Psychometric validation of the full Yale food addiction scale for children 2.0 among adolescents from the general population and adolescents with a history of mental disorder
Abstract
Objective
Food addiction is a phenotype characterised by an addiction-like attraction to highly processed foods. Adolescence is a sensitive period for developing addictive disorders. Therefore, a valid measure to assess food addiction in adolescents is needed. Accordingly, the aim of the study was to establish a categorical scoring option for the full version of the Yale Food Addiction Scale for Children 2.0 (YFAS-C 2.0), and to psychometrically validate the full YFAS-C 2.0.
Method
The data stem from the Food Addiction Denmark (FADK) Project. Random samples of 3750 adolescents from the general population aged 13–17 years, and 3529 adolescents with a history mental disorder of the same age were invited to participate in a survey including the full version of the YFAS-C 2.0. A confirmatory factor analysis was carried out and the weighted prevalence of food addiction was estimated.
Results
The confirmatory factor analysis of the YFAS-C 2.0 supported a one-factor model in both samples. The weighted prevalence of food addiction was 5.0% in the general population, and 11.2% in the population with a history of mental disorder.
Conclusions
The full version of the YFAS-C 2.0 is a psychometrically valid measure for assessing clinically significant food addiction in adolescents.
1 INTRODUCTION
The food environment has changed drastically over the course of the past decades, with calorie-dense, highly-processed foods (i.e., foods with refined carbohydrates and/or added fats) becoming increasingly abundant and affordable (Moubarac, 2015). An emerging body of research suggests highly-processed foods are reinforcing and may trigger addictive-like biological (e.g., downregulation of dopamine D2 receptors) and behavioural (e.g., use despite negative consequences) responses (Avena et al., 2008; Davis et al., 2015; Gold & Avena, 2013; Murphy et al., 2014; Schulte et al., 2016, 2017a, 2019). This phenotype is operationalised as ‘food addiction’ and conceptualised as a substance-based addiction to highly-processed foods (Gearhardt et al., 2011). Food addiction is most commonly assessed by the Yale Food Addiction Scale (YFAS), which adapts the Diagnostic and Statistical Manual of Mental Disorders criteria for substance-use disorders to assess indicators of addiction to highly-processed foods (e.g., loss of control, continued use despite consequences, withdrawal) (Gearhardt et al., 2009, 2016).
To the extent that food addiction is a valid clinical construct, adolescence may be a particularly sensitive developmental period to study, given that it is a common time for the onset of eating and some addiction disorders (e.g., nicotine-use disorder) (Nevonen & Broberg, 2000; Schneider et al., 2008). As such, the YFAS have been adapted to assess indicators of food addiction in youths. The first version, the YFAS-C (Gearhardt et al., 2013a), was based on the original YFAS (Gearhardt et al., 2009), which adapted the DSM-IV-TR diagnostic indicators for substance-use disorders. The YFAS-C modified the original YFAS by lowering the reading level and including age-appropriate questions and examples (Gearhardt et al., 2013a). Similar to the YFAS, the YFAS-C can be scored continuously, representing the number of symptoms endorsed at a clinical threshold, or categorically; representing no, mild, moderate and severe clinical significant food addiction (Gearhardt et al., 2013a). In order to reflect the DSM-5 update, the dimensional YFAS-C 2.0 (dYFAS-C 2.0) was created (Schulte & Gearhardt, 2017). In the validation study for the dYFAS-C 2.0 (where the full YFAS-C 2.0 was administered), adolescents reported lower endorsement of the problem-focussed criteria, thus only questions relating to the core behavioural features of addiction (e.g., withdrawal, craving, consuming more than intended) were retained. Therefore, the dYFAS-C 2.0 yields only a dimensional score, representing the sum of all item scores (Schulte & Gearhardt, 2017). This approach was employed to be more sensitive to capturing subclinical problems in healthy adolescents from non-clinical populations, where signs of food addiction may only just be emerging.
- (1)
To validate the full version of the YFAS-C 2.0 psychometrically in two large samples of adolescents living in Denmark; one sample of adolescents from the general population and a second sample of adolescents with a history of a clinically verified mental disorder.
- (2)
To establish a categorical scoring option for the YFAS-C 2.0, parallelling the scoring methods of all other YFAS measures.
- (3)
To estimate the prevalence of food addiction among adolescents from the general Danish population and among adolescents with a history of mental disorder. Differences in food addiction by socioeconomic characteristics—in particular, sex and weight status—were also evaluated.
We hypothesised that the full version of the YFAS-C 2.0 is a psychometric valid measure of food addiction for assessing clinically significant food addiction in adolescents from the general population as well as in adolescents with a history of mental disorder. We also hypothesised food addiction to be more prevalent among adolescents with a history of mental disorder than among adolescents from the general population.
2 MATERIALS AND METHODS
The data for the study stem from the Food Addiction Denmark Project (Horsager et al., 2019), a nationwide survey and register-based cross-sectional study conducted in Denmark in 2018. An in-depth description of the Food Addiction Denmark Project is provided by (Horsager et al., 2019, 2021a, 2021b).
