Outpatient management of prolonged seizures and seizure clusters to prevent progression to a higher-level emergency: Consensus recommendations of an expert working group
The outcomes of the Seizure Termination Project expert consensus have been presented as posters at the 35th International Epilepsy Congress 2023, the 4th International Congress of Mobile Health and Digital Technology in Epilepsy 2023, and the American Epilepsy Society Annual Meeting 2023.
Abstract
Objective
The management of prolonged seizures (PS) and seizure clusters (SC) is impeded by the lack of international, evidence-based guidance. We aimed to develop expert recommendations regarding consensus definitions of PS, SC, and treatment goals to prevent progression to higher-level emergencies such as status epilepticus (SE).
Methods
An expert working group, comprising 12 epileptologists, neurologists, and pharmacologists from Europe and North America, used a modified Delphi consensus methodology to develop and anonymously vote on statements. Consensus was defined as ≥75% voting “Agree”/”Strongly agree.”
Results
All group members strongly agreed that termination of an ongoing seizure in as short a time as possible is the primary goal of rapid and early seizure termination (REST) and that an ideal medication for REST would start to act within 2 min of administration to terminate ongoing seizure activity. Consensus was reached on the terminology defining PS (with proposed thresholds of 5 min for prolonged focal seizures and 2 min for prolonged absence seizures and the convulsive phase of bilateral tonic-clonic seizures) and SC (an abnormal increase in seizure frequency compared with the individual patient's usual seizure pattern). All group members strongly agreed or agreed that patients who have experienced a PS should be offered a REST medication, and all patients who have experienced a SC should be offered an acute cluster treatment (ACT). Further, when prescribing a REST medication or ACT, a seizure action plan should be agreed upon in consultation with the patient and caregiver.
Significance
The expert working group had a high level of agreement on the recommendations for defining and managing PS and SC. These recommendations will complement the existing guidance for the management of acute seizures, with the possibility of treating them earlier to potentially avoid progression to more severe seizures, including SE.
Key points
- Uncontrolled seizures negatively impact patient and caregiver quality of life and increase the risk of status epilepticus and its long-term consequences.
- Our consensus statements support rapid and early seizure termination (REST) as a new paradigm for treating ongoing seizures to prevent higher-level emergencies.
- We propose a new term to describe medications for acute cluster treatment (ACT) used to prevent the next or further seizures in a cluster of seizures.
- To aid in the identification of patients who may benefit from early intervention, we propose clear terminology defining prolonged seizures and seizure clusters.
- Effective early administration of a REST medication or ACT will rely on a viable seizure action plan discussed with the patient and their caregiver.
1 INTRODUCTION
While there have been significant advances in the treatment of epilepsy and, in particular, the expanded number of chronic anti-seizure medications (ASMs), 30%–40% of patients are not seizure-free,1 placing them at risk of a seizure emergency.2 Seizure emergencies occur when self-regulating mechanisms of spontaneous seizure termination fail, resulting in abnormally long seizures or repetitive seizures within minutes to hours.3, 4 Uncontrolled seizures negatively impact patient and caregiver quality of life and increase the risk of injury, seizure recurrence, and progression to status epilepticus (SE), which is associated with a high risk of long-term serious consequences such as neuronal cell death, irreversible brain damage, and mortality.2-11
SE has a widely accepted definition proposed by the International League Against Epilepsy (ILAE), with thresholds of ≥5 min for tonic-clonic convulsions and ≥ 10 min for focal seizures with impaired consciousness.3, 4 SE is a medical emergency that requires treatment with parenteral benzodiazepines and ASMs administered by medically trained professionals, which often necessitates hospitalization for stabilization.3, 12, 13 Seizure clusters (also referred to as acute repetitive seizures) are associated with a negative impact on quality of life and a range of adverse clinical outcomes, including an increased risk of progressing to SE.14-16 While the objective of treatment to delay or prevent the next seizure is generally accepted, optimal management is impeded by the lack of an accepted definition and evidence-based guidelines.6, 17, 18 Seizures that have failed to self-terminate in a typical timeframe but have not yet progressed to SE or a seizure cluster lack both standardized, uniform definitions, and clinical guidance.3 For example, the term “prolonged seizure” is not well defined and is frequently used synonymously with SE, despite the ILAE definition.
Preclinical data and evidence from patients who experience SE suggests that seizure duration is clinically meaningful and that terminating an ongoing seizure as early as possible, ideally prior to hospitalization, could translate into improved clinical outcomes and reduced healthcare resource utilization.8, 19-27 The effective treatment of seizure emergencies prior to hospitalization is hampered by the fact that most patients with epilepsy do not have a seizure action plan in place,28 and often rely on the administration of injected benzodiazepines by emergency personnel. One factor contributing to the low uptake of seizure action plans to date may be the lack of approved and effective benzodiazepine formulations suitable for outpatient use that have a sufficiently rapid onset of action to terminate an ongoing seizure before it progresses to a tonic-clonic phase, or SE, and can be easily administered by patients and caregivers.28, 29
Rapid epileptic seizure termination (REST), with treatment administered in an outpatient setting at or near the time of seizure onset (<5 min), has been recently proposed as a therapeutic goal for ongoing seizures in patients at risk of progressing to a more severe seizure or seizure emergency.3 In this paper, we will explain why we recommend that “REST” should evolve to “rapid and early seizure termination” to more accurately reflect the management goal. While REST medications are not currently available, ongoing advances in the development of rapidly acting treatments mean that interventions with the potential to achieve this goal may become available. The Seizure Termination Project was established to develop expert consensus recommendations for the definition and management of certain prolonged epileptic seizures and clusters in the outpatient setting to prevent progression to a higher-level emergency.
