Heart failure as a general pandemic in Asia
Abstract
Heart failure (HF) is an epidemic in healthcare worldwide, including Asia. It appears that HF will become more serious in the near future, with the epidemiological transition and ageing of the population. However, in contrast to Western countries, information on HF epidemiology is still limited in Asia, particularly in South Asia. In this review, we will briefly summarize available information regarding the current and future burden of HF in Asia, which indicates the importance of both primary prevention of underlying diseases of HF and secondary prevention, including management of ischaemic HF, HF with preserved EF, and HF in the elderly.
Burden of heart failure in Asia
The number of patients with heart failure (HF) has been rapidly increasing to an estimated 26 million patients worldwide, which is the so-called ‘HF pandemic’.1, 2 In the USA, 5.1 million individuals aged ≥20 years have HF, 825 000 aged ≥45 years are newly diagnosed as having HF every year,3 and >1 million patients are hospitalized for HF in both the USA and Europe.1 This HF pandemic is also evident in Asia,4-6 although available information is still limited on the incidence and prevalence of HF in the region.7-12 In Singapore, Ng et al. reported that the number of elderly (≥65 years) patients hospitalized for congestive HF increased from 1436 to 2457 during the period from 1991 to 1998, with an absolute increase of 71% and an age-adjusted increase of 38%.9 In this study, the overall prevalence of HF admission accounted for 4.5% of all admissions between 1991 and 1998 in Singapore.9 In Malaysia, it was reported that the prevalence of HF was 6.7% among 1435 acute medical admissions in the Kuala Lumpur General Hospital over the 4-week study period.10 In Taiwan, Tseng reported that HF hospitalization was identified in 2712 patients (0.27%) out of 1 million people insured by the National Health Insurance programme in 2005, which accounted for 3.4% of 79 299 patients who were hospitalized in the study cohort.11 Thus, the prevalence of HF among hospitalized patients ranges from 3.4% to 6.7% of the admission-based estimates in Asia (Table 1).9-11 In a survey reported in 2003, the prevalence of HF was 0.4, 0.9, 1.3, and 1.3% among populations aged 35–44, 45–54, 55–64, and 65–74 years, respectively, among 15 518 people in 20 urban and rural areas in China, reaching the estimation of >4 million HF patients aged 35–74 years in China.12 However, considering that the estimated number of the adult population aged >35 years has increased from 0.51 billion in 2000 to 0.72 billion in 2015 in China,13 it is conceivable that the number of HF patients has been increasing further in China. In Japan, it was estimated that ∼1 million people have HF,7 thus leading to an estimation of HF prevalence of ∼1%. In Western countries, it has been reported that the prevalence of HF was 2.1% in the population aged ≥20 years in the USA3 and ranged from 1% to 7% in European countries.14 Thus, it is assumed that the population-based prevalence of HF would be lower still in Asian countries compared with that in Western countries3, 14 (Table 1).
| Singapore | Malaysia | Taiwan | China | USA | Europe | |
|---|---|---|---|---|---|---|
| Survey year | 1991–1998 | NA | 2005 | Before 2003 | 2010 | NA |
| Publication year | 2003 | 2003 | 2011 | 2014 | 2014 | 2013 |
| Authors | Ng et al.8 | Chong et al.9 | Tseng10 | Hu et al.11 | Go et al.3 | Seferovic et al.37 |
| HF status | Hospitalized congestive HF | Primary diagnosis of congestive HF as a cause of admission | Hospitalized congestive HF | HF | HF | HF |
| No. of patients | 15 774 | 97 | 2712 | 15 518 | 5 100 000 | NA |
| Settings | Retrospective analysis of all admissions in the elderly (>65 years) in Singaporea | Retrospective screening of 1435 acute admissions in a single centre in Kuala Lumpur, Malaysia | Retrospective random sampling of 1 000 000 insured (79 299 hospitalizations). | Retrospective survey of 35- to 74-year-old Chinese in 20 urban and rural area in 10 provinces and cities. | National Health and Nutrition Examination Survey 2007–2010 and National Heart, Lung, and Blood Institute | Based on the questionnaires gathered at the first Heart Failure National Societies Summit in Belgrade, Serbia, on 29 October 2011 |
| Population-based prevalence of HF (%) | NA | NA | 0.27 | 0.9 | 2.1b | 1–7c |
| Hospital admission -based prevalence of HF (%) | 4.5 (≥65 years) | 6.7 | 3.4 | NA | NA | NA |
- HF, heart failure; NA, not available.