2.1 Participants and procedure
In brief, a total of 3750 adolescents aged 13–17 years were randomly drawn from the Danish Civil Registration System (Schmidt et al., 2014), and 3529 adolescents of the same age were drawn from the Danish Psychiatric Central Research Register (Mors et al., 2011). In the latter group, 625 adolescents were randomly sampled from each of the six major diagnostic categories according to the ICD-10 Classification of Mental and Behavioural Disorders (World Health Organization Geneva, 1993); psychotic disorders (the only exception to the n = 625 rule as there were only 404 adolescents with a psychotic disorder), affective disorders, anxiety disorders, eating disorders, autism spectrum disorders, and attention deficit disorders. To be eligible for inclusion, the adolescents identified in the registers were required to have Danish-born parents and to live with at least one parent. Adolescents who were institutionalised or otherwise in the care of the authorities were ineligible, as were adolescents (families) with a protected address or protected name. The drawn adolescents were invited to participate in the survey via their parents who were contacted via the electronic secure mail system (eBoks) used by Danish public authorities (The Agency for Digitisation M of FD, 2020). The invitation included information on the study purpose, clearly stating that participation was voluntary, and that their consent to participate could be withdrawn at any time. The invitation also included a personal link to the web-based questionnaire, and the adolescents were informed to fill it in themselves.
2.2 Ethics
Access to data from the registers as well as the invitation and study methodology were approved by Statistics Denmark and the Danish Health Data Authority. The project was registered with record number 2008-58-0028 at the Danish Data Protection Agency. After the survey was completed, data from the survey and from the Danish registers were de-identified and stored by Statistics Denmark.
2.3 Measures
The Eating Disorder Examination Questionnaire (EDE-Q): The EDE-Q is a self-reported rating scale which is based on the Eating Disorder Examination clinical interview (Berg et al., 2012), and consists of four subscales; eating, weight, and shape concern, restrained eating, as well as a global score. To our knowledge, the Danish version of the EDE-Q has not been validated. However, the Norwegian version is very well validated (Friborg et al., 2013; Rø et al., 2015), and Norwegian and Danish are mutually intelligible languages. Furthermore, the populations of Norway and Denmark are very similar with regard to sociodemographic factors and ethnicity, which likely entail that the Norwegian validation generalises well to the setting of this study.
The ADHD subscale of the Symptom Checklist-92 (SCL-92): In the present study, the ADHD subscale was used as a measure of impulsivity and attention deficit. The Danish version of the SCL-92, including the ADHD subscale, has shown good psychometric properties (Bech et al., 2014; Carrozzino et al., 2016).
The Alcohol Use Disorder Test (AUDIT): The AUDIT was developed by the World Health Organization (WHO) (Babor et al., 2001). The AUDIT can detect problematic use of alcohol, and is considered to be valid for use in adolescence (Rumpf et al., 2013).
Weight and height: Height and weight were self-reported and used to compute the BMI z-score, taking the common growth according to age and sex into account (World Health Organization Geneva, 2007). The BMI z-score was categorised according to the WHO definitions of underweight/thinness < −2 SD, normal weight −2 SD > +1 SD, overweight +1 SD < +2 SD, and obesity > +2 SD (World Health Organization Geneva, 2007). BMI z-scores > +5.5 and < −4.5 were considered biologically implausible, and we therefore intended to exclude individuals with such values from the analyses. However, all BMI z-scores were within the biologically plausible range.
2.4 The yale food addiction scale for children 2.0
The YFAS-C 2.0 consists of 35 items covering the 11 DSM-5 criteria for substance use disorders: (1) consumption of more than planned, (2) unable to cut down or stop, (3) much time spent, (4) important activities given up, (5) use despite physical/emotional consequences, (6) tolerance, (7) withdrawal, (8) craving, (9) failure in role obligation, (10) use despite interpersonal consequences, and (11) use in physically hazardous situations. Two additional items cover the criterion on distress/impairment (American Psychiatric Association, 2013).
The YFAS-C 2.0 was translated into Danish in accordance with the WHO-guideline for translation of psychometric instruments (Sartorius & Kuyken, 1994). Two Danish bilingual physicians with experience in the field of psychiatry each translated the original English version of the YFAS-C 2.0 into Danish. The two physicians discussed their respective version, for example, wording and discrepancies, and produced one combined translated version of the scale. A bilingual English-speaking translator, who had no knowledge of the original questionnaire, translated the Danish version back into English. The developer of the scale Dr. Ashley N. Gearhardt then approved the back-translated version of the YFAS-C 2.0 ensuring that the content of the translated scales corresponded with the original version.