2 METHODS
2.1 The expert working group
The two co-chairs (Jesus Eric Pina-Garza and Eugen Trinka) have expertise in the management of seizure emergencies, experience in previous consensus projects, provide geographical coverage of key regions, and between them cover the management of adult and pediatric epilepsy. Ten additional working group members were identified and selected by the co-chairs based on relevant clinical experience (providing a mix of epileptologists and neurologists specializing in the management of patients with epilepsy) or research expertise (e.g., the pharmacology of epilepsy treatments). The selection process aimed to identify as diverse a working group as possible in terms of gender and ethnicity, with a 50:50 mix of US and European experts providing experience in treating adult and pediatric epilepsy.
2.2 Critical literature review
A critical literature review was conducted to identify relevant publications relating to the characterization of prolonged seizures and seizure clusters, the associated burden to patients, caregivers, and the healthcare system, and current management (Appendix S1). The MEDLINE and Embase databases were searched for human studies published from January 2009 to May 2022 on epidemiology, disease burden, clinical outcomes, and guidelines relating to prolonged seizures and seizure clusters. After removing duplicates and screening for relevancy, 205 priority articles were identified for retrieval and review. Clinical guidelines were reviewed to compare treatment recommendations for prolonged seizures and seizure clusters.12, 13, 30, 31
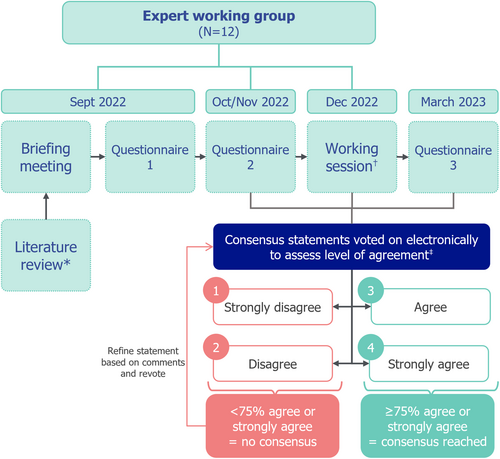
2.3 The modified Delphi approach
The consensus recommendations were developed using a multi-step modified Delphi approach. This method provides a structured, systematic way to formulate consensus recommendations that harness the collective knowledge and experience of the expert working group with iterative rounds of anonymous voting to remove any potential bias that could be introduced by a dominant member(s). The process consisted of three online questionnaires with a hybrid face-to-face/online meeting between questionnaires 2 and 3 (Figure 1). Literature findings were reviewed to identify key management gaps, and the working group completed questionnaire 1 to provide further insights. During subsequent questionnaires and at the meeting, working group members voted on statements and provided commentary on their thought processes with the aim of identifying areas of preferred clinical practice where consensus could be found. All expert group members were blinded to individual questionnaire responses and votes. At each round of voting, experts could select from five options: “strongly agree,” “agree,” “disagree,” “strongly disagree,” or “unable to answer.” Consensus was considered to have been achieved when at least 75% (9/12) of the working group voted “strongly agree” or “agree.” Statements that did not reach consensus or that group members felt could be improved were adapted based on discussion and feedback and then revoted on.
3 RESULTS
3.1 Expert working group
The expert working group all had at least 10 years of clinical and/or research experience in the field of epilepsy (six with at least 30 years of experience) in academic hospitals (n = 9), general/community hospitals (n = 1), research (n = 2), and private practice (n = 1) settings. Among working group members who currently see patients, 7/11 reported seeing more than 100 patients per month, and 8/11 reported that more than 50% of their patients have epilepsy. In questionnaire 1, working group members reported the proportion of their patients with epilepsy who experience “prolonged seizures” (with no specific definition) and “seizure clusters” (with no specific definition) as 0%–25% for 9/11 experts and 26%–50% for 2/11 experts, in both cases.
3.2 Consensus recommendations
The expert working group achieved consensus on a series of recommendations for various aspects of defining and managing seizure emergencies with a high level of agreement. The recommendations and final consensus voting results are shown in Tables 1–4 and in Tables S1-S2.