- a Based on hospital admission data from the national administrative database of the Central Claims Processing System in the Ministry of Health, Singapore.
- b Percentages are age adjusted for Americans ≥20 years of age.
- c 1% in Denmark, 1.5% in Czech Republic and Israel, 1.6% in Hungary, 1–2% in Norway, Slovakis, Sweden, Switzerland, and the UK, 2% in Ireland, Slovakia, Sweden, and Switzerland, 2.2% in France, 2.3% in Serbia, 2.98% in Lithuania, 2–3% in Belgium, 3.5% in Italy, 4.2% in Rumania, 4.4% in Portugal, and 7% in Russia.
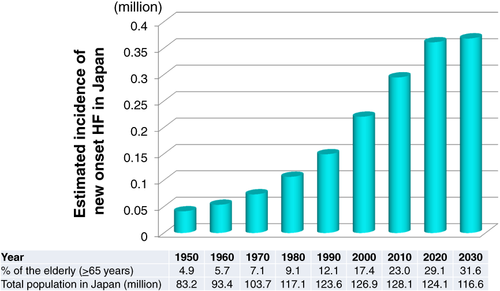
Using the estimated overall HF prevalence of 1.87% in the USA in 2010, Pillai and Ganapathi estimated the number of HF patients as 22.7 million among 1.21 billion people in India and 30 million among a total population of 1.63 billion people in South Asia in 2011.4 In contrast, based on disease-specific estimates of prevalence for the year 2000 and incidence rates of HF, Huffman and Prabhakaran estimated that the prevalence of HF due to CAD, hypertension, obesity, diabetes, and rheumatic heart disease (RHD) would range from 1.3 to 4.6 million, with an annual incidence of 0.49–1.8 million, in India.6 In Japan, Okura et al. estimated that the number of outpatients with LV dysfunction would steadily increase from 979 000 in 2005 to 1.3 million by 2030.7 Using the USA data that 10 out of 1000 people aged ≥65 years develop de novo HF per year,3 we assume that >0.3 million Japanese developed de novo HF among the 31.9 million people aged ≥65 years in 201315 and that >0.37 million would newly develop HF in 2025 (Figure 1). Thus, there is little doubt that a very large number of patients develop HF every year in Asia, indicating a general pandemic of HF worldwide.