Establishing threshold cut-offs: Response options on the YFAS reflect the frequency with which each of the 35 items occur. In the adult YFAS 2.0, there are eight frequency response options that are quantitative (e.g., ‘once a month,’ ‘4–6 times a week’). The ability to accurately quantify specific occurrences of a symptom may be more challenging for children, thus, in the YFAS-C 2.0 the response options are five descriptive categories, namely ‘never’, ‘rarely’, ‘sometimes’, ‘very often’, ‘always’. To increase consistency with the adult YFAS 2.0, the clinical thresholds identified for that measure were used to guide the identification of thresholds for the YFAS-C 2.0 based on the descriptive response option that best fit with the quantitative response option (see Supplement S1). For example, for questions on the adult YFAS 2.0 where the threshold for clinical significance was 4-6 times a week, the threshold of ‘always’ on the YFAS-C 2.0 was used. In instances where the translation of the adult YFAS 2.0 quantitative threshold to the YFAS-C 2.0 descriptive threshold was unclear, different versions were evaluated psychometrically in both the general population and in the population of adolescents with a history of mental disorder. For example, the version where the ‘once a week’ threshold in the adult YFAS 2.0 was translated to an answer of ‘sometimes’ (compared to the version where it was translated to ‘very often’) in the YFAS-C 2.0 had better overall fit indexes and stronger convergent validity (see Supplement S2). Thus, that version of the scoring was retained for the YFAS-C 2.0. The instruction sheet for scoring the YFAS for Children 2.0 (YFAS-C 2.0) is found in Supplement S3.
2.5 Data analytic plan
First, the internal consistency was examined for the EDE-Q subscales, the SCL-92 and the AUDIT among the respondents from the general adolescent population and among the adolescents with a history of mental disorder, respectively. Subsequently, before running the remaining statistical analyses, the underlying model assumptions were checked. Specific details on model assumptions are provided for each analysis in the section below. All analyses were conducted using STATA version 16.1. We only included complete responses on the YFAS-C 2.0 in the psychometric validity analyses. For the validity analyses, both the YFAS-C 2.0 and the other scale/sub-scale of interest needed to be complete to be included. The number of included responses therefore differs between analyses (specified in the tables).
Validation of the YFAS-C 2.0: The psychometric validity was tested in accordance with the original work on the YFAS 2.0 (Gearhardt et al., 2013a; Horsager et al., 2020). The validation included an examination of the internal consistency using Kuder-Richardson's alpha (KR-20), and a confirmatory factor analyses (CFA) for a one-factor model (given that all prior versions of the YFAS have a one-factor model (Gearhardt et al., 2009; Gearhardt et al., 2016; Meule & Gearhardt, 2019; Pursey et al., 2014)) based on the calculation of the following fit indices; comparative fit index (CFI), Tucker-Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). In parallel with other validations of versions of the YFAS (Gearhardt et al., 2009, 2016; Meule & Gearhardt, 2019; Pursey et al., 2014), the CFA was conducted using the eleven criteria for substance-use disorders, without the criteria for distress and impairment that are not included in the summary score. Finally, due to the strong relationship between eating pathology and addiction disorders with sex and age, the CFA was rerun after stratifying the two groups (respondents from the general adolescent population sample and from the sample of adolescents with a history of mental disorder, respectively) on sex (female/male) and age (13–15 years/16 to 17 years). The adequacy of the fit-indices was assessed in accordance with (Barrett (2007) with the following thresholds: CFI ≥0.90–0.95, TLI ≥0.90–0.95, RMSEA ≤0.06–0.08, SRMR< 0.08, and KR-20 > 0.80 (Streiner, 2003). Due to the relatively large sample size, the assumption regarding multivariate normality for the CFA analysis was assessed via Q-Q plots only. To account for non-normality, robust maximum likelihood estimation (MLR) was applied to the CFA model (Li, 2016).
The convergent and discriminant validity of the YFAS-C 2.0 was tested by calculating Pearson's correlation coefficient between the YFAS-C 2.0 total scores and measures representing constructs considered to be either convergent or discriminant with food addiction (Aloi et al., 2017; Borisenkov et al., 2018; Erzsébet Magyar et al., 2018; Gearhardt et al., 2009, 2013a, 2016; Granero et al., 2018; Meule et al., 2017a; Meule & Gearhardt, 2019; Pursey et al., 2014; Schulte et al., 2017b) (Horsager et al., 2020, 2021c). For convergent validity, the EDE-Q subscales on eating, weight, and shape concern, as well as the total score and binge eating frequency, were used (Aloi et al., 2017; Meule et al., 2017a). The SCL-92 ADHD subscale was also used as a measure of ADHD symptomatology and impulsivity, which both have shown to correlate with food addiction (Davis et al., 2011; Murphy et al., 2014; VanderBroek-Stice et al., 2017). As has been done in prior studies, discriminant validity was examined by investigating the association between YFAS-C 2.0 scores with problematic alcohol use symptom based on the AUDIT (Nunes-Neto et al., 2017) and EDE-Q restraint eating (Aloi et al., 2017; Gearhardt et al., 2016; Meule et al., 2017a). A Pearson's correlation coefficient (|r|) ≥0.30 was considered a relevant association (Kelley & Preacher, 2012) and the cut-off for statistical significance was set at p < 0.05.
The incremental validity of the YFAS-C 2.0 was examined with multiple hierarchical regression analysis to estimate the variance in BMI z-score for the YFAS 2.0-C score above and beyond binge eating frequency (Gearhardt et al., 2016; Schiestl & Gearhardt, 2018). Binge eating frequency was entered in the first model as the only explanatory variable for BMI and subsequently the YFAS 2.0-C total score was entered to the model (model two) enabling an evaluation of the unique variance in the BMI z-score accounted for each of the two measures.
