Initial prehospital Rapid Emergency Medicine Score (REMS) to predict outcomes for COVID-19 patients
Supervising Editor: Karl Sporer, MD.
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Abstract
Objective
The Rapid Emergency Medicine Score (REMS) has not been widely studied for use in predicting outcomes of COVID-19 patients encountered in the prehospital setting. This study aimed to determine whether the first prehospital REMS could predict emergency department and hospital dispositions for COVID-19 patients transported by emergency medical services.
Methods
This retrospective study used linked prehospital and hospital records from the ESO Data Collaborative for all 911-initiated transports of patients with hospital COVID-19 diagnoses from July 1 to December 31, 2020. We calculated REMS with the first recorded prehospital values for each component. We calculated area under the receiver operating curve (AUROC) for emergency department (ED) mortality, ED discharge, hospital mortality, and hospital length of stay (LOS). We determined optimal REMS cut-points using test characteristic curves.
Results
Among 13,830 included COVID-19 patients, median REMS was 6 (interquartile range [IQR]: 5-9). ED mortality was <1% (n = 80). REMS ≥9 predicted ED death (AUROC 0.79). One-quarter of patients (n = 3,419) were discharged from the ED with an optimal REMS cut-point of ≤5 (AUROC 0.72). Eighteen percent (n = 1,742) of admitted patients died. REMS ≥8 optimally predicted hospital mortality (AUROC 0.72). Median hospital LOS was 8.3 days (IQR: 4.1-14.8 days). REMS ≥7 predicted hospitalizations ≥3 days (AUROC 0.62).
Conclusion
Initial prehospital REMS was modestly predictive of ED and hospital dispositions for patients with COVID-19. Prediction was stronger for outcomes more proximate to the first set of emergency medical services (EMS) vital signs. These findings highlight the potential value of first prehospital REMS for risk stratification of individual patients and system surveillance for resource planning related to COVID-19.
1 INTRODUCTION
1.1 Background
Periodic surges of COVID-19 patients seeking care in the hospital environment overwhelm systems, reduce the availability of resources for treatment of non-COVID-19 cases, place unpredictable demands on inpatient resources and create increased risk for transmission of the infection to staff or other patients.1, 2 COVID-19 patient acuity has remained fairly consistent with the majority of patients having somewhat mild symptoms, about 25% experiencing hospitalization, and 5%-6% requiring critical care intervention.3 This suggests that a significant proportion of patients seeking care for COVID-19 at the emergency department (ED) may have less severe presentations of the disease that could potentially be evaluated and managed in the community or in an outpatient setting.3-5 Identifying this patient population could reduce the impact of patient surges on ED capacity and inpatient resources.6 Hospital flow and resource management could be greatly enhanced if emergency medical services (EMS) notification included information that could reliably differentiate patients who will likely require admission with a prolonged length of stay (LOS) from those who could safely be discharged after evaluation and managed outside of the hospital setting.
1.2 Importance
Although the pandemic has reduced patient volume in most EDs,7, 8 the percentage of patients requiring admission rapidly doubled or tripled in many hospitals and continues to fluctuate in tandem with the rate of COVID-19 cases in the community.8 EMS data have helped some hospital systems anticipate surges in hospital volume during the pandemic. Increases in requests for EMS services in dispatch centers9 or the number of EMS patients with COVID-19 related symptoms have preceded intensive care unit (ICU) surges by 1-2 weeks.10, 11 Upticks in the prevalence of low pulse oximetry measurements also have shown an ability to predict next-day hospital bed occupancy12 and community COVID-19 load.13 However, none of these strategies facilitate risk stratification of individual patients presenting with COVID-19. Such risk stratification could enable rapid clinical decisions regarding the need for hospital admissions3 and streamline patient flow through the ED. A number of studies have evaluated the value of acuity scores for the general EMS patient population. A recent comparison of the predictive value for hospital mortality of National Early Warning Score 2, Modified Early Warning Score (MEWS), Vitalpac Early Warning Score, Worthing Physiologic Scoring System, Triage Early Warning Score, Prehospital Index, and Rapid Emergency Medicine Score (REMS) modified for trauma found no statistical difference in the ability to predict mortality among the scores.14 The REMS has proven valuable for predicting ED mortality15, 16 and, when measured during initial EMS evaluation, is able to predict ED disposition (discharge, hospital admission, ED death).17
Identification of COVID-19 patients who are unlikely to require inpatient care could also improve hospital resource use and reduce risk of disease transmission. Multiple studies have explored the potential for EMS systems to perform initial screening on suspected COVID-19 patients for the purpose of identifying patients who are stable enough to be managed at home or in outpatient settings.4, 9, 10, 18-20 Recently validated tools that predict COVID-19 prognosis in the hospital 21 and outpatient3 settings use data elements that are not routinely available to EMS crews including hematocrit, white blood count (WBC), chest x-ray, and in-depth past medical history. A recent small study assessed the ability of specific physiologic parameters as well as the Quick Sepsis Related Organ Failure Assessment (qSOFA), CURB-65 (confusion, urea, respiratory rate, blood pressure, and ≥ 65 years of age) and MEWS scores to predict which COVID-19 patients would develop ventilator dependent respiratory failure. Although MEWS provided the best prediction the authors concluded that all scores demonstrated poor discrimination power.22
To date, the authors are unaware of any studies exploring whether the first prehospital REMS can be used to predict which COVID-19 patients require admission to the hospital, which may have a prolonged hospitalization, and which might potentially be safely monitored and cared for outside the hospital.