Characteristics of heart failure patients in Asia
Table 2 shows the baseline characteristics of HF patients in Asia. In Japan, the mean age of stable HF patients in our CHART-2 (Chronic Heart Failure Registry and Analysis in the Tohoku District-2) Study,16-19 hospitalized HF patients in JCARE-CARD (the Japanese Cardiac Registry of Heart Failure in Cardiology),20, 21 and acute decompensated HF patients in the ATTEND (Acute Decompensated Heart Failure Syndromes) registry22, 23 was 69, 71, and 73 years, respectively. This means that the age of Japanese HF patients was comparable with that in Western registries, such as ADHERE (the Acute Decompensated Heart Failure Registry) (72 years)24 and the EHFS II (Euro Heart Failure Survey II) (70 years).25 In contrast, in the ADHERE International-Asia Pacific, the patients registered from the eight Asian-Pacific countries between 2006 and 2008 were relatively younger, with a median age of 67 years, ranging from 53 years in the Philippines to 77 years in Hong Kong, Taiwan, and Australia.26 Of note, nearly half of the patients in the Philippines were younger than 50 years, whereas more than one-third of the patients were older than 80 years in Hong Kong, Taiwan, and Australia in the ADHERE International-Asia Pacific.26 Although available information is limited in South Asia, Khan et al. reported that the mean age of HF patients (n = 276) was 54.4 years in Punjab Institute of Cardiology Lahore in Pakistan in 2008.27 Thus, HF patients in Asian countries, as compared with those in Western countries, are relatively younger except for South Korea, Hong Kong, Taiwan, Singapore, and Japan. This variation in age at admission for HF among Asian countries might be attributed to several factors including average life expectancy and stages of epidemiological transition. Indeed, the human development index (HDI),28 which is a composite measure of life expectancy, adult literacy, education enrolment, and standards of living, had a strong correlation with median admission age in the ADHERE International-Asia Pacific (r2 = 0.81, P < 0.005).26 As regards HF aetiology, CAD had the highest prevalence, ranging from 28.2% to 53.1%, followed by valvular heart disease (VHD) and cardiomyopathy, while the prevalence of hypertension was highest among the co-morbidities, ranging from 31.5% to 77.8% in Asia (Table 2).9, 10, 16, 21, 22, 29-32 However, it should be noted that infectious diseases are still major contributors to HF in Asia, particularly in South Asia. In India, the estimated number of patients with RHD aged 5–40 years is at least 1.4 million,33 and Joshi et al. reported in a small study (n = 125) that RHD was the most common underlying heart disease (52.8%) in India in 1999.34 It was also reported that RHD was the most frequent aetiology of HF in patients aged <40 years between 2000 and 2010 in Hubei Province, China.32 In addition to the high prevalence of RHD, the prevalence of COPD is also high in patients aged ≥35 years (4.1%) in India.35 Furthermore, India is estimated to have 1.41 million children aged 0–15 years with congenital heart diseases.36 Considering the high prevalence of RHD, COPD, and congenital heart diseases in Asia, a considerable number of patients would newly develop HF in the near future, warranting close attention on the further burden of HF in this region.
| Authors | Nochioka et al.29 | Shiba et al.16 | Hamaguchi et al.21 | Kajimoto et al.22; Sato et al.23 | Youn et al.30 | Lee et al.37 | Tseng11 | Yin et al.31 | Chong et al.9 | Atherton et al.26 | Adams et al.24; Atherton et al.26 | Nieminen et al.25 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | CHART-1 | CHART-2 | JCARE-CARD | ATTEND | KorHF | KorAHF | ADHERE-AP | ADHERE | EHFS II | |||
