Site-specific accumulation of recently activated CD4+Foxp3+ regulatory T cells following adoptive transfer
Abstract
CD4+Foxp3+ regulatory T (Treg) cells are required for the maintenance of self-tolerance, as demonstrated by profound autoimmunity in mice and humans with inactivating Foxp3 mutations. Recent studies demonstrate that Treg cells are anatomically compartmentalized within secondary lymphoid organs based on their TCR repertoire and specific organ-protective function; however, whether this reflects differential homing or in situ selection is not known. Here, using Foxp3-GFP reporter mice, we have examined the ability of polyclonal Treg cells from cervical LNs to return to their site-of-origin following adoptive transfer to nonlymphopenic congenic recipients. We find that bulk cervical LN Treg cells do not home directly to cervical LNs but rather accumulate site specifically over time following transfer. Site-specific enrichment is both more rapid and more pronounced among a population of recently activated (CD69+) Treg cells. These data suggest that compartmentalization of Treg cells within secondary lymphoid organs may be governed by antigen recognition and implicate CD69 as a potential marker of recently activated Treg cells recognizing locally expressed antigens.
Introduction
CD4+Foxp3+ regulatory T (Treg) cells play a nonredundant role in preventing naturally occurring autoreactive lymphocytes from causing spontaneous autoimmune disease. This is underscored by the widespread fatal autoimmunity in mice and humans with inactivating Foxp3 mutations [1]. Although Treg-cell defects have been implicated in various spontaneous autoimmune diseases, identification of defects within specific Treg-cell subsets and their role in autoimmunity requires a more comprehensive understanding of how Treg cells are anatomically organized. Further, better understanding how Treg cells distribute throughout secondary lymphoid organs following adoptive transfer is particularly important as cellular adoptive therapies become a reality [2].
Treg cells are distributed anatomically with distinct TCR repertoires within different secondary lymphoid organs [3] and display enriched organ-protective function within organ-draining LNs [4]. However, whether and how this is achieved following adoptive transfer is unknown. Specifically, do adoptively transferred Treg cells home directly to their site-of-origin, or do they initially distribute nonpreferentially with subsequent site-specific accumulation? In this study, through a series of adoptive transfers of Treg cells into nonlymphopenic congenic hosts, we show that Treg cells from cervical LNs (cervLNs) do not directly or exclusively home to cervLNs following transfer but, instead, accumulate site specifically over weeks following transfer. Moreover, we show that a sizeable proportion of cervLN Treg cells are recently activated (CD69+) at steady state and demonstrate earlier site-specific accumulation compared to bulk cervLN donor Treg cells and greater site-specific accumulation compared to either CD69− or bulk cervLN donor Treg cells, suggesting this process may be dependent on antigen recognition. Our work thus supports a role for antigen in establishing and maintaining specific Treg-cell distribution and identifies CD69+ cervLN Treg cells as a useful population for studies to further elucidate molecular mechanisms of the site-specific accumulation of Treg cells following transfer.
Results and discussion
CervLN donor Treg cells accumulate site specifically over time following adoptive transfer
To evaluate whether Treg cells home directly and exclusively to their site-of-origin following adoptive transfer, congenically marked Treg cells purified from cervLNs of Foxp3-GFP donor mice were transferred to nonlymphopenic congenic Foxp3-GFP recipient mice. The presence of donor Treg cells within different secondary lymphoid organs was then assessed by flow cytometry at serial time points (Fig. 1). We chose to focus on cervLN Treg cells for several reasons: (i) cervLN Treg cells have been shown to be compartmentalized in both TCR repertoire and organ-protective function studies [3, 4]; (ii) cervLN Treg cells represent a larger population than skin-draining LN (skinLN) Treg cells and thus require fewer donor mice for adequate donor cell numbers (Table 1); and (iii) cervLN donor Treg cells are more readily recoverable following adoptive transfer to nonlymphopenic recipients compared to gut-draining LN (gutLN) donor Treg cells (our unpublished observations). The relatively small donor Treg-cell populations recovered (Fig. 1A–C) are comparable to previous reports of Treg-cell transfers to nonlymphopenic recipients [5, 6]. At 1, 4, and 12 weeks following transfer, donor Treg cells were recovered from each location, including cervLNs, skinLNs, gutLNs, and spleen (Fig. 1A–C, and Supporting Information Fig. 1). Thus, adoptively transferred Treg cells do not home directly or exclusively to their site-of-origin.