Estimation of the weighted prevalence of food addiction: We used augmented inverse probability weighting (AIPW) (Cao et al., 2009; Glynn AQuinn, 2010; Rothman et al., 2008) to calculate the weighted prevalence of food addiction accounting for non-respondents. Hence, the AIPW model was used to inflate the weights for respondents who were under-represented (according to their sociodemographic, economic, and health profile) among all respondents. The weights were based on the register variables from the attrition analysis (Horsager et al., 2019) and included: age, sex, parental marital status, parental socioeconomic factors (educational level, occupation status and personal income), urbanisation, region, and data on parental and adolescent medical disease (the Charlson Comorbidity Index), prior psychiatric disorders and prior use of psychotropic medication. In the calculation of the prevalence estimates both complete and partial responses of the YFAS-C 2.0 were included. A partial response to the YFAS 2.0 was defined as having answered a minimum of one question per symptom category, which enabled the scoring of each symptom including the impairment/distress symptom.
Demographic and weight class characteristics in food addiction: The comparison of age, sex and weight class between adolescents with and without food addiction was analysed using descriptive statistics with means and standard deviations (SDs) for age, and relative frequencies for sex and weight class. Comparisons between individuals with and without food addiction were analysed with students simple t-test, Chi2-test, and ANOVA with post hoc comparisons.
3 RESULTS
In total, 559 of the 3750 invitees from the general population and 413 of the 3529 invitees from the population of adolescents with a history of mental disorder completed the full YFAS-C 2.0 questionnaire, corresponding to response rates of 14.9% and 11.7%, respectively. The mean age was 14.8 years (SD = 1.8, Range 13–18) with 55.3% of female sex in the general population. In the population of adolescents with a history of mental disorder, the mean age was 15.5 years (SD = 1.3, Range 13–18), and 63.4% were females. The results of the attrition analyses are available in (Horsager et al., 2021a, 2021b). In summary, compared to the non-respondents, the respondents were more likely to be female, and to have parents with higher education and higher income (both samples). In the general population sample, the parents of the respondents were more likely to be in the labour force than the non-respondents. The parental occupational level did, however, not differ statistically significantly between respondents and non-respondents from the sample of adolescents with a history of mental disorder.
3.1 Internal consistency of the EDE-Q subscales, the SCL-92 and the AUDIT
The Cronbach Alpha was as follows for the EDE-Q subscales; Restrained eating, general adolescent population α = 0.84, adolescents with a history of mental disorder α = 0.88; Eating concern, general adolescent population α = 0.77, adolescents with a history of mental disorder α = 0.80; Shape concern, general adolescent population α = 0.92, adolescents with a history of mental disorder α = 0.94; Weight concern, general adolescent population α = 0.84, adolescents with a history of mental disorder α = 0.89; Global score, general adolescent population α = 0.88, adolescents with a history of mental disorder α = 0.91. For the SCL-92, the Cronbach Alpha was α = 0.78 in the general adolescent population, and α = 0.83 for the adolescents with a history of mental disorder, respectively. For the AUDIT, the Cronbach Alpha was α = 0.83 for both the general adolescent population and for the adolescents with a history of mental disorder.
3.2 Psychometric validation of the YFAS 2.0
Factor structure and internal consistency: The prevalence of endorsed YFAS-C 2.0 symptoms and factor loadings of each symptom are provided in Table 1. Among the respondents from the general adolescent population sample the mean number of endorsed YFAS-C 2.0 symptoms was 1.1 (SD = 1.8); 1.3 (SD = 1.9) for females and 0.9 (SD = 1.7) for males (p = 0.002), respectively. Among the respondents from the sample of adolescents with a history of mental disorder, the numbers of symptoms endorsed were 1.7 (SD = 2.4), and 2.0 (SD = 2.6) for females and 1.1 (SD = 2.1) for males (p < 0.001), respectively. In the general adolescent population sample, the most commonly endorsed YFAS-C 2.0 criteria were ‘use despite physical/emotional consequences’ (16.6%) followed by ‘consumed more than planned’ (15.6%) and ‘withdrawal’ (15.6%). Among the adolescents with a history of mental disorder, the most frequently endorsed were ‘withdrawal’ (23.5%), ‘important activities given up’ (23.2%), and ‘consumed more than planned’ (20.6%). The least endorsed criteria were the same for both populations, namely ‘tolerance’ and ‘failure in role obligation’.
