Selective forgetting of self-threatening statements: Mnemic neglect for dementia information in people with mild dementia
Abstract
Objective
We tested whether people with dementia manifest selective forgetting for self-threatening information, the mnemic neglect effect (MNE). This selective forgetting is observed among healthy adults in the recall, but not the recognition, of self-threatening feedback.
Methods
Sixty-four statements about dementia were rated for their level of negativity by 280 staff and students at University of the West of England. The 12 statements rated as most negative and the 12 statements rated as least negative were then read to 62 people with dementia. Participants were randomized to 1 of 2 conditions with the statements referring either to self or to another person. High-negativity and self-referent statements had strong threat potential. Participants recalled the statements and then completed a recognition task, which consisted of the 24 previously read statements and 24 new statements.
Results
Participants manifested the MNE: They recalled fewer high-negativity (compared with low-negativity) statements, but only when these referred to the self rather than another person. This pattern occurred independently of levels of depression or anxiety. Participants also made more self-protective intrusion errors when the statements referred to the self than another person. Participants did not differ in their recognition of statements.
Conclusion
The MNE occurs among people with dementia. The selective forgetting of highly negative, self-referent statements serves to protect the self against the threat that dementia represents. Given the similarities between the MNE and the clinical phenomenon of repression, the findings may mark psychological processes that are implicated in the acceptance (or lack thereof) of a dementia diagnosis.
Key points
- The mnemic neglect effect (MNE) involves selective forgetting of information that threatens the self. The MNE occurs among healthy adults, but it is not known whether MNE occurs among people with dementia.
- Sixty-two people examined with mild dementia recalled 24 dementia-related statements that we experimentally varied whether the statements (1) referred either to the self or another person and which (2) were high or low in negativity.
- Participants manifested the MNE: They recalled fewer high-negativity statements when these statements referred to the self than another person. Recall of low negativity statements was not affected by whether these statements referred to the self or another person.
- The MNE occurs for people who are living with dementia. Selective forgetting of highly negative and self-referent (dementia-related) information serves to protect the self against threat.
1 INTRODUCTION
Dementia is a syndrome caused by a cluster of illnesses, the most common of which is the Alzheimer disease. All forms of dementia are characterized by the progressive and gradual deterioration of cognitive abilities, although the nature and severity of these deficits differ depending on the specific diagnosis. Alzheimer disease is marked by progressive impairment in episodic memory, manifesting as forgetting, as well as problems with recognition and language. Other forms of dementia include dementia with Lewy bodies, associated with visual hallucinations, and frontotemporal dementia, associated with poor executive function (eg, decision making and planning).
Although some dementia symptoms can be treated, there is no cure. As dementia progresses, not only do symptoms worsen, but they also become widespread, so that ultimately almost all domains of an individual's functioning are impaired. The personal consequences of this global decline include increasing difficulty in performing many activities that are taken for granted in everyday life, a cumulative dependency on others, and profound changes in social relationships.
A common theme across psychological approaches to dementia has been to position it as a threat to the self1-3 or to facets of the self, such as well-being4-6 and relationships.7-9 If dementia represents a threat to the self, then the social psychological literature on self-protection, that is, on psychological mechanisms that underlie the processing and recall of self-threatening information (eg, negative feedback), are likely to be relevant in understanding how people with dementia respond to the most threatening aspects of it.
A prominent theoretical formulation of feedback processing and recall is the mnemic neglect model. At the heart of this model is the mnemic neglect effect (MNE), which is defined as selective forgetting of self-threatening feedback.10 Specifically, participants recall poorly experimenter-provided feedback (in the form of statements or behaviours they are likely to enact) that is self-threatening compared with feedback that is not so. Although participants encode both types of feedback, they process self-threatening (compared with non–self-threatening) feedback in a relatively shallow manner, which in turn impedes retrieval. However, initial encoding of the feedback is sufficiently strong to ensure good recognition of it—both self-threatening and non–self-threatening. In addition, recognition is dissociated from recall: Whereas the former refers to a discrimination task that is largely based on feelings of familiarity, the latter involves the conscious retrieval of details from memory.11
The MNE has been robustly observed in laboratory and naturalistic settings.10
It functions to protect the self. That is, participants engage in selective forgetting in an attempt to protect the self from the psychological discomfort that self-threatening information entails. People with dementia often come across information related to their illness, much of which may well threaten their sense of self. It is possible, therefore, that they exhibit the MNE for dementia-related information. This is the research question we addressed in the current study.