3.2.1 Terminology describing prolonged seizures and seizure clusters
Consensus was achieved for the definitions of prolonged seizures and seizure clusters given in Table 1 (Figure S1). A threshold of 5 min is proposed for prolonged focal seizures and 2 min for prolonged absence seizures and the convulsive phase of bilateral tonic-clonic seizures, as the majority of such seizures terminate within 2 min.20, 32 The definition of seizure clusters was based on comparison with the patient's usual seizure pattern; however, it was noted that for some patients, seizure clusters represent the “typical” pattern, and these patients would also be diagnosed as having seizure clusters. A specific time-delimited definition of seizure clusters (i.e., number of seizures within 24 h) was rejected as this may prevent the identification of clinically relevant changes in seizure clusters in these patients.
| Expert working group (N = 12) votes, n (%) | Strongly agree | Agree | Disagree | Strongly disagree | Unable to answer |
|---|---|---|---|---|---|
| A prolonged focal seizure is defined as ongoing seizure activity for >5 min but has not yet progressed to focal status epilepticus as per the ILAE definition of > 10 min | 8 (67) | 2 (17) | 2 (17) | 0 | 0 |
| A prolonged generalized absence seizure is defined as ongoing seizure activity for > 2 min but has not yet progressed to absence status epilepticus as per the ILAE definition of 10–15 min | 5 (42) | 5 (42) | 2 (17) | 0 | 0 |
| A prolonged bilateral tonic–clonic seizure is defined as ongoing convulsive seizure activity for >2 min but has not yet progressed to tonic–clonic status epilepticus as per the ILAE definition of >5 min | 8 (67) | 4 (33) | 0 | 0 | 0 |
| Seizure clusters are defined as an abnormal increase in seizure frequency compared with the individual patient's usual seizure pattern | 5 (42) | 5 (42) | 2 (17) | 0 | 0 |
- Abbreviation: ILAE, International League Against Epilepsy.
3.2.2 Treatment definitions and goals
The working group was aligned on the importance of rapidly terminating an ongoing seizure through early administration of medication with a fast onset of action and confirmed that this represents a current unmet need in the management of patients experiencing prolonged seizures. During discussion, it became apparent that the term defined by REST could be improved: first, because “rapid epileptic seizure termination” could be interpreted as occurring at any time following seizure onset, whereas the management goal is to intervene as early as possible upon seizure recognition; and second, the use of epileptic before seizure was considered redundant, supported by a recent ILAE taskforce report stating that “seizure” should always refer to epilepsy.33 Therefore, the term was evolved to “rapid and early seizure termination (REST).”
New terminology was proposed to differentiate treatments used to terminate ongoing seizures (REST medication) from those used to prevent the next or further seizures in a cluster (acute cluster treatment [ACT]), which would include currently available rectal, buccal, and nasal benzodiazepine formulations. The working group recognized that some ACTs could terminate ongoing seizures if administered during the seizure and the seizure lasts sufficiently long for the drug to exert its effect, and that future medications suitable for REST may also be used as ACTs. All members of the working group strongly agreed that termination of an ongoing seizure in as short a time as possible is the primary goal of REST and that an ideal REST medication would start to act within 2 min of administration to terminate the ongoing seizure activity (Table 2). This timeframe derives from the short window of opportunity within which to terminate the seizure before it becomes prolonged or progresses to a tonic-clonic phase, or SE. It should be noted that at the time of writing, there are no approved treatments that are known to meet this target; however, several potential candidates are in development.3
| Expert working group (N = 12) votes, n (%) | Strongly agree | Agree | Disagree | Strongly disagree | Unable to answer |
|---|---|---|---|---|---|
| Rapid and early seizure termination (REST) is a new management paradigm that encompasses the acute treatment of ongoing seizures | 7 (58) | 5 (42) | 0 | 0 | 0 |
| A REST medication is a treatment with the ability to terminate an ongoing seizure | 6 (50) | 4 (33) | 2 (17) | 0 | 0 |
| An acute cluster treatment (ACT), is a medication with the ability to prevent the next or further seizures in a cluster of seizures | 8 (67) | 3 (25) | 1 (8) | 0 | 0 |
| An ideal REST medication would start to act within 2 min of administration to terminate ongoing seizure activity | 12 (100) | 0 | 0 | 0 | 0 |
| Termination of an ongoing seizure in as short a time as possible is the primary goal of REST medication | 12 (100) | 0 | 0 | 0 | 0 |
| Other important goals of REST and ACT are: | |||||
| Prevention of progression to status epilepticus | 11 (92) | 1 (8) | 0 | 0 | 0 |
| Prevention of progression to more severe seizure types | 6 (50) | 6 (50) | 0 | 0 | 0 |
| Reducing the risk of hospitalization | 9 (75) | 3 (25) | 0 | 0 | 0 |
| Outcome-related benefits of REST and ACT for prolonged seizures and seizure clusters include: | |||||
| Reducing the time to reorientation and return to function for the patient | 4 (33) | 7 (58) | 1 (8) | 0 | 0 |
| Reducing the need for emergency services | 9 (75) | 3 (25) | 0 | 0 | 0 |
| Reducing the burden on the caregiver | 6 (50) | 6 (50) | 0 | 0 | 0 |
| A potential benefit of REST medication for prolonged seizures and seizure clusters is reducing the risk of cumulative neuronal damage | 8 (67) | 4 (33) | 0 | 0 | 0 |
- Abbreviations: ACT, acute cluster treatment; REST, rapid and early seizure termination.