| General population (n = 559) | Population with mental disorder (n = 413) | |||
|---|---|---|---|---|
| Food addiction symptoms (SRAD diagnostic indicators) | Met criterion N (%) | Factor loadings 1-factor model | Met criterion N (%) | Factor loadings 1-factor model |
| Consumed more than planned | 87 (15.6) | 0.45 | 85 (20.6) | 0.51 |
| Unable to cut down or stop | 45 (8.1) | 0.52 | 51 (12.4) | 0.65 |
| Great deal of time spent | 38 (6.8) | 0.29 | 49 (11.9) | 0.45 |
| Important activities given up | 78 (14.0) | 0.47 | 96 (23.2) | 0.63 |
| Use despite physical/emotional consequences | 93 (16.6) | 0.61 | 79 (19.1) | 0.70 |
| Tolerance | 19 (3.4) | 0.54 | 21 (5.1) | 0.57 |
| Withdrawal | 87 (15.6) | 0.48 | 97 (23.5) | 0.58 |
| Craving | 52 (9.3) | 0.57 | 66 (16.0) | 0.65 |
| Failure in role obligation | 27 (4.8) | 0.53 | 27 (6.5) | 0.67 |
| Use despite interpersonal/social consequences | 45 (8.1) | 0.54 | 55 (13.3) | 0.57 |
| Use in physically hazardous situations | 29 (5.2) | 0.53 | 36 (8.7) | 0.49 |
| Impairment or distress | 27 (4.8) | - | 61 (14.8) | - |
Among the respondents from the general adolescent population sample, the confirmatory factor analysis for a single factor model (see Table 1 and Supplement S2) showed factor loadings ranging from 0.29 to 0.61 (all with p-values <0.001), CFI = 0.907, TLI = 0.884, RMSEA = 0.064, and SRMSR = 0.046. The internal consistency measured by Kuder-Richardson alpha (KR-20) was 0.78. Among the respondents from the sample of adolescents with a history of mental disorder, the confirmatory factor analysis for a single factor model showed factor loadings ranging from 0.45 to 0.70 (all with p-values <0.001), CFI = 0.942, TLI = 0.927, RMSEA = 0.063, and SRMSR = 0.043. The internal consistency measured by Kuder-Richardson alpha (KR-20) was 0.85. The factor loadings and fit indices were, with few exceptions, similar when stratifying on sex- and age-group (see results in Supplement S4–S5). The factor loadings tended to be higher and the fit indices to be better for females and the 16–17 year old.
Convergent and Discriminant validity: The correlations demonstrating the convergent and discriminant validity of the YFAS-C 2.0 for each population are provided in Table 2. For both samples, all measures of convergent eating pathology were moderately correlated with the YFAS-C 2.0 total score (r's = 0.44–0.64, all p's < 0.05). For binge eating frequency there was a substantial difference in the correlation coefficient between the general sample (r = 0.38, p < 0.05) and the sample of individuals with a history of mental disorder (r = 0.64, p < 0.05). The ADHD subscale (r = 0.41, p < 0.05 in the general sample and r = 0.42, p < 0.05 in the sample of individuals with a history of mental disorder, respectively) correlated moderately with the YFAS-C 2.0 total score in both populations.
| Population | General | Mental disorder |
|---|---|---|
| YFAS-C 2.0 total score (n) | YFAS-C 2.0 total score (n) | |
| YFAS-C 2.0 total score (n) | 1 (559) | 1 (413) |
| Age (n) | 0.11* (559) | 0.12* (413) |
| ADHD (SCL-92) (n) | 0.41* (526) | 0.42* (386) |
| Restraint eating (EDE-Q) (n) | 0.38* (549) | 0.38* (405) |
| Eating concern (EDE-Q) (n) | 0.47* (517) | 0.49* (367) |
| Shape concern (EDE-Q) (n) | 0.46* (527) | 0.44* (383) |
| Weight concern (EDE-Q) (n) | 0.46* (527) | 0.50* (391) |
| Binge eating frequency (EDE-Q) (n) | 0.38* (535) | 0.64* (399) |
| Eating pathology (global EDE-Q score) (n) | 0.49* (506) | 0.47* (348) |
| BMI z-score (n) | 0.27* (534) | 0.29* (390) |
| Alcohol dependence (AUDIT) (n) | 0.12* (362) | 0.25* (279) |
- Abbreviations: AUDIT, The Alcohol Use Disorder Test; EDE-Q, Eating disorder Examination Questionnaire; SCL-92, The Symptom Checklist-92.
- *Significance level: p < 0.05.
Regarding discriminant validity, restrained eating was the least correlated measure of eating pathology with the YFAS-C 2.0 total score in both populations (r = 0.38, p < 0.05 in both populations), although there was still a significant positive association. Problematic use of alcohol did correlate positively, though weakly, with the YFAS-C 2.0 score (r = 0.12, p < 0.05 in the general sample and r = 0.25, p < 0.05 in the population of adolescents with a history of mental disorder).
Incremental validity: Among the respondents from the general population sample (n = 527), in model one when binge eating frequency was entered as the only explanatory variable for the BMI z-score, it was a statistically significant predictor of the BMI z-score (t = 4.97, β = 0.37 [0.22; 0.51], p < 0.001) explaining 4.5% of the variance in the model (R-squared = 0.0449). When the YFAS-C 2.0 total score was added (model two (n = 527)) the association between binge eating frequency and the BMI z-score weakened (t = 0.79, β = 0.22 [0.06; 0.37], p = 0.006), and the YFAS-C 2.0 total score was more strongly associated with the BMI z-score (t = 4.87, β = 0.13 [0.08; 0.18], p < 0.001), accounting for additional 4.1% of the variance in the model (R-squared = 0.09).
Among the respondents from the sample of adolescents with a history of mental disorder, in model one (n = 387) binge eating was statistically significantly associated with the BMI z-score (t = 3.95, β = 0.26 [0.13; 0.38], p < 0.001) explaining 3.9% of the variance in the model (R-squared = 0.04). In model two (n = 387), binge eating frequency was no longer statistically significantly associated with the BMI z-score (t = 0.40, β = 0.03 [-0.13; 0.20], p = 0.69), but the YFAS-C 2.0 total score was (t = 4.08, β = 0.14 [0.07; 0.21], p < 0.001), accounting for additional 4.0% of the variance in the model (R-squared = 0.08).