We reasoned that dementia-related information can be a potent source of self-threat. Self-threat, though, will vary. In particular, dementia-related information may range from high to low on negativity. High-negativity information is diagnostic or accurate of the illness and emphasizes the serious consequences of it for well-being (eg, “The illness means that you may forget the names of friends or family” and “As the illness gets worse, so you will increasingly come to rely on others”), whereas low-negativity information is relatively nondiagnostic of the illness and refers largely to encouraging or manageable consequences of it for well-being (eg, “People with your illness can be distracted away from their problems” and “The illness means you will still be able to learn to do new activities”). Further, dementia-related information may refer to one's self (eg, when provided directly by a medical practitioner during an assessment) or to another person (eg, when contained in a pamphlet or dispensed generically by a medical practitioner). Thus, the most threatening dementia-related information includes aspects of the illness that are highly negative and refer to one's self.
We adopted an exploratory approach to addressing whether the MNE will be observed among people with dementia. According to the mnemic neglect model, the MNE will emerge in the case of self-threatening (vs non–self-threatening) dementia-related feedback: People with dementia, in an act of self-protection, will recall poorly self-threatening (compared with non–self-threatening) information. Alternatively, it is possible that people with dementia, given the salience of their symptoms and the prevalence of changes in their lifestyle, will be hypervigilant12, 13 toward new and threatening dementia-related information. As such, they will process such information deeply and recall it relatively well: The MNE will be reversed (or at least cancelled out).
We tested a sample of 62 people with dementia. We presented them with 24 dementia-related statements that varied in level of negativity (high vs low). For half of participants, the statements referred to the self (self-referent), whereas for the other half, they referred to a hypothetical gender-neutral person named Chris. (In the rare cases where the participant, a relative, or friend was named Chris, we changed the hypothetical person's name to the gender-neutral name Jo.) We also assessed participants' levels of depression and anxiety. Subsequently, we instructed participants to recall the 24 statements and then recognize them (in comparison with a new set of 24 statements). Evidence for the MNE would be obtained, if participants recalled poorly the threatening (ie, high-negativity, self-referent) statements, controlling for levels of depression and anxiety. As per prior research on the mnemic neglect model,10 we did not expect differences in recognition.
2 METHOD
2.1 Materials
We generated 64 descriptive statements of dementia from material widely available within the United Kingdom (eg, information leaflets published by the Alzheimer's Society and the National Health Service [NHS] Choices website *) and intended to be read by people with dementia. Two hundred eighty staff and students from University of the West of England responded to an online Qualtrics survey (www.qualtrics.com) and made 2 ratings of each statement (1 = not at all, 6 = extremely) according to (1) how diagnostic of dementia it was and (2) the extent to which it reflected serious consequences of dementia for well-being. As responses to the 2 questions were positively correlated (Appendix A), we combined them into an index. This enabled us to select the 12 statements with the highest scores (high negativity) and the 12 statements with the lowest scores (low negativity; Appendix A).
2.2 Participants and design
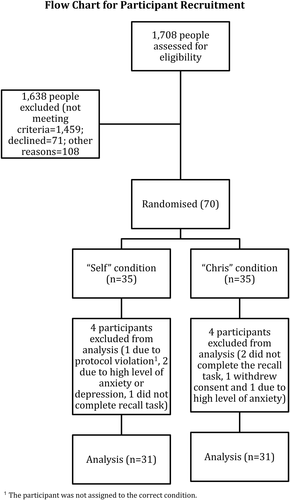
Between February and October 2015, we recruited 70 people with dementia from 3 sites in the South West of England: 2 NHS Mental Health Trusts and 1 independent memory clinic for NHS patients (Table 1, Figure 1). † Participants were eligible to take part, if a diagnosis of probable vascular dementia,14 Alzheimer disease,15 or mixed dementia (based on clinical judgements of the psychiatric or medical teams) had been made within the previous 18 months. ‡ All participants had mild levels of cognitive impairment, as demonstrated by scores on cognitive screening tests completed during the previous 3 months. Depending on the site from which participants were recruited, these were a cut-off score of 1316 on the Montreal Cognitive Assessment,17 a cut-off score of 5018 on the Addenbrooke's Cognitive Examination III,19 and a minimum score of 15 on the Mini-Addenbrooke's Cognitive Examination.20 Participants were also assessed by a member of their clinical team as having the capacity to consent to take part in the study.