| Registration year | 2000–2004 | 2006–2010 | 2004–2005 | 2007–2011 | 2004–2009 | 2011–2012 | 2005 | 1993–2007 | NA | 2006–2008 | 2005–2006 | 2004–2005 |
| Location, country | Japan | Japan | Japan | Japan | Korea | Korea | Taiwan | China | Malaysia | Asia-Pacific Region | USA | Europe |
| HF status | Stage C/D | Stage C/D | Worsening HF as a primary cause of hospitalization | Acute HF syndrome | Hospitalized HF (survivor), LVEF <40% | Acute HF | Hospitalized congestive HF | Hospitalized HF | Hospitalized HF | Acute decompensated HF | Acute decompensated HF | Acute HF |
| No. of patients | 1078 | 4736 | 2549 | 4841 | 1527 | 2006 | 2692 | 6949 | 97 | 10 171 | 17 382 | 3580 |
| Settings | Prospective, multicentre, 26 hospitals, observational | Prospective, multicentre, 24 hospitals, observational | Prospective, multicentrer, 164 hospitals, observational | Prospective, multicentre, 52 hospitals, observational | Prospective, multicentre, 24 centres, observational | Prospective, multicentre, 10 centres, observational | Retrospective, random sampling of 1 000 000 insured | Retrospective, single-centre review of hospital records | Retrospective, single-centre, screening of 1435 acute admissions | Prospective, multicentre, 43 hospitals, 8 countries, observational | Prospective, multicentre, 301 hospitals, observational | Prospective, multicentre, 133 hospitals, 30 countries, observational |
| Age, years, mean/median | 68.7 (13.4) | 68.9 (12.3) | 70.7 (13.3) | 73.0 (13.8) | 69 (59–77) | 69 (14) | 73.1 (13.0) | 60.1 (16.3) | 63.6 | 67/66 | 75/– | 69.9 (12.5) |
| Male sex, % | 64.5 | 68.4 | 60 | 58 | 56 | 55 | 54.5 | 62.7 | 62.9 | 57 | 49 | 61.3 |
| Aetiology | ||||||||||||
| CAD, % | 26.4 | 47.1 | 32 | 31.2 | 40.1 | 38 | 31.5 | 45 | 49.5 | 50 | 57 | 53.6 |
| Cardiomyopathy, % | – | – | – | – | 21.9 | – | 7.42 | – | – | – | – | |
| DCM, % | – | – | 18.4 | 12.6 | – | – | – | 4.1 | – | – | 19.3 | |
| HCM, % | – | – | – | – | – | – | – | – | – | – | – | – |
| VHD, % | 23.8 | 23.8 | 27.7 | 19.4 | 10.7 | – | 27.5 | 4.1 | – | – | 34.4 | |
| HHD, % | 17.7 | 9.9 | 24.2 | 17.7 | – | 6 | – | – | 18.6 | – | – | – |
| Co-morbidity | ||||||||||||
| Hypertension, % | 47.4 | 74.3 | 52.8 | 69.1 | 42 | 59 | 38.9 | 38.7 | 49.5 | 64 | 77 | 62.5 |
| Diabetes mellitus, % | 19.5 | 23.3 | 30 | 33.8 | 31.4 | 36 | 28.1 | 18.3 | 28.9 | 45 | 45 | 32.8 |
| Prior MI, % | – | – | 27 | – | 15.4 | – | – | 12.8 | ||||
| Atrial fibrillation, % | – | – | 35.2 | – | 20.8 | 27 | – | 23.2 | 4.1 | 24 | 31 | 38.7 |
| Medications* | ||||||||||||
| RAS inhibitor, % | – | – | 76.5 | – | 68.0 | 65 | 50.8 | – | – | 63 | 67 | 80 |
| ACE inhibitor, % | 57.4 | 44.6 | 37.4 | 30.6 | 45.6 | – | – | – | – | – | – | – |
| ARB, % | 13.1 | 31.8 | 44.4 | 46.0 | 24.5 | – | – | – | – | – | – | – |
| Beta-blocker, % | 27.9 | 49 | 48.6 | 67.4 | 40.9 | 44 | 25.4 | – | – | 41 | 74 | 61 |
| Diuretics, % | 76.3** | 50.9** | – | – | – | – | 76.3 | – | – | – | – | – |
| AA, % | – | – | 41.6 | – | 37.5 | 40 | – | – | – | 31 | 20 | 48 |
| CCB, % | 30.5 | 31.8 | 25.2 | – | – | – | 29.3 | – | – | – | – | – |
| Digitalis, % | 48.1 | 23.5 | 30.9 | – | – | – | 32.4 | – | – | 34 | 26 | 31 |
| In-hospital mortality, % | – | – | – | 6.4 | – | 6.1 | 3.9 | 5.4 | 5.2 | 4.8 | 3 | 6.7 |
- AA, aldosterone antagonist; CCB, calcium channel blocker; DCM, dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy; HF, heart failure; HHD, hypertensive heart disease; MI, myocardial infarction; NA, not available; RAS, renin–angiotensin system; VHD, valvular heart disease.
- * Medications at outpatient clinics, during hospitalization, or at discharge.
- ** loop diuretics.
