quality or unavailability of doctors and long waiting times, prompt individuals to seek care from private facilities, resulting in financial hardships. Physicians from public healthcare facilities report a lack of specialised training, patient overload, and poor follow-up as operational gaps in the delivery of DM care in India [84]. The low level of public health expenditure has limited the capacity and quality of healthcare services in India's public health sector [85], highlighting the necessity to increase government health spending. We found that over 60% of inpatient and outpatient care for DM was sought at private health facilities. In India, the private health sector employs more than 80% of doctors involved in treating DM and its associated complications, which is one of the reasons of patients prefering private facilities [86]. The private sector delivers a substantial proportion of NCD-related care in India [60, 87, 88], exacerbating concerns about cost. Previous studies have documented instances of overcharging, unnecessary tests and treatments, and malpractices in the private health sector, largely because of inadequate monitoring by the government [83, 89-92]. A recent report suggests that improved regulation is a key driver of decreasing costs and improving quality of care [83].
4.1 Strengths and limitations of the study
To the best of our knowledge, this is the first comprehensive study examining all four indicators of financial burden (CHE, impoverishment, distressed financing, and foregone care), disaggregated by the type of care sought (inpatient or outpatient) and type of healthcare facility visited (public or private), to provide a holistic picture of the financial hardships experienced by Indian households with any member suffering from DM. The strength of this study also lies in its use of the latest nationally representative survey data on health, which enhances the generalisability of the study results.
This study also involved few limitations that should be considered while interpreting the findings of the study. First, the NSSO survey collects information on self-reported ailments, which can be susceptible to under-reporting [93]. In the case of a few ailments, such as DM, a reported diagnosis by a qualified healthcare practitioner was required. However, it is estimated that over 50% of individuals with DM remain undiagnosed in India [2]; therefore, under-reporting of DM cases is a potential limitation of our study. Second, the higher burden of DM among individuals belonging to higher socioeconomic status should be interpreted with caution, because it might be attributed to either greater exposure to risk factors or better awareness and access to healthcare among such individuals. However, since the NSSO survey does not provide details about the individual-specific risk factors associated with DM (such as body mass index and tobacco use) and the exact cause of visiting the healthcare facility, it limited our ability to conduct a more nuanced analysis. Finally, the expenditure data were self-reported and may be subject to recall bias, particularly for inpatient care, where the recall period is 365 days.
5 CONCLUSION
The current study highlights the colossal financial burden of OOPE experienced by DM-affected households in India. The burden of DM and its associated financial impact necessitate the need for multisectoral efforts, such as increasing government health expenditure, strengthening the public health sector, and improving regulatory implementation for private healthcare providers to augment financial risk protection. Policy measures to increase the uptake of health insurance and consider outpatient services under the purview of health insurance are also necessary to alleviate financial hardship. Moreover, ensuring the affordability of insulin and other essential drugs is imperative. Finally, for long-term sustainability, policymakers must prioritise health promotion and disease prevention strategies to contain the diabetes epidemic and associated financial burden.
AUTHOR CONTRIBUTIONS
Both the authors contributed to the conception and design of the study. Mehak Nanda conducted the data analysis and wrote the initial draft of the manuscript. Rajesh Sharma reviewed the manuscript and supervised the work. All authors contributed to the study and approved the submitted version.
ACKNOWLEDGMENTS
This study has received no specific grant from any funding agency in public, commercial or not-for-profit sectors.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ETHICS STATEMENT
This study is based upon secondary data, which is available in the public domain. Hence, it does not require ethics committee approval.
INFORMED CONSENT
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
This study used data from the 75th round of the National Sample Survey on Health. Data are available in the public domain https://www.mospi.gov.in/.
REFERENCES
- 1 STs and SCs are the two most socially backward and economically disadvantaged social groups in India [30, 31]. OBCs include backward classes of citizens other than SCs and STs as specified in the lists prepared by the Government of India, which are periodically updated [32].
- 2 USD 1 = INR 68.3 using average 2018 exchange rate.