|
Self (n = 31) Mean (SD) |
Other (n = 31) Mean (SD) |
|
|---|---|---|
| Age | 80.94 (7.77) | 79.28 (7.01) |
| Cognitive Level | ||
| • MoCA | 18.44 (2.79) | 20.27 (2.39) |
| • ACE-III | 75.67 (8.47) | 78.75 (6.63) |
| • M-ACE | 25.00 (3.16) | 25.80 (1.81) |
| Anxiety (GAI) | 2.36 (3.45) | 2.48 (3.30) |
| Depression (GDS) | 2.65 (1.94) | 2.35 (2.16) |
| Diagnosis | ||
| • Alzheimer | 17 | 24 |
| • Vascular | 8 | 4 |
| • Mixed | 6 | 3 |
| Gender | ||
| • Men | 18 | 12 |
| • Women | 13 | 19 |
| Living status | ||
| • With spouse | 21 | 25 |
| • Alone | 7 | 5 |
| • With family | 3 | 1 |
- Abbreviations: GAI, Geriatric Anxiety Inventory; GDS, Geriatric Depression Scale. Depending on recruitment site, we used the following cognitive screening tasks: the Montreal Cognitive Assessment or MoCA (n = 20), the Addenbrooke's Cognitive Examination III or ACE-III (n = 28), and the Mini-Addenbrooke's Cognitive Examination or M-ACE (n = 14).
We used a 2 (negativity: high, low) × 2 (referent: self, other) mixed design, with the first independent variable being within subjects and the second being between subjects. We randomly assigned participants to the levels of the between-subjects variable, self-referent and other-referent.
2.3 Measures
We measured anxiety with the Geriatric Anxiety Inventory21 (a 20-item self-report questionnaire designed to assess levels of anxiety in an older population) and depression with the 15-item Geriatric Depression Scale.22 People with dementia who had either a significant history of premorbid psychiatric problems or were anxious/depressed (more than 3 standard deviations above the mean and exceeding clinical cut-off points for severe levels of anxiety or depression) were not eligible for inclusion. Figure 1 provides a flow chart of participant recruitment. In the other-referent condition, 3 participants withdrew from the study after allocation, with a fourth participant being excluded due to extremely high levels of anxiety (15 or higher of a maximum score of 20 on the Geriatric Anxiety Inventory) and depression (12 of 15 on the Geriatric Depression Scale). A further 4 participants completed the recall but not the recognition task. In the self-referent condition, one participant withdrew before completing the recall task, with 2 others being withdrawn due to high levels of anxiety and depression. Also, one participant completed the recall but not the recognition task. Finally, a protocol violation by the on-site researcher assistant (ie, the participant was allocated to the other-referent condition, but the case record form suggested that the participant was treated as being in the self-referent condition) led to the removal of this participant's data from analyses. Consequently, we entered data from 62 participants into the recall analysis and from 57 participants into the recognition analysis.
2.4 Procedure
We followed closely (but see below) the standard mnemic neglect protocol validated in prior studies with healthy adults.23, 24 § Participants were tested by research assistants (3 female, 1 male). The research assistants were blinded to participant condition allocation until after the consent procedure. In the self-referent condition, participants were instructed to “Imagine that these descriptions relate to you,” whereas in the other-referent condition, they were instructed to “Imagine that the descriptions relate to a person named Chris.” The wording of the 24 statements varied slightly depending on whether they were self-referent (eg, “The impact of the illness depends on your emotional resilience”) or other-referent (“The impact of the illness depends on Chris' emotional resilience”). The order in which statements were read was identical in the self-referent and other-referent conditions.