1.3 Goals of this investigation
This study aimed to determine whether the first prehospital REMS could predict ED mortality, ED discharge, hospital mortality, and hospital LOS for COVID-19 patients transported by EMS.
1.3 The Bottom Line
The Rapid Emergency Medicine Score (REMS) uses vital signs collected in the prehospital environment to predict outcomes. In this study the authors tested the ability of the REMS to predict hospital mortality among prehospital patients ultimately diagnosed with COVID-19. When applied to over 13,000 prehospital patients from across the United States, REMS was modestly predictive of emergency department and hospital dispositions. REMS may potentially play a role in community-wide COVID-19 management.
2 METHODS
2.1 Study design and setting
We conducted a retrospective observational study using de-identified prehospital patient care records from the ESO Data Collaborative (Austin, TX). ESO is one of the largest EMS electronic health record providers in the United States. Compliant with the National EMS Information System, the electronic health record facilitates entry of dispatch, patient demographics, clinical presentation, vital signs, assessments, and interventions performed by the EMS clinician. A subset of EMS agencies use a bidirectional health data exchange software product to link and receive hospital outcome information. Data elements from participating receiving facilities are directly linked back to the EMS record using standard Health Level Seven messaging, including ED and in-patient dispositions and diagnoses.
The Data Collaborative contains all patient care records from EMS agencies who have signed voluntary agreements to contribute their de-identified data for research purposes. Data contained in the collaborative are entered by individual clinicians during the routine course of public safety and healthcare patient encounters. As of January 1, 2020, there were 1322 agencies participating in this collaborative. This dataset includes EMS encounters occurring in all 50 states and the District of Columbia and includes agencies that are fire based, municipal third service, hospital based, and privately owned. The institutional review board at St. David's HealthCare determined that this study qualified as exempt research.
2.2 Selection of subjects
Given the advancements in treatment that led to measurable improvements in mortality for COVID-19 patients admitted between March and July 2020,23 we queried records from July 1 to December 31, 2020 to produce more stable estimates of outcomes including mortality. We included all emergency responses (911 activations) for adult patients (18 years and older) who had a hospital diagnosis of COVID-19 based on International Classification of Diseases, Tenth Revision codes (B97.2, B97.21, B97.29, B34.2, and U07.2). We limited our analysis to COVID-19 diagnoses rather than EMS-suspected COVID-19 in order to directly explore predictive characteristics of the REMS in this unique patient population. We excluded patients in cardiac arrest before EMS arrival. Given that only patients with ED or hospital diagnoses were included, this study inherently excluded all patients who were not transported to a hospital by EMS.