3.3 Food addiction prevalence estimate and demographic characteristics
Among the respondents from the general population sample, the crude prevalence of food addiction was 4.8% CI 95% [3.1; 6.4], with a weighted prevalence estimate on 5.0% CI 95% [3.2; 6.9]. Among females the weighted prevalence estimate was 9.1% CI 95% [5.8; 12.4] and in males 1.8% CI 95% [0.2; 3.3], respectively. Among the respondents from the sample of adolescents with a history of mental disorder, the crude prevalence estimate of food addiction was 11.4% CI 95% [8.5; 14.2], with a weighted prevalence estimate of 11.2% CI 95% [8.3; 14.0]. Among females, the weighted prevalence of food addiction was 14.9% CI 95% [10.9; 19.0] and in males it was 5.9% [2.1; 9.7], p = 0.001. In both populations, individuals with food addiction were older compared to those without food addiction (see Table 2).
For both the general population and the population of adolescents with a history of mental disorder, there were statistically significant differences in the crude prevalence of food addiction by weight class (see Table 3). Making post-hoc pairwise comparison of the prevalence of food addiction between adjacent weight classes, a dose-response-like tendency was found for the general population. However, in the population of adolescents with a history of mental disorder, there was only a statistically significant pairwise difference in the prevalence of food addiction between individuals with normal weight and overweight, and between normal weight and obesity, respectively (see Figure 1 for the general population and Figure 2 for the population of adolescents with a history of mental disorder).
| General population | Population with a history of mental disorder | |||||
|---|---|---|---|---|---|---|
| Food addiction | No-food addiction | p-value | Food addiction | No-food addiction | p-value | |
| Age (years)Mean/SD | 15.5 (1.3) | 14.8 (1.4) | 0.011 | 15.8 (1.2) | 15.4 (1.3) | 0.044 |
| Crude prevalence (%) | 4.8 | 95.2 | 11.4 | 88.6 | ||
| Weighted prevalence (%) | 5.0 | 95.0 | 11.2 | 88.8 | ||
| Sex (female) (%) | 86.2 | 53.8 | <0.001 | 84.9 | 59.5 | 0.001 |
| Parental marital status (%) | ||||||
| Married or cohabiting | 69.0 | 79.0 | 50.9 | 72.6 | ||
| Single | 31.1 | 21.1 | 49.1 | 27.4 | ||
| 0.203 | 0.001 | |||||
| Weight status (%)a | ||||||
| Underweight | 0.0 | 4.1 | 4.3 | 6.8 | ||
| Normal weight | 55.2 | 86.7 | 63.8 | 79.0 | ||
| Overweight | 24.1 | 7.3 | 21.3 | 9.8 | ||
| Obese | 20.7 | 1.9 | 10.6 | 4.4 | ||
| <0.001 | 0.021 | |||||
- Note: Comparing individuals with and without food addiction. All tests are performed as Chi2 tests except for the comparison of age between groups where the two-sample t-test was used.
- a Performed as ANOVA.
- BMI z-score categorised according to the WHO; underweight/thinness < −2 SD, normal weight −2 SD > +1 SD, overweight +1 SD < +2 SD, and obese > +2 SD.
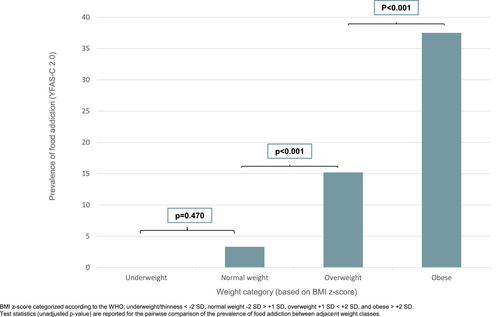
Prevalence of food addiction divided on BMI z-score weight categories, general population.
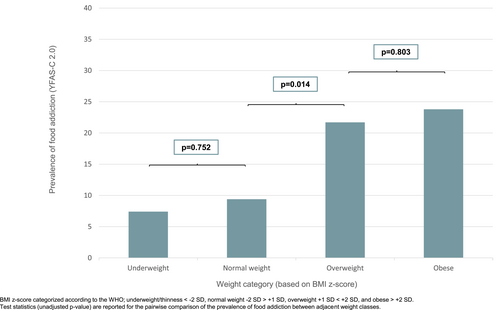
Prevalence of food addiction divided on BMI z-score weight categories, in a population of adolescents with a history of mental disorder.
4 DISCUSSION
In the present study we psychometrically validated the YFAS-C 2.0 in two large samples of Danish adolescents – one from the general population and one from a population of adolescents with a history of mental disorder and established a categorical scoring option for the scale. In addition, the weighted prevalence of food addiction was estimated in both populations, and sociodemographic characteristics of individuals fulfiling the criteria of food addiction were identified.