To accommodate participants' reduced cognitive capacity, we made 2 changes to the standard mnemic neglect protocol.25, 26 First, instead of presenting participants with a continuous stream of statements, the research assistants read out the statements in 4 sets of 6, with each set containing 3 high-negativity and 3 low-negativity statements. Second, instead of positioning the free recall task after all of the 24 statements had been read out, the research assistants asked participants to recall as many statements as possible at the end of each set of 6 statements.
Next, participants completed a recognition task. The research assistants read aloud 48 statements comprising 24 “old” statements (those that participants had already heard) and 24 “new” statements (ones that participants had not previously heard and which we derived from the list of statements that had initially been rated for negativity). We include the new statements in Appendix B. Participants were then asked whether or not they had heard each statement read to them. Finally, participants were offered a mood repair session (watching a brief comedy video) before finally being debriefed.
3 RESULTS
3.1 Recall
We coded the recalled statements on the basis of a predefined gist criterion, in which we counted statements as correctly recalled if the text conveyed their general meaning.25, 26 For example, the statement “The illness can make X feel depressed” would be counted as correct, if there was a reference to being depressed or sad, or grieving or upset.
We entered the number of statements recalled into a 2 (negativity: high, low) × 2 (referent: self, other) analysis of variance. The mnemic neglect model predicts an interaction between negativity and referent: Recall will be lower when the high-negativity (vs low-negativity) statements refer to the self rather than other. Indeed, this interaction was significant (F1,60 = 5.36, P = .024). Participants recalled high-negativity statements poorly when these statements referred to them (M = 2.42, SD = 1.43) rather than to Chris (M = 3.26, SD = 1.53; t60 = −2.23, P = .029, d = 0.57). However, participants did not differ in their recall of low-negativity statements referring either to them (M = 1.74, SD = 1.51) or to Chris (M = 1.52, SD = 1.29; t60 = 0.64, P = .53, d = −0.16). The MNE thus emerged among people with dementia for dementia-related statements. Moreover, this interaction remained significant after controlling for (ie, entering in the analyses as covariates) depression (
 = 5.03, P = .029) and anxiety (
= 5.03, P = .029) and anxiety (
 = 5.475, P = .023). Finally, we obtained a significant main effect for negativity (F1,60 = 27.67, P < .001): Overall, participants manifested better recall for high-negativity (M = 2.84, SD = 1.53) than low-negativity (M = 1.63, SD = 1.40) statements. There was no main effect for referent (F1,60 = 1.16, P = .286).
= 5.475, P = .023). Finally, we obtained a significant main effect for negativity (F1,60 = 27.67, P < .001): Overall, participants manifested better recall for high-negativity (M = 2.84, SD = 1.53) than low-negativity (M = 1.63, SD = 1.40) statements. There was no main effect for referent (F1,60 = 1.16, P = .286).
3.2 Intrusion errors
Participants made a total of 36 repetition errors (ie, recalling a statement twice) and valence reversal errors. A valence reversal error was defined as one in which the recalled statement reversed or negated the meaning of the original statement that had been read aloud. For example, instead of the low-negativity, other-referent statement “the illness doesn't mean that Chris has to stop doing the things that they enjoy,” one participant recalled “the illness may interfere with things Chris wants to do.” Similarly, instead of the high-negativity, self-referent statement “your illness is a progressive disease,” another participant recalled “the illness does not mean that I will get progressively worse.” The total combined number of repetition and valence reversal errors amounted to 11.50% of overall recall, approximately double the rate observed among healthy adults in laboratory experiments.24 The unusually high rate of intrusion errors led us to initiate a supplemental analysis that also tests the mnemic neglect model, uniquely so among people with dementia.