3 MEASUREMENTS
3.1 Rapid Emergency Medicine Score
Scoring for the REMS is calculated by assigning point values to categories of mean arterial pressure, pulse rate, respiratory rate, oxygen saturation, Glasgow Coma Scale, and patient age (Table 1). Total REMS values range from 0 to 26 and higher values are associated with increased mortality.24 We used the first set of prehospital vital signs as entered by the EMS clinician in the REMS calculation, consistent with prior studies of EMS obtained REMS and hospital disposition.17
| Low range | High range | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Vital Signs | |||||||||
| REMS points | +4 | +3 | +2 | +1 | 0 | +1 | +2 | +3 | +4 |
| Mean arterial pressure (mmHg) | <50 | 50–69 | 70–109 | 110–129 | 130-159 | >159 | |||
| Pulse rate (beats/minute) | <40 | 40–54 | 55–69 | 70–109 | 110–139 | 140-179 | >179 | ||
| Respiratory rate (breaths/minute) | <6 | 6–9 | 10–11 | 12–24 | 25–34 | 35-49 | >49 | ||
| Oxygen saturation (%) | <75 | 75–85 | 86–89 | >89 | |||||
| Glasgow Coma Scale | <5 | 5–7 | 8–10 | 11–13 | >13 | ||||
| Age | |||||||||
| REMS points | 0 | +1 | +2 | +3 | +4 | +5 | +6 | ||
| Age category (years) | <45 | 45–54 | 55–64 | 65–74 | >74 | ||||
3.2 Outcome measures
We examined 4 outcome measures: ED mortality, ED discharge, hospital mortality, and hospital LOS.
We created a dichotomous variable for ED mortality by categorizing dispositions of patients who died in the ED versus patients who did not die in the ED (discharged from the ED, admitted, transferred to another facility).
For ED discharge, we created a 2-level variable by grouping all patients discharged from the ED to locations other than hospice versus those who were admitted to the hospital, transferred from the ED to another facility, or discharged to hospice. Patients discharged to hospice were not included in the discharged from ED group because they were likely to be substantially different from discharged patients due to their age (61% > 75) and likelihood of imminent death (54% die within 30 days of admission to hospice).25 We excluded patients who died in the ED from the ED discharge variable, because characteristics of this patient group would likely differ from patients discharged alive or patients who were admitted, transferred, or discharged to hospice.
For hospital mortality, we created categories for patients who died after admission versus patients who were discharged from the hospital. We excluded patients who were transferred to another facility and those who were still patients at the end of the study period as the definitive outcome for the encounter was unknown. We also excluded patients discharged to hospice as this disposition is distinct from other hospital discharge dispositions.
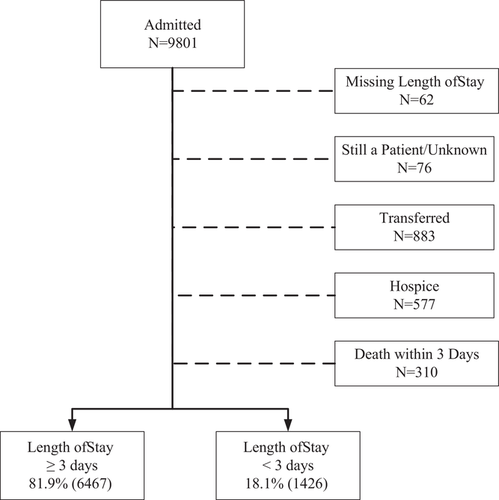
For hospital LOS, we used 3 days as a cut-point based on prior literature. 26 We created a dichotomous variable for admitted patients with a hospital LOS <3 days versus those who had an inpatient LOS of 3 or more days. For LOS analysis, we excluded patients who were transferred to another facility or who were still a patient at the end of the follow-up period because total LOS could not be determined. We also excluded patients who died within 3 days of admission as these patients were likely distinct from patients who were discharged alive within 3 days of admission. Similarly, we excluded patients who were discharged to hospice as being discharged to hospice likely represents a distinct cohort compared with patients with other discharge dispositions.
3.3 Analysis
We calculated prehospital REMS using the first set of vital signs obtained by EMS from the patient care record. We excluded records that were missing 1 or more elements needed to calculate a REMS value. In the descriptive analysis, we summarize continuous variables using median and interquartile range (IQR) and categorical variables with frequencies and percentages.
To determine the overall predictive ability of REMS for each outcome variable, we calculated the area under the receiver operating curve (AUROC) and 95% confidence interval (95% CI). In general, AUROC values between 0.7 and 0.8 are considered acceptable and values greater than 0.8 represent excellent predictive ability.27 We used sensitivity and specificity curves to determine the optimal statistical prediction cut-point for each outcome by examining the intersection of these curves. We used univariable logistic regression models to assess the relationship between the dichotomized REMS variable and each outcome.