All members of the working group strongly agreed or agreed on three important goals of REST and ACT: (1) prevention of progression to status epilepticus; (2) prevention of progression to more severe seizure types; and (3) reducing the risk of hospitalization. Consensus was also reached on the three outcome-related benefits of REST and ACT for prolonged seizures and seizure clusters: (1) reducing the time to reorientation and return to function for the patient; (2) reducing the need for emergency services; and (3) reducing the burden on the caregiver. Reduced risk of cumulative neuronal damage was included as a separate “potential” outcome-related benefit, as several experts noted that there may not be sufficient published data to support this as an outcome in seizures that had not progressed to SE.
3.2.3 Patient groups who should be offered a REST medication or ACT
Consensus statements and levels of agreement on which types of patients should be offered a REST medication or ACT are listed in Table 3. The wording of the statements reflects the level of consensus/evidence supporting the use of treatment in each situation: “should be offered” versus “may be considered for” versus “should be offered with caution.” All members of the working group strongly agreed or agreed that all patients who have experienced a prolonged seizure should be offered a REST medication, and all patients who have experienced a seizure cluster should be offered an ACT.
| Expert working group (N = 12) votes, n (%) | Strongly agree | Agree | Disagree | Strongly disagree | Unable to answer |
|---|---|---|---|---|---|
| All patients who have experienced a prolonged seizure should be offered a REST medication | 10 (83) | 2 (17) | 0 | 0 | 0 |
| All patients who have experienced a seizure cluster should be offered an ACT | 10 (83) | 2 (17) | 0 | 0 | 0 |
| All patients who have experienced status epilepticus should be offered a REST medication | 7 (58) | 4 (33) | 1 (8) | 0 | 0 |
| Patients who have a history of myoclonic or absence seizures that progress to generalized tonic-clonic seizures should be offered REST medication or ACT | 10 (83) | 2 (17) | 0 | 0 | 0 |
| Patients who experience focal seizures should be offered REST medication when they have a history of focal seizures without impaired awareness that progress to focal seizures with impaired awareness | 5 (42) | 7 (58) | 0 | 0 | 0 |
| Patients who experience focal seizures should be offered REST medication when they have a history of focal seizures without impaired awareness that progress to bilateral tonic-clonic seizures | 9 (75) | 2 (17) | 0 | 0 | 1 (8) |
| REST medication may be considered for patients with a history of debilitating post-ictal symptoms (excluding sedation) irrespective of seizure duration | 6 (50) | 5 (42) | 1 (8) | 0 | 0 |
| REST medication may be considered for patients when an ASM is being reduced or discontinued | 4 (33) | 7 (58) | 1 (8) | 0 | 0 |
| REST medication and/or ACT should be offered with caution to patients who are at high risk of severe adverse events, such as respiratory depression | 6 (50) | 6 (50) | 0 | 0 | 0 |
| REST medication and/or ACT should be offered with caution to patients who are at risk of medication abuse or have suspected drug addiction, as this can be mitigated by limited supply | 1 (8) | 9 (75) | 1 (8) | 0 | 1 (8) |
| REST medication and/or ACT should be offered with caution to patients who are taking opioid medication | 2 (17) | 8 (67) | 1 (8) | 0 | 1 (8) |
| REST medication and/or ACT should NOT be offered to patients who are taking chronic benzodiazepine medication for seizure management | 0 | 0 | 6 (50) | 6 (50) | 0 |
- Abbreviations: ACT, acute cluster treatment; ASM, anti-seizure medication; REST, rapid and early seizure termination.
It was noted that patients who have a history of myoclonic or absence seizures that progress to generalized tonic-clonic seizures may require both a REST medication and an ACT if these patients also have a history of seizure clusters. The recommendations represent an ideal scenario; in some cases, patients may live alone, so administration of a REST medication may not be possible during a phase of a seizure with impaired consciousness. Consensus was reached regarding offering a REST medication to all patients who have experienced SE (regardless of convulsive history).