If the MNE is in the service of self-protection, then this will be reflected in the type of intrusion errors. Following previous research,27 we categorized such errors as either self-protective (ie, valence reversal of high-negativity statements and repetition of low-negativity statements) or non–self-protective (valence reversal of low-negativity statements and repetition of high-negativity statements). We then compared the proportion of each type of intrusion error that participants made in the 2 referent conditions. We hypothesized that, if intrusion errors act to protect the self, then we would observe more self-protective errors (and fewer non–self-protective error) in the self-referent (than other-referent) condition. There was no significant difference between the self-referent (n = 15, 41.67% of all intrusion errors) and other-referent (n = 21, 58.33% of all intrusion errors) conditions in terms of the overall number of intrusion error,
 = 1.00, P = .317. However, a chi-square analysis yielded a significant association between referent and intrusion error type,
= 1.00, P = .317. However, a chi-square analysis yielded a significant association between referent and intrusion error type,
 = 5.60, P = .018. Participants made a higher number of self-protective (n = 11, 73.33% of self-referent intrusion errors) than non–self-protective (n = 4, 26.67% of self-referent intrusion errors) errors in the self-referent condition but made a lower number of self-protective (n = 7, 33.33% of other-referent intrusion errors) than non–self-protective (n = 14, 66.67% of other-referent intrusion errors) errors in the other-referent condition. This pattern of results reinforces the claim that the MNE is in the service of self-protection among people with dementia.
= 5.60, P = .018. Participants made a higher number of self-protective (n = 11, 73.33% of self-referent intrusion errors) than non–self-protective (n = 4, 26.67% of self-referent intrusion errors) errors in the self-referent condition but made a lower number of self-protective (n = 7, 33.33% of other-referent intrusion errors) than non–self-protective (n = 14, 66.67% of other-referent intrusion errors) errors in the other-referent condition. This pattern of results reinforces the claim that the MNE is in the service of self-protection among people with dementia.
3.3 Recognition
Following prior research,24 we used signal detection theory to analyse the recognition data. To take account for biases in responding, as would occur, for example, if a participant identified all 48 items as having been in the original list of words that was read out, we calculated a discrimination index (d1) by subtracting the ratio of false positives (or false alarms) from the ratio of correct positive responses (or hits). We entered the discrimination index scores into a 2 (high/low negativity) × 2 (self-referent/other-referent) analysis of variance. As expected, the interaction was not significant (F1,54 = 0.47, P = .49). No other effect was significant (Table 2).
|
High Negativity Mean (SD) |
Low Negativity Mean (SD) |
|
|---|---|---|
| Self (n = 30) | 0.18 (0.18) | 0.17 (0.12) |
| Other (n = 27) | 0.19 (0.18) | 0.21 (0.25) |
4 SUMMARY OF RESULTS
The MNE emerged among people with dementia: They manifested selective forgetting for self-threatening (ie, high-negativity, self-referent) statements compared with non–self-threatening (ie, low-negativity, other-referent) statements, regardless of their levels of depression or anxiety. The results pattern is consistent with the argument that the MNE is in the service of self-protection for people who live with dementia. Another result—pertaining to intrusion errors—is also consistent with this argument. Participants in the self-referent (vs other-referent) condition were more likely to reverse the valence of high-negativity statements and to repeat low-negativity statements. Finally, as in prior relevant literature,24 recognition patterns did not differ. Although participants recalled fewer high-negativity statements referring to themselves than Chris, their recognition of these statements was equivalent, thereby indicating that all statements were encoded.
5 CONCLUSIONS
We presented participants with dementia-related statements that varied on negativity. Also, we kept the information content constant among participants while manipulating the referent; that is, some participants were read and recalled information that referred to the self, whereas others were read and recalled identical information that pertained to another person. These methodological strengths are uniquely suited to testing the mnemic neglect model.
The model states that self-threatening (relative to non–self-threatening) information is processed shallowly and recalled poorly,24 a phenomenon labelled the MNE. This phenomenon has been robustly observed among healthy adults. However, it was not clear whether it would be present among persons with dementia. On the one hand, such persons may find highly negative statements about dementia threatening and thus process this information shallowly and recall it poorly. On the other hand, they may be vigilant toward highly negative, dementia-related information and hence process it deeply and recall it well. We conducted the first investigation on the topic to find out.
The results indicated that the MNE occurs among people with dementia. They recalled poorly dementia-related information when it was self-threatening, that is, when it was highly negative and referred to them. However, they recalled dementia-related information relatively well when it was non–self-threatening, that is, when it was low on negativity and referred to another person. This pattern of selective recall aligns with the assertion that the MNE serves to guard the self against threat.24 We obtained additional evidence that participants engaged in information processing that is likely to reduce threat to the self. In particular, they committed more self-protective intrusions (ie, valence reversals of high-negativity statements and repetitions of low-negativity statements) than non–self-protective intrusions (valence reversals of low-negativity statements and repetitions of high-negativity statements). Yet recognition patterns did not differ for self-threatening versus non–self-threatening information, a finding that is consistent with the mnemic neglect model.