| Group | Abbreviation | LNsa | Total number of cells (×106)b | CD4+Foxp3+ (percentage of total cells)b | CD4+Foxp3+ (×105)b |
|---|---|---|---|---|---|
| Cervical | cervLN | Mandibularc, accessory mandibularc, superficial parotid | 8.75 ± 0.625 | 5.24 ± 0.36 | 4.56 ± 0.4 h |
| Skin-draining | skinLN | Proper axillary, accessory axillaryd, subiliace, popliteal | 5.16 ± 0.664 | 4.77 ± 0.47 | 2.34 ± 0.25 h |
| Gut-draining | gutLN | Jejunalf, colic, pancreaticoduodenalg, gastric | 13.7 ± 2.72 | 5.39 ± 0.24 | 7.05 ± 1.1 |
| Spleen | − | − | 41.1 ± 3.98 | 3.04 ± 0.16 | 12.6 ± 1.5 |
- a Anatomical names based on [14]; common names noted below based on [15].
- b Live cell counts by Trypan blue exclusion,percentage CD4+Foxp3+ cells by flow cytometry, and number of CD4+Foxp3+ calculated. Data represent mean ± SEM pooled from eight individual mice in three independent experiments.
- c Commonly referred to collectively as superficial cervical.
- d Commonly referred to as brachial.
- e Commonly referred to as inguinal.
- f Commonly referred to as mesenteric.
- g Commonly referred to as pancreatic.
- h p = 0.0005 by two-tailed paired t-test comparing cervLN to skinLN.

To determine if Treg cells would accumulate within the cervLNs over time, we first determined their relative distribution at each time point posttransfer (Fig. 1D). Over time, there is an increasing trend in the proportion of donor Treg cells recovered within the cervLNs (Fig. 1D). Not surprisingly, many donor Treg cells were recovered from sites with greater total cell numbers such as spleen and gutLNs (Fig. 1D and Table 1). To account for this, we calculated enrichment factors that normalized the relative distributions of donor Treg cells to that of recipient Treg cells for each site within each individual mouse. Specifically, we calculated enrichment factors as log2 of the ratio:percent of all recovered donor Treg cells that are recovered from a particular site divided by the percent of all recovered recipient Treg cells recovered from that site. Enrichment factors >0 suggest relative enrichment of donor cells at that site, whereas values <0 suggest a relative exclusion from that site. At all time points following transfer, cervLN donor Treg cells are relatively excluded from gutLNs (Fig. 1E). This is consistent with the recent finding that pooled LN and spleen-derived Treg cells are recovered preferentially within non-gutLNs following adoptive transfer [6] and suggests decreased access to, or decreased retention or survival within gutLNs. Initially, there is a trend toward preferential accumulation within skinLNs (Fig. 1E). By 4 weeks posttransfer, maximal enrichment within cervLNs is achieved; however, nonsite-specific enrichment within skinLNs remains high at this time. Thus, at 4 weeks posttransfer, bulk cervLN Treg cells have not preferentially accumulated site specifically. At 12 weeks posttransfer, maximal site-specific (i.e. cervLN) enrichment is maintained whereas nonsite-specific enrichment has markedly diminished. These data demonstrate that over weeks following adoptive transfer, donor Treg cells accumulate preferentially (though not exclusively) within their site-of-origin.