Management and outcomes of acute heart failure patients in Asia
In the ADHERE International-Asia Pacific, as compared with other Western HF registries, the prevalence of new-onset HF was higher, intravenous diuretics were administered at similar rates, and a higher proportion of patients received invasive mechanical ventilation.26 In the ATTEND registry in Japan22, 23 and the Korean Acute Heart Failure Registry (KorAHF) in Korea,37 the use of intravenous diuretics was relatively low (76.3% and 72%, respectively) as compared with ADHERE (92%)26 and EHFS II (84.4%).25 In contrast, the use of intraveneous vasodilators was more frequent in the ATTEND registry (78.3%) and in the KorAHF registry (40%)37 as compared with ADHERE (9%)26 and EHFS II (38.9%).25 In Asia, the most commonly used medication during hospitalization and/or at discharge is diuretics, followed by renin–angiotensin system (RAS) inhibitors, including ACE inhibitors and ARBs, and beta-blockers, although the prevalence of treatment with beta-blockers varied widely between 25.4% and 49% (Table 2).11, 16, 21, 23, 26, 30, 32 In Asian countries, in-hospital mortality due to HF ranged from 3.9% to 6.4%, while it was 3.0% and 6.7% in ADHERE and EHFS II, respectively (Table 2).
Management and outcomes of chronic heart failure patients in Asia
We have recently reported that in our CHART Studies in Japan, the use of RAS inhibitors and beta-blockers for Stage C/D HF patients increased from 69.1% and 27.9% in 2000–2004 to 72.3% and 49.0% in 2006–2010, respectively, while that of loop diuretics and digitalis decreased.5, 16 In the ADHERE International-Asia Pacific, it was reported that patients at discharge received aldosterone antagonists more and beta-blockers less as compared with ADHERE (Table 2).26 In South Asian countries, it was reported that the most commonly used medications are beta-blockers, ACE inhibitors/ARB, diuretics, and aldosterone antagonists.4
Although available data are limited, implantable cardioverter defibrillators (ICDs) and/or CRT are likely to be underused in Asian countries. In our CHART-2 Study (n = 10 219), among 2,778 patients with ischaemic heart disease or dilated cardiomyopathy in NYHA class II/III, 315 had an LVEF ≤35%.38 Among them, according to the Japanese Circulation Society guideline, 56 with a history of non-sustained ventricular tachycardia and the remaining 259 without it were considered to have class I and IIa recommendations for ICD implantation,39 respectively. However, the use of prophylactic ICD was only 30.4% and 6.6% in each group, respectively.38 It is also estimated that ICDs are underused, particularly in South Asia, partly due to limited accessibility and affordability.5
Although long-term mortality data are limited, Youn et al. reported that 1-year mortality after discharge was 9.2% in HF patients with reduced LVEF in South Korea.30 In the JCARE-CARD, the rates of all-cause death, cardiac death, and re-hospitalization due to worsening HF were 20.6, 12.7, and 36.3%, respectively, during a 2.1-year follow-up after discharge.21 In our CHART-2 Study, the crude mortality rate was 49.2/1000 person-years without significant sex difference during the median 3.1-year follow-up (52.4/1000 person-years for women vs. 47.3/1000 for men, P = 0.225).19
Cardiovascular disease burden in epidemiological transition as a cause of the heart failure pandemic in Asia
Since the 1950s, there has been a burden of cardiovascular disease (CVD) worldwide, although geographic variations may also exist.40-42 There has been an apparent epidemiological transition, including a decrease in infection-related deaths in childhood and a concomitant increase in cardiovascular and other chronic diseases.40-42 This transition appears to have played a central role in the HF burden.40-42 Although there are few studies examining the trends in HF during the epidemiological transition in Asia, the involvement of the transition in the HF burden has been associated with an increase in CVD, particularly that in CAD. For example, in India, the prevalence of CAD has increased in association with reduced infant mortality, increased personal income, intake of a high-fat diet, and prolongation of life expectancy.43 Indeed, the average life expectancy in India was only 41 years in 1951–1961, increased to 61.4 years in 1991–1996, and is projected to reach 72 years by 2030,43 creating an enlarging pool of candidates of CVD and subsequent HF.