The level of consensus was less strong regarding patients with a history of debilitating post-ictal symptoms and patients who are reducing or discontinuing ASM. Further research is needed to confirm the benefits of rapid seizure termination in reducing the impact of serious post-ictal symptoms. This recommendation specifically excludes cases of sedation as a post-ictal symptom, which could be either improved or worsened by the use of a REST medication. REST medication for patients whose ASM is being reduced or discontinued should be considered on a case-by-case basis, following initial concern from EU experts that this may lead to inappropriate use and over-prescription. The statement that “REST medication or ACT should NOT be offered to patients who are taking chronic benzodiazepine medication for seizure management” was rejected as this would exclude many patients who could benefit from REST medication or ACT. The combination of such medication with chronic benzodiazepine should be individualized based on dosing and other factors. This is supported by clinical study data showing a similar safety and efficacy profile for diazepam nasal spray in patients with and without concomitant benzodiazepine use.34
3.2.4 Advice to patients and caregivers on when to use a REST medication or ACT
Consensus statements and levels of agreement on advice to patients and caregivers on when to use REST medication or ACT are listed in Table 4. These recommendations will need to be given in the context of the proposed definitions for prolonged seizures and seizure clusters described above. All members of the working group agreed that when prescribing a REST medication or ACT, a seizure action plan should be agreed upon in consultation with the patient and their caregiver. For patients with a history of more than one prolonged seizure with a recognizable pattern of onset, the ideal scenario would be to administer a REST medication as early as possible, before the seizure becomes prolonged (Figure S2). Patients with a history of prolonged bilateral tonic-clonic seizures should also receive a REST medication as early as possible due to the severity of this seizure type. In the case of bilateral tonic-clonic seizures without a history of prolonged seizures, early recognition will not be possible; in this case, REST medication should be given after 2 min of convulsive activity when feasible. For patients who experience seizure clusters, consideration of a REST medication or ACT should be based on a clearly recognized pattern of seizure clusters with treatment administered as soon as the pattern is recognized (Figure S3). In patients who have seizure clusters as their main seizure pattern, treatment should be considered at the onset of the first seizure with the aim of preventing progression to a seizure cluster.
| Expert working group (N = 12) votes, n (%) | Strongly agree | Agree | Disagree | Strongly disagree | Unable to answer |
|---|---|---|---|---|---|
| When prescribing a REST medication or ACT, a seizure action plan should be agreed upon in consultation with the patient and caregiver | 10 (83) | 2 (17) | 0 | 0 | 0 |
| Patients with a history of stereotypical prolonged seizures (or their caregivers) are generally able to recognize onset of a prolonged seizure by an individual set of signs or symptoms | 6 (50) | 5 (42) | 0 | 0 | 1 (8) |
| Patients with a history of prolonged seizures of any type who have a recognizable pattern of onset should be advised to administer REST medication as early as possible | 8 (67) | 3 (25) | 1 (8) | 0 | 0 |
| Patients with a history of prolonged seizures of any type should be advised to administer REST medication as soon as the seizure becomes abnormally prolonged based on that patient's seizure pattern | 7 (58) | 4 (33) | 1 (8) | 0 | 0 |
| Patients with a history of prolonged bilateral tonic-clonic seizures should receive a REST medication as early as possible | 7 (58) | 5 (42) | 0 | 0 | 0 |
| When feasible, patients having a bilateral tonic-clonic seizure should receive a REST medication after 2 min of convulsive activity | 3 (25) | 7 (58) | 1 (8) | 0 | 1 (8) |
| Patients with a history of seizure clusters should be advised to administer REST medication and/or ACT when their pattern of onset has been recognized, according to their individual seizure history/pattern | 9 (75) | 3 (25) | 0 | 0 | 0 |
| In patients who have seizure clusters as their main seizure pattern, REST medication, and/or ACT should be considered at onset of the first seizure | 5 (42) | 7 (58) | 0 | 0 | 0 |
- Abbreviations: ACT, acute cluster treatment; REST, rapid and early seizure termination.
3.2.5 Additional recommendations
There was a high level of agreement on consensus recommendations for considerations when prescribing a REST medication or ACT, barriers to management, and the burden associated with seizure emergencies (Tables S1-S2). The working group members felt that the main consideration when prescribing a REST medication would be safety and/or tolerability, with the risk of drug–drug interactions representing a lesser priority.
4 DISCUSSION
This working group brought together a diverse panel of experts in the field of epilepsy from across Europe and the United States to develop definitions of prolonged seizures and seizure clusters and treatment recommendations to terminate an ongoing seizure or prevent the next or further seizures in a cluster. With the definitions of prolonged seizures and seizure clusters as seizure events that could benefit from early intervention, new terminologies are needed to clearly distinguish between treatments for terminating ongoing seizures versus treatments intended to prevent subsequent seizures in a cluster. We propose REST medication and ACT, respectively, to replace the previously used “rescue treatment” with more specific terms that describe the aim of the treatment and are likely to be more widely understood. Termination of an ongoing seizure in as short a time as possible is the primary goal of REST medication. The working group came to a consensus that an ideal REST medication would need to start acting within 2 min of administration to terminate seizures before they progressed to a more severe seizure, including SE. Currently available formulations of “rescue medications” that are suitable for administration by patients and their caregivers are not known to achieve this goal because they likely have onsets of effect of 2 min or later.29 Future clinical trials of potential REST medications should focus on time to seizure termination as a primary outcome measure, rather than the number of seizures over a given time period.