One possibility is that cervLNs are unique and promote the preferential accumulation of any transferred Treg cells regardless of origin. To evaluate this, we transferred Treg cells isolated from either skinLNs or gutLNs to congenic recipients as above. Over time, adoptively transferred donor Treg cells from skinLNs and gutLNs do not accumulate within cervLNs to the same extent as do adoptively transferred Treg cells from cervLNs (Supporting Information Fig. 2). Thus, preferential accumulation of Treg cells within cervLNs following transfer is specific to cervLN donor Treg cells.
To determine whether similar site-specific accumulation is a property of conventional CD4+Foxp3− T (Tconv) cells, we performed transfer studies with Tconv cells isolated from gutLNs and non-gutLNs. Neither gutLN nor non-gutLN Tconv cells accumulated site specifically (Supporting Information Fig. 3) suggesting that site-specific accumulation may be a property specific to Treg cells.
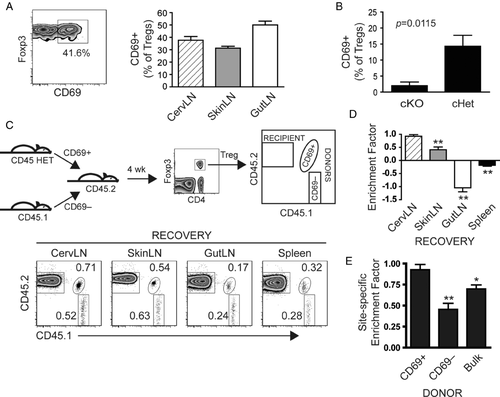
Recently activated Treg cells from cervLNs demonstrate enhanced site-specific enrichment
Given the distinct Treg-cell TCR repertoires within different secondary lymphoid organs [3], we hypothesized that recently activated Treg cells would demonstrate enhanced site-specific accumulation following adoptive transfer. CD69 is a cell surface marker rapidly upregulated following TCR activation [7] but which also may be upregulated by lymphocytes in the presence of inflammatory cues such as type I interferons [8]. In unmanipulated Foxp3-GFP reporter mice, 30–60% of Treg cells within each LN group were CD69+ (Fig. 2A). To evaluate the requirement for TCR signaling in CD69 expression by Treg cells at steady state, we analyzed Treg cells from mice in which the key TCR signaling adaptor molecule SLP-76 was conditionally deleted [9]. For these experiments, we used mice lacking either one (conditional heterozygous; cHet) or both (conditional knockout; cKO) copies of SLP-76. Following conditional deletion of SLP-76, the CD69+ Treg-cell population in cervLNs of cKO mice was greatly diminished demonstrating a requirement for SLP-76-mediated signaling in maintaining the population of CD69+ Treg cells at steady state (Fig. 2B). This suggests CD69 expression by Treg cells may be TCR mediated, though we have not excluded the possibility that other signals, such as via integrins, may play a role. We therefore used CD69 as a marker of activation to address our hypothesis that the recently activated Treg-cell subset would demonstrate enhanced site-specific accumulation compared to the nonactivated Treg-cell subset in adoptive transfer experiments. CervLN Treg cells congenically marked based on CD69 expression were co-transferred to recipient mice of a third congenic specificity (Fig. 2C) such that all three populations (CD69+ donor Treg cells, CD69− donor Treg cells, and recipient Treg cells) were readily identifiable. While donor Treg cells (both CD69+ and CD69−) were again recovered at all locations (Fig. 2C and Supporting Information Fig.4), the CD69+ donor Treg cells accumulated site specifically at 4 weeks posttransfer (Fig. 2D). Notably, this site-specific accumulation (defined as accumulation preferentially within site-of-origin compared to other sites) occurred earlier compared to that of bulk cervLN donor Treg cells. Enrichment within cervLNs was greater than enrichment within each noncervLN site at 4 weeks posttransfer for CD69+ donor Treg cells (Fig. 2D), whereas similar greater enrichment than each noncervLN site was not achieved by bulk donor Treg cells until 12 weeks posttransfer (Fig. 1E). Moreover, the CD69+ cervLN Treg cells clearly demonstrated enhanced site-specific accumulation compared to the CD69− or bulk cervLN donor Treg cells at 4 weeks posttransfer (Fig. 2E). This was specific to recovery at cervLNs as recovery at noncervLN sites was not dominated by CD69+ donor cells (Supporting Information Fig. 5). These data suggest that the site-specific accumulation of Treg cells may be governed, at least in part, by local SLP-76-mediated activation signals such as via TCRs, presumably reflecting antigen dependence.