Our findings of the MNE for recall, but not recognition, are consistent with the dementia literature,28, 29 which suggests that people living with Alzheimer disease who do not explicitly acknowledge their illness often evince implicit awareness of it.30 In one study, for example, people with early dementia took longer to read dementia-related words than neutral words matched for frequency and syllable length.31 However, although in that study the threat posed by the dementia-related words was indirect, the statements in our study were self-referent and the level of self-threat was manipulated.
It has been suggested that the memory impairments characteristic of dementia result in a failure to update personal information and thus contribute to a “petrified self.”32 In contrast, our findings suggest that self-protection is not only due exclusively to memory impairments caused by neural deficits but is also due to psychosocial processes related to the level of self-threat. Qualitative analyses of the narratives of people living with dementia suggest that, for many, acceptance of the diagnosis poses a dilemma33, 34: confronting their dementia directly at the risk of increased distress or retreating away from it at the risk of losing control. Some people with dementia appear to resolve this dilemma by exploring the more threatening aspects of dementia indirectly, through stories and metaphors.35, 36 This indirect exploration may decrease self-threat in a similar way as the other-referent statements did in our study. Within a clinical context, therefore, the differential recall of self-referent versus other-referent dementia-related statements can be understood as a proxy measure of the acceptance of a dementia diagnosis. As such, our investigation may constitute an alternative way of exploring whether the acceptance of a dementia diagnosis is influenced by psychological mechanisms related to self-protection.
5.1 Study limitations
We derived the ratings of dementia-related statements on self-threat from University of the West of England staff and undergraduate students rather than from people with dementia, because we wanted to avoid the risk of distressing the latter population. Of course, we cannot rule out the possibility that people with dementia might have rated the statements somewhat differently than university staff and students. However, we have reasons to be confident in the validity of the obtained ratings. Firstly, staff and students were familiar with dementia. As our informal observations suggested, many staff members completed the survey because of personal interest in dementia and frequently because their lives had been affected by dementia (due to an association with a relative or friend). Also, students attended dedicated sessions on neurological conditions, including various forms of dementia, given that psychology across the lifespan in prominent throughout the Psychology programme at University of the West of England. Secondly, the results of the study validated the ratings; that is, the statements rated as highly negative were recalled poorly (when coupled with self-reference).
The attrition rate was high relative to mnemic neglect studies with healthy adults. This included 5 participants completing the recall task but withdrawing from the recognition task. One contributory factor may have been the semantic similarities between some of the recall statements and some of the (novel) recognition statements. For example, the recall statement “The illness doesn't mean that X has to stop doing the things that X enjoys” is similar to the novel recognition task statement “With the illness there is still much that X can enjoy in life.” This similarity may have rendered the recognition task difficult and thus discouraged further participation. Again, we are confident in our findings. This attrition was limited to 5 participants, and the null results on recognition mimicked those of results obtained with healthy adults.
5.2 Study implications
Our findings have both clinical and empirical implications. On a clinical level, we selected our statements about dementia from information leaflets that are widely available in the United Kingdom and intended to be read by people who live with dementia. In our study, recall of some statements was improved when they referred to another person than the self. This finding suggests that information in such leaflets will be recalled better when self-threat is reduced, that is, when the statements refer to another person (eg, the general or average other). Additionally, previous research has established that the MNE is cancelled out under various circumstances, such as when the threatening information is relayed by a close friend (rather than a stranger),37 when motivation for self-improvement is strong (rather than weak),38 when the threatening information pertains to aspects of one's self that are modifiable (vs fixed),38 and when the self is bolstered (via self-esteem induction) prior to the delivery of threatening information.25 Extrapolating from these findings, dementia researchers may consider devising situations that are likely to improve the recall of threatening information. For example, nostalgic recall (relative to control) bolsters the self by augmenting psychological resources (eg, self-esteem) in both nonclinical populations39 and people living with dementia.40 Consequently, we expect that, following an induction of nostalgia, participants will be more likely to recall self-referent high-negativity information about dementia. We intend to test this hypothesis in a future study.