4 RESULTS
4.1 Characteristics of study subjects
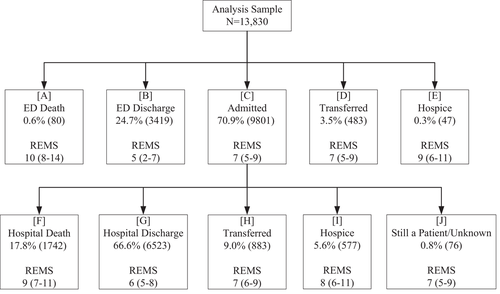
There were 15,261 EMS records with linked hospital data for patients diagnosed with COVID-19 between July 1, 2020 and December 1, 2020, from 326 EMS agencies. We excluded 99 patients with documented out-of-hospital cardiac arrest and 119 patients under the age of 18 years. Of the 15,044 eligible records, 1214 (8%) were missing 1 or more elements needed to calculate REMS, leaving 13,830 patients in the analysis sample (Figure 1). Of eligible EMS encounters, age was missing for 3 (< 0.1%) patients, systolic blood pressure for 171 (1.1%), diastolic blood pressure for 369 (2.5%), respiratory rate for 440 (2.9%), oxygen saturation for 362 (2.4%), and Glasgow Coma Scale score for 296 (1.9%). The median age of all included patients was 71 (IQR: 58–81) and 50% were female. The median first prehospital REMS score was 6 (IQR: 5–9) (Table 2). EMS clinicians selected a primary or secondary impression specifically related to COVID-19 for 46.2% (6391) of patients. Among patients where COVID-19 was not specifically selected by EMS (7439), the most common primary impressions were generalized weakness (14.1%, 1055), acute respiratory distress (12.8%, 950), and shortness of breath (11.1%, 828).

| Analysis Sample N = 13,830 | ED Mortality N = 80 | ED Discharge N = 3419 | Hospital Mortality N = 1742 | LOS ≥3 Days N = 6467 | |
|---|---|---|---|---|---|
| Age, years | |||||
| Median (IQR) | 71 (58–81) | 79 (67.5–88) | 61 (44–76) | 77 (68–85) | 73 (62–82) |
| Sex | |||||
| Female | 50.0% (6909) | 41.3% (33) | 55.3% (1889) | 43.0% (747) | 48.4% (3123) |
| Male | 50.0% (6897) | 58.7% (47) | 44.7% (1524) | 57.0% (992) | 51.6% (3333) |
| US Census region | |||||
| Northeast | 6.5% (880) | 2.5% (2) | 6.0% (201) | 4.5% (78) | 7.6% (483) |
| Midwest | 16.7% (2279) | 16.7% (13) | 14.7% (493) | 24.7% (426) | 16.5% (1051) |
| South | 65.3% (8912) | 75.6% (59) | 65.5% (2196) | 58.9% (1015) | 65.2% (4157) |
| West | 11.5% (1576) | 5.1% (4) | 13.8% (463) | 11.8% (204) | 10.8% (687) |
| US Census urbanicity | |||||
| urbanized area | 82.8% (11,381) | 95.0% (76) | 84.2% (2861) | 82.7% (1432) | 82.8% (768) |
| urban cluster | 5.6% (771) | 1.3% (1) | 5.2% (175) | 5.3% (91) | 5.3% (341) |
| Rural | 11.6% (1590) | 3.7% (3) | 10.6% (360) | 12.0% (208) | 11.9% (768) |
| First prehospital REMS | |||||
| Median (IQR) | 6 (5–9) | 10 (8–14) | 5 (2–7) | 9 (7–11) | 7 (5–9) |
- Abbreviations: IQR, interquartile range; REMS, Rapid Emergency Medicine Score
4.2 Main results
4.2.1 REMS as a predictor of ED mortality
Out of the 13,830 included patients, <1% (80) died in the ED (Figure 2). The median age among those who died in the ED was 79 (IQR: 67.5–88). The median first prehospital REMS among patients who died in the ED was 10 (IQR: 8-14). The AUROC for REMS as a predictor of ED mortality versus ED discharge, hospital admission, or transfer to another facility or hospice was 0.79 (95% CI: 0.74–0.84). A cut-point of 9 or higher was statistically optimal for predicting ED death and resulted in a sensitivity of 72% and specificity of 74% (Table 3). Compared to those with a first prehospital REMS < 9, patients with a REMS of 9 or higher had more than a 7-fold increase in odds of ED death (OR: 7.62, 95% CI: 4.66–12.47).