While further studies are needed, prolonged seizures, seizure clusters, and status epilepticus may be considered to result from related underlying mechanisms. The significant association between the occurrence of seizure clusters and convulsive status epilepticus found in one study leads the authors to suggest that seizure clusters may indicate a pathophysiology that also predisposes to status epilepticus.35 Another hypothesis is that the occurrence of seizures over time may persistently lower the seizure threshold, leading to both seizure clusters and status epilepticus.36 Based on available evidence, the working group believes that rapid and early seizure termination and the consequent reduction in risk of progression to SE, should lead to clear outcome-related benefits, including reduced use of emergency services, reduced risk of hospitalization and mortality, and increased overall quality of life. Seizure duration is an independent adverse predictor of outcome,3, 5, 6, 8, 19, 20 and a reduction in total time from seizure onset to seizure termination (i.e. time to administration plus time to seizure cessation) correlates with improved outcomes.3, 5, 6, 19 Several studies, in both adult and pediatric patient cohorts, have shown that early treatment of SE, prior to hospital admission, is associated with an increased likelihood of seizure termination, and a decreased risk of prolonged hospitalization, the need for further treatment, and death.22-27, 37 Further research will be needed to clearly demonstrate the benefits of rapid termination of an ongoing seizure with respect to prevention of SE, healthcare resource utilization, and patient/caregiver quality of life. One potential outcome-related benefit that will require further research is a reduction in the risk of cumulative neuronal damage, including the possible worsening of epilepsy.
To facilitate the identification of patient groups who may benefit from REST medication or ACT, we have proposed clear terminology defining different types of prolonged seizures and seizure clusters. Our proposed 2-minute threshold for defining prolonged bilateral tonic-clonic seizures is supported by data from several electroencephalographic telemetry studies showing that the majority of such seizures terminate within 2 min, with the convulsive phase lasting on average 62–74 s.20, 32, 38, 39
The 2-minute threshold for generalized absence seizures was largely based on the varied individual experiences of the experts, given the lack of published data to support the recommendation. The analysis published by Meritam Larsen PM et al. (2022), shortly after the working group session, reported that typical absence seizures rarely have a duration that exceeds 30 s and atypical absence seizures last up to 100 s, suggesting that this threshold could be revised to 1 min.38 On the other hand, the authors acknowledge that the risk of adverse consequences from prolonged absence seizures is very low.
For seizure clusters, it was noted that, for some patients, clusters are their typical pattern. They, therefore, may not experience an increase in their usual pattern but still experience clusters. Although some were in favor of including a timeframe for the seizure cluster definition, it was ultimately agreed that this should not be included in the consensus definition; however, in clinical practice, ≥2 or 3 seizures within 6, 12, or 24 h may be a useful threshold when considering if a patient requires ACT, and the number of seizures within the same timeframe may be useful for quantifying treatment outcomes. In addition to seizure frequency, it may also be important to consider the inter-seizure interval when assessing a patient's risk of progressing to SE. A recent study found that in SE, the interval between seizures was less than 120 s. This suggests there may be an inter-seizure interval below which the development of SE is more likely, although further studies are needed to determine this.40
We aimed not to over complicate the statements regarding who should be offered treatment, since this could lead to confusion and possible underuse. Thus, the first recommendations are that all patients who have experienced a prolonged seizure should be offered a REST medication, and all patients who have experienced a seizure cluster should be offered an ACT. While there is limited evidence showing that experiencing a first prolonged seizure or seizure cluster increases a patient's risk of a similar subsequent event, offering REST or ACT medication would provide a degree of reassurance, reducing seizure worry. In the case that a pattern of prolonged seizure or seizure cluster does not emerge, the medication can be withdrawn. In many cases, the appropriate use of REST medication and ACT will be driven by a clear understanding of each patient's seizure history.
There is an ongoing discussion around the use of REST medication in patients with serious post-ictal symptoms. Most patients with seizures will experience some form of post-ictal symptoms, including confusion, fear, exhaustion, headache, emotional reactivity, memory problems, and behavioral changes that can last for some time.41-44 The most dramatic after effect of seizures is probably postictal psychosis, which is reported to occur in around 2% of patients with epilepsy,42 and which the ILAE suggests should be treated with benzodiazepines and early administration of anti-psychotic medication.45 The construction of clear recommendations for treatment during the post-ictal phase is complicated by the fact that post-ictal symptoms can be difficult to distinguish from ictal symptoms. In some patients, ictal activity continues, often in an occult fashion, as a type of nonconvulsive status epilepticus.46 Furthermore, the severity and duration of post-ictal symptoms are not necessarily dependent on the duration of the seizure; in this case, recommending REST medication based on a history of prolonged post-ictal symptoms irrespective of the duration of the seizure may be too broad. The recommendation specifies that REST medication “may be offered” to those with a history of “debilitating” post-ictal symptoms; however, further research is needed to confirm the benefits of rapid seizure termination in reducing the impact of debilitating post-ictal symptoms.
The recommendation of offering a REST medication for patients whose ASM regime is being simplified or discontinued generated debate before consensus was reached. While there may be a risk that such a broad recommendation could lead to overuse of REST medication, it was felt that the availability of a rapidly effective treatment could provide a sense of security for patients who feel worried/anxious about coming off chronic ASM. This clinical scenario should be considered on a case-by-case basis. Research investigating the potential benefits of a REST medication in reducing the seizure duration in patients reducing or discontinuing their ASM would be of value to further inform this recommendation.