4.1 Psychometric validation of the full YFAS-C 2.0
Akin to the adult YFAS 2.0 (Gearhardt et al., 2016), the YFAS-C 2.0 exhibits a one-factor structure and was found to have sound psychometric properties regarding internal consistency and convergent, discriminant, and incremental validity. This was evident in both the general adolescent population and in the population of adolescents with a history of mental disorder, as well as for the sex- and age-group stratified groups. There was a tendency towards higher factor loadings and better fit indices in the population with a history of mental disorder, among females, and in the older age group (16–17 year old), respectively, probably due to the higher prevalence of food addiction in these subgroups (less variance in data). Thus, while the dYFAS-C 2.0 (which provides dimensional scoring) may have utility when the aim is to detect sub-clinical signs of food addiction in adolescents (Schiestl & Gearhardt, 2018), the YFAS-C 2.0 provides a tool to assess both symptoms and clinically significant food addiction in both non-clinical and clinical samples of adolescents.
4.2 Food addiction and other measures of pathology in adolescents
Consistent with prior research in adults and youths (Gearhardt et al., 2016; Horsager et al., 2021a, 2021b; Meule & Gearhardt, 2019; Oliveira et al., 2021; Schiestl & Gearhardt, 2018; Skinner et al., 2021), food addiction was associated with greater eating pathology, including binge eating frequency. Of note, the correlations between food addiction and eating pathology were moderate in strength, which provides evidence that the concept of food addiction and other measures of eating pathology cannot be conflated with one another. Food addiction was also associated with adolescents' BMI z-score above and beyond the frequency of binge eating, explaining approximately 4% additional variance in both study samples. This was highly comparable to the psychometrics of the YFAS 2.0 measure for Danish adults (Horsager et al., 2020).
As hypothesised, food addiction was also positively associated with symptoms of ADHD. The co-occurrence of food addiction and ADHD has been observed in both adult and adolescent samples (Brunault et al., 2019; Meule et al., 2017b; Samela et al., 2021). Individuals with both food addiction and ADHD, compared to either condition alone, may have higher emotional distress (Samela et al., 2021) and/or be more likely to have both elevated attentional (e.g., inability to concentrate) and motor (e.g., acting without thinking) impulsivity (Meule et al., 2017b). Thus, future studies may consider testing whether interventions that target improvements in distress tolerance and attentional and motor inhibitory control may be efficacious for simultaneously improving symptoms of food addiction and ADHD.
In contrast to hypotheses, the constructs selected for discriminant validity, dietary restraint and problematic alcohol use were both modestly positively associated with food addiction. In adults from the United States, food addiction was not positively associated with dietary restraint (Carter et al., 2019; Gearhardt et al., 2009, 2013b, 2016). However, a moderately positive association between food addiction (assessed using the dYFAS-C 2.0) and dietary restraint has previously been reported (Schiestl & Gearhardt, 2018). Thus, it is plausible that there may be developmental differences in the association between food addiction and dietary restraint. Notably, the positive association between food addiction and dietary restraint was modest, and food addiction was more strongly associated with all other measures of eating pathology (e.g., binge eating and eating concern). Further, the modest association between food addiction and problematic alcohol consumption in both adolescent samples may suggest that adolescents prone to addictive-like eating behaviour may have a shared vulnerability towards alcohol-related problems. In agreement with this line of thinking, Mies and colleagues (Mies et al., 2017) found that adolescents with elevated symptoms of addictive-like eating behaviour were also more likely to report increased use of other addictive substances (cigarettes, alcohol, and cannabis). In the present study, however, the association between food addiction and problematic alcohol consumption was not robust enough to cause concern about the YFAS-C 2.0 capturing substance-use disorders generally instead of food addiction specifically.
4.3 Prevalence of food addiction using the YFAS-C 2.0
In the general sample, 5.0% of adolescents met criteria for food addiction on the YFAS-C 2.0, which is lower than the 9.4% of Danish adults who met criteria for food addiction on the YFAS 2.0 (Horsager et al., 2020). These numbers are notable for two key reasons. First, it may be that rates of food addiction increase (or nearly double, based on these estimates) from adolescence to adulthood. Second, a substantial proportion of adolescents appear to already exhibit clinically significant indicators of food addiction. Adolescence is a critical period for the development of addictive disorders due to heightened reward salience, intensified emotional states, and lowered inhibitory control (Gladwin et al., 2011). These findings suggest that it may be prudent to identify addiction-like eating behaviours in adolescents, in order to aid early intervention and potentially prevent symptoms from persisting or worsening in adulthood.
In the sample of Danish adolescents with a history of mental disorder, the prevalence of food addiction was 11.2%, which was over twice the 5.0% rate observed in the sample of adolescents from the general Danish population. These trends parallel recent studies in Danish adults, observing food addiction prevalence rates of 9.4% in the general population and 23.7% among adults with a history of mental disorder (Horsager et al., 2020, 2021c). Thus, individuals with mental disorder may have a greater susceptibility to addictive-like eating behaviour, suggesting that the need for early identification and intervention of addictive-like eating behaviour may be even more pertinent in this high-risk group.
The prevalence of food addiction was higher in female adolescents than males, which is consistent with some (Meule & Gearhardt, 2019; Nunes-Neto et al., 2017; Pursey et al., 2014) but not all (Hauck et al., 2017; Schulte & Gearhardt, 2018) findings in adult samples. Notably, the present finding contrasts a meta-analysis that did not observe sex differences across 18 studies that reported food addiction prevalence using the original YFAS-C (Yekaninejad et al., 2021). It may be that the newly developed YFAS-C 2.0 is more sensitive for detecting sex differences or that the higher rates of food addiction in females may be attributed to specific characteristics of Danish adolescents. Nevertheless, the current study suggests that female adolescents in the Danish population may be at elevated risk of having clinically significant symptoms of food addiction.