In conclusion, our research showed that people living with dementia exhibit selective amnesia for threatening information, that is, highly negative and self-referent information pertaining to their illness. As such, our findings contribute to the understanding of memory processes in people with dementia and, by implication, of psychological mechanisms underlying the acceptance of a diagnosis of dementia. We hope our findings spark additional investigations on the topic.
ACKNOWLEDGEMENTS
We thank the participants in our study. We also thank Lauren Buckley, Aspasia Ftenou, Charlotte Godwin, Tom Ingram, Abbie Jones, Michelle Phillips, and Dani Tingley for their assistance with data collection; India Hart for providing maternity cover of the trial coordinator role; and Sanda Ismail and Bettina Zengel for their input. Last but not least, we recognize the contribution of the 3 Alzheimer's Society monitors: Julia Burton, Louise Gillam, and Andra Houchen.
This research was financially supported by Alzheimer's Society (grant ref: 202, AS-PG-2013-13).
CONFLICT OF INTEREST
None declared.
APPENDIX A
Dementia-related statements (recall task)
| Statement | N | Correlation Between Responses to 2 Questions | Mean of Combined Ratings (SD) |
|---|---|---|---|
| High negativity | |||
| The symptoms that X may experience can include loss of memory | 249 |
rs = 0.44 P < .001 |
5.26 (0.79) |
| X's illness is a progressive disease | 248 |
rs = 0.61 P < .001 |
5.12 (0.94) |
| The illness means that X may forget the names of friends or family | 249 |
rs = 0.38 P < .001 |
5.06 (0.92) |
| As the illness gets worse, so X will increasingly come to rely on others | 254 |
rs = 0.46 P < 0.001 |
5.03 (0.91) |
| The illness means that X's symptoms will tend to become more severe | 267 |
rs = 0.61 P < .001 |
5.02 (0.92) |
| The symptoms that X may experience can include problems with communication | 273 |
rs = 0.54 P < .001 |
4.98 (0.87) |
| The illness may make X feel confused at times | 246 |
rs = 0.48 P < .001 |
4.96 (0.87) |
| The illness can make X feel depressed | 259 |
rs = 0.53 P < .001 |
4.87 (0.97) |
| The illness may make X feel insecure | 249 |
rs = 0.56 P < .001 |
4.87 (0.99) |
| The illness will mean that X cannot always remember things you/they have heard | 260 |
rs = 0.42 P < .001 |
4.83 (0.90) |
| As a result of the illness X may misinterpret the world around you/them | 250 |
rs = 0.52 P < .001 |
4.79 (1.00) |
| As a result of the illness X may have problems reasoning | 261 |
rs = 0.69 P < .001 |
4.77 (1.03) |
| Low negativity | |||
| The illness doesn't mean that X has to stop doing the things that X enjoys | 280 |
rs = 0.11 P = .064 |
3.71 (1.11) |
| People with X's illness can be distracted away from their problems | 246 |
rs = 0.25 P < .001 |
3.64 (1.16) |
| Even with the illness X can be reassured | 249 |
rs = 0.26 P < .001 |
3.60 (1.20) |
| The illness develops when the arteries in X's brain become blocked | 269 |
rs = 0.54 P < .001 |
3.59 (1.48) |
| The illness does not change who you are/X is | 282 |
rs = 0.36 P < .001 |
3.53 (1.54) |
| In the illness proteins can gradually build-up inside X's brain | 250 |
rs = 0.67 P < .001 |
3.52 (1.48) |
| When diagnosed with the illness it helps if X has a high quality of life | 247 |
rs = 0.52 P < .001 |
3.44 (1.43) |
| The illness is caused by a shortage of important chemicals in X's brain | 242 |
rs = 0.59 P < .001 |
3.37 (1.39) |
| With the illness, X will still be able to find answers for yourself/themselves | 252 |
rs = 0.13 P = .040 |
3.33 (1.07) |
| The illness means X will still able to learn to do new activities | 249 |
rs = 0.15 P = .017 |
3.23 (1.10) |
| The impact of the illness depends on X's emotional resilience | 247 |
rs = 0.42 P < .001 |
3.13 (1.29) |
| The illness may make X fidget constantly | 246 |
rs = 0.55 P < .001 |
3.13 (1.27) |
- X refers to either self (ie, “You”) or other (ie, “Chris”).