Available ACTs and investigational REST medications are generally based on benzodiazepine formulations delivered via various routes of administration.3, 5, 29 As such, patients can experience adverse events related to both the drug (typically somnolence, sedation, and drowsiness) and the route (e.g. injection site pain, nasal discomfort, and abnormal taste).5, 29 While benzodiazepines can lead to respiratory depression when administered in high doses and dependence through misuse or long-term intake,29 the controlled dose delivered by drug–device combinations may mitigate against these risks.
For patients and their caregivers, these recommendations will represent a major change in the way they view the management of seizures and will require careful explanation and education. In most cases, patients without a history of prolonged seizure do not receive emergency medication within 5 min of seizure onset since even a seizure meeting the definition of prolonged would be over before currently available treatments would likely have their onset of effect.29 The earlier treatment proposed in our recommendations should be presented as an ideal scenario, with acceptance that this may not always be possible in real-world settings.
Effective early administration of a REST medication or ACT will rely on the prior establishment of a viable seizure action plan discussed with and clearly explained to the patient and their caregiver.16 Currently, most adult patients with epilepsy do not have a seizure action plan in place, with only 30% of patients (n = 259) with seizure clusters reporting having one in place in a survey conducted in the United States.28, 47 However, support for the provision of seizure action plans is increasing, and electronic customizable templates are available to help establish a standardized and widespread approach to developing seizure action plans for all patients with epilepsy.16, 28 Other potential barriers to the effective implementation of our recommendations may include a lack of awareness of future REST medications and ACTs as they become available, a lack of adequate insurance coverage, and a lack of clear legal frameworks covering liability for the administration of medications in community settings (e.g., schools).48
This consensus report has some limitations. The working group was selected by the co-chairs based on their evaluation of experience and expertise and could have been subject to some selection bias; however, the group aimed to include both pediatric and adult experts and to have representatives from a broad international community. Similarly, there is a possibility of bias in the selection of topics for research and discussion by the co-chairs and the formulation of survey questions to address these topics. Nevertheless, this working group believes that the recommendations proposed herein will complement the existing guidance for SE, providing a robust framework for further development of clear definitions and recommendations supporting the possibility of treating earlier to rapidly terminate ongoing seizures and avoid progression to SE and the associated consequences such as use of emergency services, brain damage, long-term hospitalization, and mortality.4, 7, 9, 49 These recommendations will require ongoing adaptation as new data and new treatments become available.
5 CONCLUSIONS
Lack of clarity regarding the ideal timing of intervention is an important barrier to the effective use of seizure termination and prevention treatment. The consensus statements proposed here should provide a clearer picture for clinicians, patients, and caregivers, and facilitate the establishment of REST as a new paradigm for the management of acute, ongoing seizures. The availability of REST medications supported by adequately controlled clinical trials is needed to accomplish this goal.
AUTHOR CONTRIBUTIONS
Jesus Eric Pina-Garza and Eugen Trinka conceptualized and designed the consensus methodology and supervised data collection. All authors were involved in the analysis and interpretation of the literature review, contributed to the voting data, and reviewed and critically revised the manuscript. All authors approved the final manuscript for submission.
ACKNOWLEDGMENTS
Medical writing and administrative support were provided by Nick Gibbs BSc and Sean McAteer PhD at Ogilvy Health UK.
FUNDING INFORMATION
The Seizure Termination Project is funded by UCB Pharma. Project management, data collation, and editorial assistance, provided by Ogilvy Health UK, were funded by UCB Pharma. UCB Pharma reviewed the outputs of the project for scientific accuracy but was not directly involved in any stage of the formulation of recommendations and was blinded to all stages of expert working group voting.