| Outcome | AUROC | StatisticalCut-Point | Sensitivity | Specificity |
|---|---|---|---|---|
| ED mortality | 0.79 (0.74–0.84) | 9 or higher | 72% | 74% |
| ED discharge | 0.72 (0.71–0.73) | 5 or lower | 58% | 74% |
| Hospital Mortality | 0.72 (0.71–0.73) | 8 or higher | 68% | 63% |
| LOS ≥3 days | 0.62 (0.60–0.63) | 7 or higher | 56% | 60% |
- Abbreviations: AUROC, area under the receiver operating curve; ED, emergency department; LOS, length of stay; REMS, Rapid Emergency Medicine Score.
4.2.2 REMS as a predictor of ED discharge
Overall, 25% (3419) of EMS patients diagnosed with COVID-19 were discharged from the ED, and 71% (9801) were hospitalized; the remaining 4% (610) died in the ED or were transferred (Figure 2). The median first prehospital REMS among discharged patients was 5 (IQR: 2–7). Meanwhile, the median REMS among patients who were admitted to the hospital was 7 (IQR: 5–9). First prehospital REMS demonstrated an AUROC of 0.72 (95% CI: 0.71–0.73) as a predictor of ED discharge versus admission, transfer, or hospice (Table 3). A REMS of 5 or lower demonstrated optimal prediction of ED discharge with a sensitivity of 58% and specificity of 74%. A REMS of 5 or lower was associated with nearly a 4-fold increase in odds of ED discharge (OR: 3.87, 95% CI: 3.57–4.19).
4.2.3 REMS as a predictor of hospital mortality
Out of 9801 admitted EMS patients diagnosed with COVID-19, 18% (1742) died (Figure 2). The median first prehospital REMS among patients who died in the hospital was 9 (IQR: 7-11) compared to a median of 6 (IQR: 5–8) among patients discharged alive from the hospital. AUROC was 0.72 (95% CI: 0.71–0.73) for REMS prediction of hospital death versus hospital discharge (Table 3). Sensitivity and specificity for hospital death were 68% and 63% respectively at an optimal REMS cut-point of 8 or higher. Patients whose initial prehospital REMS was 8 or higher had over 3 times the odds of dying after hospital admission (OR: 3.59, 95% CI: 3.21–4.02).
4.2.4 REMS as a predictor of hospital LOS
Hospital LOS was missing for 6% (62) of admitted patients. The median hospital LOS for admitted patients who died was 8.3 days (IQR: 4.1–14.8 days) compared to 5.2 days (IQR: 3.2–8.5 days) among those who were discharged alive. A total of 310 (18.2%) patients with hospital LOS data died within 3 days of admission. After excluding hospitalized patients who died within 3 days, were transferred or discharged to hospice, or did not have a disposition available by the end of the study period, 82% of patients had a hospital LOS of 3 or more days (6467/7893) (Figure 3). The median first prehospital REMS among patients with hospital LOS less than 3 days was 6 (IQR: 4–8) compared to a median of 7 (IQR: 5–9) among those with a hospital LOS of 3 or more days. First prehospital REMS demonstrated an AUROC of 0.62 (95% CI: 0.60–0.63) for predicting hospital LOS of 3 days or more. The optimal REMS cut-point for this outcome was 7 or higher with a sensitivity of 56% and specificity of 60%. Patients with a first prehospital REMS of 7 or higher had nearly a 2-fold increase in odds of being hospitalized for 3 or more days (OR: 1.95, 95% CI: 1.74–2.20).
5 LIMITATIONS
This was a large retrospective study of data obtained directly from prehospital electronic health records. As a convenience sample of records from participating agencies in a data collaborative using a single software provider, these findings are not intended to represent a quantification of disease prevalence in any particular region. Further, only a subset of agencies and receiving facilities use the health data exchange software that links EMS records to hospital outcome information. The analytic sample was more weighted toward urban settings; these findings may not generalize to other environments. Thus, interpretations of the results presented should focus on the observed associations between variables, in particular first EMS REMS and dispositions following EMS transport and direct extrapolation to other settings is cautioned.