APPENDIX B
New dementia-related statements (included in recognition task)
| Statement | N | Correlation Between Responses to 2 Questions | Mean of Combined Ratings (SD) |
|---|---|---|---|
| The illness can sometimes quickly get worse for X | 254 |
rs = 0.513 P < .001 |
4.71 (1.05) |
| The chances of X developing the illness increases with age | 267 |
rs = 0.358 P < .001 |
4.61 (1.01) |
| X may forget and carry out the same activity twice | 261 |
rs = 0.411 P < .001 |
4.53 (0.97) |
| The illness may mean that X forgets where X has put something | 248 |
rs = 0.373 P < .001 |
4.50 (1.00) |
| The illness occurs when X's brain is affected by a disease | 281 |
rs = 0.693 P < .001 |
4.48 (1.43) |
| The illness means X may forget and ask the same questions over and over | 259 |
rs = 0.276 P < .001 |
4.47 (0.96) |
| With the illness X will notice that X sometimes lose track of what X is saying | 255 |
rs = 0.506 P < .001 |
4.30 (1.03) |
| The impact of the illness depends on the support available to X | 254 |
rs = 0.569 P < .001 |
4.26 (1.25) |
| X may not notice the early signs of the illness | 248 |
rs = 0.253 P < .001 |
4.22 (1.15) |
| The symptoms of X's illness can vary greatly from one person to another | 251 |
rs = 0.376 P < .001 |
4.22 (1.15) |
| The illness can be caused by very small strokes resulting in X's brain being damaged | 253 |
rs = 0.603 P < .001 |
4.21 (1.42) |
| The illness begins gradually with very minor changes for X | 274 |
rs = 0.176 P = .003 |
4.14 (1.00) |
| The illness may mean that X may wake in the middle of the night and get dressed | 275 |
rs = 0.494 P < .001 |
4.03 (1.17) |
| As a result of the illness X may find it difficult to sleep | 251 |
rs = 0.617 P < .001 |
3.97 (1.23) |
| Someone with X's illness may be restless at night | 248 |
rs = 0.596 P < .001 |
3.97 (1.18) |
| The illness may affect X's body clock so that X wakes up in the night | 250 |
rs = 0.527 P < .001 |
3.96 (1.18) |
| Some people with a similar type of illness to X's benefit from medication | 258 |
rs = 0.316 P < .001 |
3.85 (1.16) |
| Memory aids such as a diary can be very helpful for X | 256 |
rs = 0.307 P < .001 |
3.82 (1.28) |
| Drug treatments may slow down the speed at which X's symptoms get worse | 282 |
rs = 0.283 P < .001 |
3.79 (1.15) |
| Someone with X's illness may feel stressed by too much noise | 248 |
rs = 0.587 P < .001 |
3.79 (1.23) |
| Early symptoms of the illness are often mild for X | 251 |
rs = 0.175 P = .005 |
3.75 (1.09) |
| With the illness X will be able to recall things that happened in the past | 249 |
rs = 0.136 P = .032 |
3.75 (1.18) |
| With the illness there is still much that X can enjoy in life | 281 |
rs = 0.113 P = .059 |
3.71 (1.13) |
| People with X's illness can remain independent for as long as possible | 260 |
rs = 0.041 P < .513 |
3.71 (1.04) |
- X refers to either self (ie, “You”) or other (ie, “Chris”).
REFERENCES
- * http://www.nhs.uk/Conditions/dementia-guide/Pages/dementia-choices.aspx.
- † The trial was granted NHS Research Ethics Committee approval on December 18, 2014 (14/SW/1142), with two major amendments approved subsequently (April 15, 2015, for home visits and November 13, 2015, for recruitment of study 2 participants). The study received approval from the University of the West of England Faculty of Health and Social Sciences ethics committee on February 13, 2015 (HAS/15/02/113).
- ‡ All participants consented to allow access to medical records that included details of recent cognitive assessments.
- § The trial protocol was registered online (Current Controlled Trials ISRCTN30485698).