CONFLICT OF INTEREST STATEMENT
All authors received honoraria from UCB Pharma for participating in the Seizure Termination Project. Jesus Eric Pina-Garza has received book royalties from Elsevier; received consulting fees as an advisor to Eisai, Jazz Pharmaceuticals, Marinus, Neurelis, SK Life Science, UCB Pharma, and Zogenix; and received payment or honoraria for speaker bureaus for Eisai, Jazz Pharmaceuticals, Marinus, Neurelis, SK Life Science, UCB Pharma, and Zogenix. Michael Chez has received honoraria as a consultant and speaker for Marinus, UCB Pharma; as a speaker for Catalyst and Neurelis; and as an advisory board member for SK Life Science. James Cloyd has received consulting fees from Neurelis, Solievo, UCB Pharma, and West Therapeutics; royalty payments through the University of Minnesota from Ligand; and research funding through the University of Minnesota from PrevEp. Lawrence Hirsch has received consultation fees for advising from Accure, Ceribell, Eisai, Gilead, Marinus, Neurelis, Neuropace, Rafa Laboratories, UCB Pharma & Vial Health Technology; Royalties from Wolters-Kluwer for authoring chapters for UpToDate-Neurology, and from Wiley for co-authoring the book “Atlas of EEG in Critical Care,” 1st and 2nd editions; and honoraria for speaking from Neuropace, Natus, and UCB Pharma. Reetta Kälviäinen reports personal fees from Angelini Pharma, Lundbeck, Marinus, Orion Pharma, Eisai, UCB Pharma, OmaMedical, Takeda, and Jazz Pharmaceuticals; her institution received grants from the European Union, the Academy of Finland, Finnish Government Research Funding, the Saastamoinen Foundation, the Vaajasalo Foundation, and the Jane and Aatos Erkko Foundation. Pavel Klein has served as a consultant, advisory board member, or speaker for Abbott, Angelini, Aquestive, Arvelle Therapeutics, Aucta Pharmaceuticals, Dr. Reddy's, Eisai, Jazz Pharmaceuticals, Neurelis, Neurona, SK Life Science, Sunovion, UCB Pharma, UNEEG, UniQure, is a member of the Medical Advisory Board of Stratus and of the Scientific Advisory Board of OB Pharma, is the CEO of PrevEp, Inc., and has received research support from CURE/Department of Defense and from the NIH/SBIR. Lieven Lagae has received grants, and is a consultant and/or speaker for Zogenix (now a part of UCB Pharma), LivaNova, UCB Pharma, Shire, Eisai, Novartis, Takeda/Ovid, NEL, and Epihunter en. Raman Sankar has received grants or contracts from DoD and NINDS; has received book royalties from Cambridge University Press and Demos; has received consulting fees from Aquestive, Eisai, and UCB Pharma; has received payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Aquestive, BioMarin, Jazz Pharmaceuticals, Neurelis, SK Life Science, UCB Pharma, and Zogenix; and has participated on a Data Safety Monitoring Board for Takeda. Nicola Specchio has served on scientific advisory boards for GW Pharma, BioMarin, Arvelle, Marinus, and Takeda; has received speaker honoraria from Arvelle, Jazz Pharmaceuticals, Biocodex, UCB Pharma, Zogenix, Takeda, Eisai, Biomarin, Livanova, Sanofi; and has served as an investigator for Zogenix, Marinus, Biomarin, UCB Pharma, Roche, Takeda, GRIN Therapeutics, Jazz Pharmaceuticals, and Livanova. Adam Strzelczyk received personal fees and grants from Angelini Pharma, Biocodex, Desitin Arzneimittel, Eisai, Jazz (GW) Pharmaceuticals, Marinus Pharma, Precisis, Takeda, UCB Pharma (Zogenix), and UNEEG medical. Manuel Toledo declares consulting honoraria and research fundings from Arvelle, Angelini, UCB Pharma, Eisai Inc., Bial, Takeda, Jazz Pharma, GW Pharmaceuticals, Esteve, Neuraxpharm, and Neuroelectrics. Eugen Trinka reports paid consultancy from Arvelle, Argenx, Angelini, Clexio, UCB Pharma, Eisai, Epilog, Bial, Medtronic, Everpharma, Biogen, Biocodex, Takeda, Jazz, Liva-Nova, Newbridge, Sunovion, GW Pharmaceuticals/Jazz, and Marinus; Research funding (directly or to an institution) from GSK, Biogen, Eisai, Novartis, Red Bull, Bayer, and UCB Pharma; Speaker's honoraria from Arvelle, Angelini, GSK, GW Pharmaceuticals, Biocodex, Böhringer Ingelheim, Eisai, Epilog, Bial, Everpharma, UCB Pharma, Liva-Nova, Newbridge, Hikma, Novartis, and Sanofi. He is CEO of Neuroconsult Ges.m.b.H. Grants from the Austrian Science Fund (FWF), the Österreichische Nationalbank, and the European Union.
REFERENCES
Test yourself
-
According to the expert consensus recommendations, what threshold of ongoing seizure activity defines it as being prolonged for the three different seizure types?
-
Focal seizures: 10 min
Absence seizures: 5 min
Convulsive phase of bilateral tonic-clonic seizures: 5 min
-
Focal seizures: 5 min
Absence seizures: 2 min
Convulsive phase of bilateral tonic-clonic seizures: 2 min
-
Focal seizures: 5 min
Absence seizures: 10 min
Convulsive phase of bilateral tonic-clonic seizures: 2 min
-
Focal seizures: 5 min
Absence seizures: 10 min
Convulsive phase of bilateral tonic-clonic seizures: 5 min
-
-
What term has been proposed to describe a medication that can rapidly terminate an ongoing seizure?
- Rapid and early seizure termination (REST) medication
- Acute seizure treatment (AST)
- Emergency seizure termination (EST) medication
- Emergency rescue medication (ERM)
-
What term has been proposed to describe a medication with the ability to prevent the next or further seizures in a cluster of seizures?
- Rapid and early seizure termination (REST) medication
- Rapid cluster treatment (RCT)
- Acute cluster treatment (ACT)
- Emergency seizure termination (EST) medication
Answers may be found in the supporting information.