Postprocedural development of left upper extremity mass
Meetings: Presented at VCOM- Carolinas Research Day as a poster presentation in Spring 2021
1 PATIENT PRESENTATION
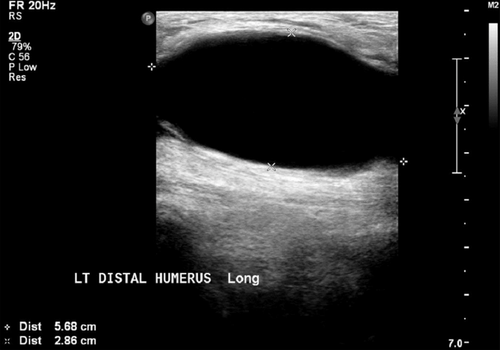
An 89-year-old male presented to the emergency department for a lump near his antecubital fossa of his left upper extremity. He recently underwent percutaneous left brachial artery access for splenic artery embolization. Post procedure, he developed swelling around the intravenous site and numbness in the fingers of his left hand with decreased grip strength. On physical examination, there was a mass over the left medial epicondylar region with no erythema, edema, tenderness, or warmth (Figure 1). The lesion was not pulsatile. He had associated decrease pincher grasp of his left upper extremity. An ultrasound of the mass was ordered.

2 DIAGNOSIS
2.1 Pseudoaneurysm
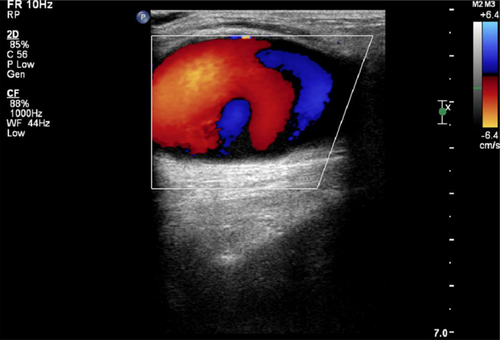
Ultrasound of the left upper extremity showed an anechoic structure measuring 7.0 × 2.6 cm (Figure 2). Doppler of the structure revealed a swirling color flow and a small neck feeding the vessel near the medial left distal humerus soft tissue. This bidirectional blood flow creates a “Yin-Yang” appearance, which is a classic ultrasound finding for pseudoaneurysms (Figure 3). Pseudoaneurysms most commonly occur as complications of endovascular procedures 0.5% to 2% of the time.1 They are a known complication of endovascular procedures with the femoral artery, which is the most common arterial access.2 However, the arteries in the upper extremity are becoming more favored for procedural use because of fewer hospital complications as compared to femoral access.3 Recognition of a pseudoaneurysm is imperative because of the risk of rupture, hemorrhage, and potential distal ischemia due to reduced blood flow.1, 4 Some pseudoaneurysms with diameters of less than 1.8 cm may spontaneously resolve.5, 6 For those larger in diameter, thrombin injection is the preferred treatment.5, 6 Ultrasound guided direct compression may also be used to resolve pseudoaneurysms non-invasively.5 Surgical repair is reserved for those patients who fail either the thrombin injection or direct compression.7 This patient was ultimately referred to vascular surgery for repair.