This site-specific accumulation is likely due to a combination of local proliferation, survival, and retention. In a TCR transgenic system, antigen-specific Treg cells proliferated preferentially in LNs draining their cognate antigen [5]. Retention within secondary lymphoid organs has recently been demonstrated to result from CD69-mediated downregulation of sphingosine 1 phosphate receptor 1 (S1P1), a receptor required for lymphocyte egress from LNs [8, 10]. Our data show that TCR-mediated signals may be required for the expression of CD69 on a subset of Treg cells at steady state, and others have demonstrated downregulation of S1P1 by Treg cells following TCR stimulation [11]. Thus, site-specific retention mediated by downregulation of S1P1 following TCR stimulation may play a key role in site-specific accumulation following transfer by increasing Treg-cell dwell time within LNs in which their cognate antigen is presented. The recovery of either bulk or CD69+ donor cervLN Treg cells from all sites at each time point strongly argues against site-directed LN homing as a major factor in establishing Treg-cell distribution within specific LNs. Similarly, as of yet, no specific homing receptors that distinguish one LN versus another have been identified. Given the finding that Treg cells are present within both lymphoid and nonlymphoid tissues at steady state [12], however, we cannot exclude the possible contribution of nonlymphoid tissue-specific homing followed by recirculation to the draining LNs.
Concluding remarks
This study highlights a potential key role for antigen recognition in establishing and maintaining the compartmentalization of Treg cells within different secondary lymphoid organs. Our data identify CD69+ cervLN Treg cells as a readily abundant population of Treg cells that accumulate site specifically over time following adoptive transfer making them an ideal population for studies to further elucidate the molecular mechanisms of the compartmentalization of Treg cells within secondary lymphoid organs. Further understanding these mechanisms, such as identification of Treg-specific self-antigens, will provide tools to develop more efficient Treg-based cellular therapies aimed at directing in vitro expanded Treg cells to particular lymphoid compartments to treat organ-specific autoimmunity.
Materials and methods
Mice
Foxp3-GFP knockin reporter mice on the C57BL/6 background (CD45.2) [13] were bred with CD45.1 congenic C57BL/6 mice (B6.SJL-Ptprca Pepcb/BoyJ, The Jackson Laboratory) to generate CD45.1+, CD45.2+, and CD45.1+CD45.2+ heterozygous (CD45 HET) Foxp3-GFP reporter congenic strains. Tamoxifen inducible SLP-76 conditional knockout (cKO; SLP-76F/nullR26RyfpCreT2) and conditional heterozygous (cHet; SLP-76F/+R26RyfpCreT2) mice have been previously described [9]. For induced SLP-76 deletion, mice were treated with tamoxifen (Sigma), 200 μg/g/day by oral gavage for 5 days, then LNs were harvested 6–14 days after the last tamoxifen dose. Mice were maintained at the University of Pennsylvania under specific pathogen-free conditions and used in accordance with University of Pennsylvania Animal Care and Use Committee guidelines.