Data were entered during the course of patient care activities with no researcher quality checks other than for missing data elements. Approximately 8% of records had 1 or more missing REMS data elements, meaning that REMS could not be calculated. ED dispositions were similar among those without a REMS score, as 29% (353) were discharged and 67% were admitted (813). This study included only patients with a documented hospital diagnosis of COVID-19 regardless of whether the EMS professional recognized the potential for COVID-19 during field assessment. It is possible that some patients presented to EMS with other primary concerns not related to COVID-19 such as traumatic injury. It is also possible that EMS clinicians suspected COVID-19 during the encounter and that a patient later tested negative for the disease at the hospital. We limited this analysis to patients diagnosed with COVID-19 to specifically examine predictive characteristics of REMS in this unique patient population with a novel disease. Prior studies have demonstrated the value of prehospital REMS for predicting hospital outcomes for a general cohort of EMS-transported patients, suggesting utility even when the EMS suspicion of COVID-19 may not be confirmed.14, 17 Nevertheless, future research will be required to determine whether REMS is a useful predictor of hospital outcomes for the subset of EMS patients with suspected COVID-19 with and without confirmation at the hospital after transport. Likewise, this study could not comment on the predictive value of REMS for patients who were not transported to the hospital; prior studies have suggested that nearly 18% of COVID-19 patients who called 911 were not transported to the hospital.6
This study relied on the initial prehospital REMS score, calculated using the chronologically first available elements, to predict hospital outcomes. Prehospital and hospital interventions delivered after these first measurements may have confounded the patient's condition and subsequently outcomes. It is unknown whether REMS scores calculated using data more proximate to hospital arrival would be more or less predictive. This study was also limited to evaluation of REMS without consideration of other potential scoring systems. However, prior studies have demonstrated that REMS provides comparable or superior prediction of hospital outcomes when comparing a number of available scoring systems including National Early Warning System, MEWS, Vitalpac Early Warning Score, Worthing Physiological Scoring System, Triage Early Warning Score, and the Prehospital Index.14 The REMS also does not require a body temperature measurement, which is not consistently recorded in the prehospital setting.28-30
6 DISCUSSION
In this retrospective study of over 13,000 confirmed COVID-19 patients transported to the hospital by EMS, first prehospital REMS was associated with ED and hospital outcomes. Adequate EMS data were present to calculate REMS in 92% of cases, substantially higher than previously reported,17, 24 suggesting that REMS may be a practical tool for use in the prehospital setting. Collectively, these findings suggest utility of REMS in the specific and sometimes complex COVID-19 patient population. The proposed cut-points may provide tools to support EMS transport decisions and hospital preparation for admission and use of scarce intensive care resources.
Overall predictive characteristics of first prehospital REMS for ED and in-hospital patient dispositions were moderate and in line with widely used prehospital screening instruments for conditions such as stroke.31 As previous authors have reported,17, 32 we found that prehospital REMS demonstrated slightly higher predictive power for ED mortality than ED discharge or hospital admission. Nevertheless, REMS demonstrated good discrimination for predicting ED discharge. The observed AUROC of 0.72 (95% CI: 0.71–0.73) is comparable to the 0.76 reported for predicting hospital admission in a study using REMS data collected on non-trauma patients in the ED.17 This discrimination level is also similar to the AUROC of REMS as a predictor of ED discharge (0.684) among a large cohort of all EMS-transported patients.17 The hospital admission rate for patients in this study (71%) was nearly double that reported in a large cohort of all EMS-transported patients (36%). The median age and first prehospital REMS score were higher in this cohort of EMS patients diagnosed with COVID-19 compared to the study of all EMS-transported patients.17 The optimal REMS cut-point of 5 or lower for predicting ED discharge (6 or higher for predicting admission, transfer, or hospice) aligns with that found among the cohort of all EMS-transported patients. This cut-point is also similar to the cut-point of 7 or higher reported by Wei for predicting hospital admission; the higher cut-point reported by Wei may reflect the younger population (mean age 44).17, 32 The similarity of the results across these 3 studies with substantially different populations may suggest that REMS can be a broadly applicable adjunct for helping predict ED discharge or hospital admissions.