4.4 Food addiction and weight status
Within both samples of Danish adolescents, food addiction was generally higher in the overweight and obese weight classes. Individuals who were underweight reported the lowest rates of food addiction and the prevalence rates increased for individuals categorised as having normal weight, overweight, and obesity. Danish adolescents with a history of mental disorder generally had higher rates of food addiction, relative to those in the general sample, when comparing all weight classes. However, among participants with obesity, 23.8% of those with a history of mental disorder and 37.5% of individuals in the general sample met the criteria for food addiction.
4.5 Limitations and future directions
While there were a number of strengths of the current study, including the use of two large samples of adolescents from both the general population and a population of adolescents with a history of mental disorder, there were also limitations to consider. The limitations of the Food Addiction Denmark Project, which provides data for this study are covered thoroughly elsewhere (Horsager et al., 2019). Here, we will focus on the limitations associated specifically with studying food addiction in the current samples. The survey data were cross-sectional, omitting the opportunity to investigate the temporality of the association between the measures collected in the survey. Longitudinal research on food addiction that starts in adolescence or childhood is an important next step. Additionally, the survey response rates were low. However, due to the availability of sociodemographic, socioeconomic, and health-care data on both respondents and non-respondents, we were able to estimate the weighted prevalence of food addiction. Lastly, though the YFAS-C 2.0 aims to be developmentally appropriate for assessing food addiction in both children and adolescents, the solid psychometric properties of the YFAS-C 2.0 found in the present study of adolescents do not necessarily extend to children. Thus, a key future direction is to evaluate the psychometric properties of the YFAS-C 2.0 in children from both general populations and clinical samples. Additionally, a natural and important next step would be to further investigate the measurement invariance of the YFAS-C 2.0 properties across different groups of both children and adolescents, to further ensure the psychometric soundness of the YFAS-C 2.0
5 CONCLUSIONS
This is the first study to validate the full version of the YFAS-C 2.0. The Danish YFAS-C 2.0 showed sound psychometric properties in a general population of adolescents as well as in a population of adolescents with a history of mental disorder. Across both samples, food addiction was more prevalent in females and among adolescents with overweight/obesity. As previously observed in adults, adolescents with a history of mental disorder had increased rates of food addiction compared to those in the general population (11.4% vs. 5.0%, respectively). Pressing next steps to extend the current findings include longitudinal studies to assess the developmental trajectory of the food addiction phenotype.
AUTHOR CONTRIBUTIONS
The study was designed by Christina Horsager, Marlene Briciet Lauritsen and Søren Dinesen Østergaard. The data was analysed by Christina Horsager and Emil Færk. Results were interpreted by Christina Horsager, Erica M. LaFata, Marlene Briciet Lauritsen, Søren Dinesen Østergaard and Ashley N. Gearhardt. The first version of the manuscript was drafted by Christina Horsager and Erica M. LaFata and revised critically for important intellectual content by Emil Færk, Ashley N. Gearhardt, Marlene Briciet Lauritsen and Søren Dinesen Østergaard. The final version of the manuscript was approved by all authors prior to submission.
ACKNOWLEDGEMENTS
This work is supported by grants from the Beckett Foundation (17-0-0822), the A.P Møller Foundation of Medical Science (17-L-0013) and the Heinrich Kopps Grant (all to CH), and a PhD fellowship from Aalborg University Hospital, Psychiatry, all to CH. SDØ is supported by the Novo Nordisk Foundation (grant number: NNF20SA0062874), the Lundbeck Foundation (grant numbers: R358-2020-2341 and R344-2020-1073), the Danish Cancer Society (grant number: R283-A16461), the Central Denmark Region Fund for Strengthening of Health Science (grant number: 1-36-72-4-20), The Danish Agency for Digitisation Investment Fund for New Technologies (grant number 2020–6720), and Independent Research Fund Denmark (grant number: 7016-00048B). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
CONFLICT OF INTEREST STATEMENT
Søren Dinesen Østergaard received the 2020 Lundbeck Foundation Young Investigator Prize. Furthermore, Søren Dinesen Østergaard owns/has owned units of mutual funds with stock tickers DKIGI, IAIMWC and WEKAFKI, and has owned units of exchange traded funds with stock tickers BATE, TRET, QDV5, QDVH, QDVE, SADM, IQQH, USPY, EXH2, 2B76 and EUNL. The remaining authors report no conflicts of interest.
CONSENT TO PARTICIPATE
The adolescents were invited via their parents (legal guardians) to ensure, that the parents were informed on the purpose of the study. This procedure ensured that the parents were able to help decide whether their child should have the opportunity to participate in the survey. Furthermore, the invitees were informed, that survey participation was voluntary and that their consent to participate could be withdrawn at any time.
Open Research
DATA AVAILABILITY STATEMENT
In accordance with Danish legislation, the original (individual-level) data cannot be shared due to its personal sensitive nature.