Cell sorting and adoptive transfer
CervLNs, skinLNs, or gutLNs (Table 1) were isolated from multiple congenic Foxp3-GFP mice. Single cell suspensions were treated with ACK lysing buffer (Lonza) to lyse RBC and labeled with Alexa Fluor 700-conjugated anti-CD4 (eBioscience) with or without allophycocyanin-conjugated anti-CD69 (BD) monoclonal antibodies. Treg cells (CD4+Foxp3+) or Tconv cells (CD4+Foxp3−) were purified by FACS on a FACSAria (BD). For some experiments, Treg cells were further sorted based on CD69 expression. For cotransfer experiments, CD69+ and CD69− Treg cells from different congenic Foxp3-GFP donor mice were combined prior to transfer. Cells in sterile PBS were transferred by retro-orbital injection. For SLP-76 experiments, YFP+ cells (SLP−/− for cKO or SLP+/− for cHet) were purified on an FACSAria prior to surface and intracellular staining.
Flow cytometry
Single cell suspensions from secondary lymphoid organs (Table 1) were labeled with fluorochrome conjugated monoclonal antibodies specific for cell surface molecules CD4 (Alexa Fluor 700), CD45.1 (eFluor450, eBioscience), CD45.2 (allophycocyanin, BD), with or without CD69 (PerCP-Cy5.5, BD), or appropriate isotype controls. For some experiments, cells were then fixed and permeabilized with a Foxp3 intracellular staining kit (eBioscience) according to manufacturer's protocol and stained with allophycocyanin-conjugated anti-Foxp3 (eBioscience) monoclonal antibody. Data were collected on a FACSCanto II (BD) or FACSCalibur (BD) and analyzed using FlowJo software (version 7.6.1, TreeStar Software, Inc). For transfer study analyses, a minimum of 1.5 × 106 singlet events within the lymphocyte gate were collected.
Calculation of distribution percent and enrichment factor
Donor Treg-cell distribution percent was calculated as the absolute number of donor Treg cells recovered within a particular site at a given time point divided by the total number of donor Treg cells recovered at all sites at that time point × 100%. Recipient Treg-cell distribution percent was similarly calculated in each experiment but data were pooled together from different time points given the observation that these recipient distribution percent did not differ between different time points.
Enrichment was defined as ((number of donor Treg cells recovered at site x)/(total number of donor Treg cells recovered at all sites)) / ((number of recipient Treg cells recovered at site x)/(total number of recipient Treg cells recovered at all sites)). In other words, enrichment represents the fold change of the fraction of all recovered donor Treg cells which were recovered at site x compared to the fraction of all recovered recipient Treg cells recovered at that site. Similar enrichment calculations were performed with Tconv cells. To transform these exponentially growing ratios to a linear function, the enrichment factor was defined as log2 (enrichment).
Statistics
Statistical analyses were performed with Prism version 4.00 (GraphPad Software). For comparison of two groups, unpaired two-tailed Student's ttest was used. For comparison of multiple groups, repeated measures one-way ANOVA with Dunnett's posttest was used. For two-dimensional analyses, repeated measures two-way ANOVA with Bonferroni posttest was used. Repeated measures ANOVA were used to account for cells isolated from different locations within the same recipient mouse. Statistical significance was defined as p < 0.05.
Acknowledgements
We thank Ryan Wychowanec and the University of Pennsylvania Flow Cytometry and Cell Sorting facility for technical assistance, Martha Jordan and Gary Koretzky for critical reading of the manuscript, and Adeeb Rahman, Tao Zou, Matthew Riese, and members of the Turka, Koretzky, and Behrens labs for assistance and discussion. This work was supported by NIH grants T32 DK07006-35 (S.M.L.), AI37691, and AI41521 (L.A.T.), and by an Arthritis Foundation Postdoctoral Fellowship (S.M.L.).
Conflicts of interest
The authors declare no financial or commercial conflict of interest.
References
Abbreviations
-
- cervLN
-
- cervical LN
-
- cHet
-
- conditional heterozygous
-
- cKO
-
- conditional knockout
-
- gutLN
-
- gut-draining LN
-
- skinLN
-
- skin-draining LN
-
- Tconv cell
-
- conventional CD4+Foxp3– T cell