Our findings suggest that the predictive accuracy of REMS is best for clinical outcomes that are proximate in time to when the data were collected and declines for outcomes that are hours or days later. Clinically this may relate to changes in the patient's condition between the time of REMS measurement and the outcome in question. If this premise is accurate, it suggests the possibility that REMS could become a tool for evaluating trends in patient condition over time rather than a static determination of mortality or hospital admission probability. This observation has been made in at least 1 previous study that described changes in REMS during the prehospital encounter and noted that reductions in patients with high first REMS may reflect clinical changes during care.33 If measured before and after a specific intervention (such as EMS care and transport) change in REMS may even reflect the impact of the intervention on patient survival, admission, or LOS. The change in REMS during a patient encounter may also have important implications when considering which EMS data to use when calculating REMS (early or late in the clinical encounter). More research is needed.
The ability of REMS to help predict which patients will be able to be discharged from the ED (and which will require admission) complements other research aimed at predicting surges. Two French studies demonstrated that identification of surges in requests for EMS services preceded actual hospital and ICU surges by 12–19 days.9, 10 A similar study in Maryland found that increases in the rate of EMS patients suspected by crews as having COVID-19 predicted increases in COVID-19 hospitalizations by 9 days.11 A complex algorithm informed by the number of daily calls to regional National Health Service (UK) offices was also successful in predicting local COVID-19 case volumes.34 A score that could predict LOS provides a valuable tool for hospital planners to anticipate how long a COVID-19 patient may need to be hospitalized. This study demonstrated a moderate ability for REMS to predict prolonged (3 or more days) hospital admission with a cut-point of 7 or higher and an AUROC of 0.62 (95% CI: 0.60–0.63), virtually identical to other reports.32 Prior studies with similar aims have shown mixed results. Mughal et al used a retrospective study of hospitalized, confirmed COVID-19 patients to identify information available at admission that could predict the onset of ventilatory-dependent acute respiratory failure. Predictive scores including qSOFA, CURB-65, and MEWS were unable to differentiate between patients requiring intubation and those who did not.22 The COVID-19 Acuity Score is a recently validated score that predicts hospital admission (AUC 0.80), critical care admission (AUC 0.82), and death (AUC 0.87) for COVID-19 patients in the outpatient setting, but it requires multiple data elements that are not available for most patients in the out-of-hospital setting such as chest radiograph, body mass index, and an exhaustive past medical history.3 Although the current study did not evaluate REMS ability to identify patients who will require ICU admission, it does appear to predict the need for hospitalization and potentially identify those requiring a longer LOS.
Likewise, this study contributes to research proposing the use of EMS data to support health system efforts to reduce the number of COVID-19 patients who seek care in the hospital and may be safely treated as outpatients. An Israeli study demonstrated successful screening of potential COVID-19 patients via telephone. Symptomatic patients were screened by paramedics and referred to physicians as appropriate. EMS also provided polymerase chain reaction testing at patients’ homes. Patients who were symptomatic and had a positive COVID-19 test were transported by EMS to a negative pressure bed in the COVID-19 section of a designated ED.19 Goldberg et al. reduced the entry of potential COVID-19 patients into the healthcare system by having EMS send a “testing team” to the home of patients identified by their primary care practitioner as having a high risk for COVID-19 based on symptoms reported by telephone. EMS successfully performed over 400 home-based tests with no personal protective equipment breaches or EMS crew infection.18 The current study may add to this literature by demonstrating that REMS can help identify patients who are unlikely to require hospital admission and might be safe candidates for monitoring and care outside of the hospital.
In summary, in this large cohort of EMS patients diagnosed with COVID-19, first prehospital REMS demonstrated moderate predictive value for ED mortality, ED discharge, hospital mortality, and hospital LOS. From a healthcare system planning perspective, prehospital REMS may provide early evidence to identify a subset of admitted patients who may require prolonged admission and increased resource use. At the encounter level, prehospital REMS may represent an important adjunct for decision making for patients who may be candidates for safe treatment at home or an alternative destination versus transport to an ED. Collectively, these findings expand prior studies that demonstrate the value of prehospital REMS in predicting hospital disposition by demonstrating a moderate ability to risk stratify and surveil EMS patients diagnosed with COVID-19.
ACKNOWLEDGEMENT
The authors would like to acknowledge the ESO agencies who have agreed to have their de-identified data included in the ESO Data Collaborative as well as the thousands of frontline EMS providers who entered these data during the course of their patient care.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
Study conceptualization and design: SSB, RPC, ARF, JBM. Literature review: SSB. Data analysis and interpretation of results: SSB, RPC, ARF, SEM, ALB, ABH, JBM. Manuscript development: SSB, RPC, ARF, SEM, ALB, ABH, JBM.