During the process of the epidemiological transition, industrialization and urbanization played a significant role in shifting the major causes of death and disability from nutritional deficiencies and infectious diseases to degenerative diseases including CVD.41, 42 Urbanization inevitably increases consumption of high-calorie foods, while it reduces physical activity and energy expenditure. Industrialization also makes people sedentary, particularly in rural areas, through mechanization in agriculture and use of motor cars. Indeed, we found that the age-adjusted incidence of acute myocardial infarction (AMI) in young (≤44 years) and middle-aged (45–64 years) male patients significantly increased from 1998 to 2009 in the rural area but not in the urban area of the Miyagi prefecture in Japan, along with a markedly increased prevalence of dyslipidaemia.44 Furthermore, in Japan, the prevalence of ischaemic HF has increased from the CHART-1 to the CHART-2 Study, as has that of diabetes mellitus and hypertension.16 This increase in ischaemic aetiologies in patients with HF was also reported in Beijing, China.45 Thus, along with the introduction of high-fat diets, smoking, and sedentary lifestyles, non-communicable diseases are predominating, with the highest mortality caused by CVD, particularly in the younger generation in both rural and urban areas in Asia. In fact, the REACH (Reduction of Atherothrombosis for Continued Health) registry demonstrated that the average age of patients with atherothrombosis or those at high risk was relatively younger in Asia (65 years) as compared with other regions (69 years).46 Similarly, two recent large-scale studies revealed that the age of onset for acute coronary syndrome (ACS) is much lower in India than in the Western population.47, 48 Furthermore, it should be underlined that the increased incidence of CVD could further enhance the continuing burden of infectious, nutritional, and perinatal diseases, which has been noted as the ‘double-burden’ in developing and middle-income countries.49
Increase in ischaemic heart failure in Asia
In Western countries, increased prevalence of ischaemic HF after AMI has been noted since the 1970s.50, 51 Velagaleti et al. evaluated 676 Framingham Heart Study participants in the USA between 45 and 85 years of age (mean age 67 years, 34% women) who developed a first AMI between 1970 and 1999.50 They found higher risks of HF at 30 days [risk ratio (RR) 2.05, 95% confidence interval (CI) 1.25–3.36] and 5 years (RR 1.74, 95% CI 1.07–2.84) in patients who developed AMI in 1990–1999, as compared with the period 1970–1979, whereas 30-day and 5-year mortality rates were decreased.50 Similarly, Ezekowitz et al. performed a population-based cohort study with 7733 patients aged ≥65 years who were hospitalized for a first AMI and without a prior history of HF between 1994 and 2000 in Canada.51 They found that the 5-year rate of HF increased by 25%, whereas the 5-year mortality rate after AMI decreased by 28%.51 These studies gave us an important message that the prevalence of ischaemic HF after AMI has been increasing in exchange for improved mortality due to better implementation of coronary reperfusion therapies and evidence-based medications in the current era.
Although available data are still limited on the increasing prevalence of ischaemic HF after AMI, this may also be the case in Asia. In Japan, we found that the prevalence of ischaemic HF accounted for 25.3% in the CHART-1 Study, with patient enrolment between 2000 and 2004,29, 52 and was markedly increased to 47.1% in the CHART-2 Study with enrolment between 2006 and 2010.16-19 Importantly, the increased prevalence of ischaemic HF was accompanied by that of hypertension and diabetes, demonstrating the rapid trend of Westernization of HF aetiology in Japan.6, 16 This trend of Westernization was also reported from China.45 These lines of evidence strongly suggest the current and future burden of ischsemic HF in Asia, although there is little information available for South Asia. Furthermore, we have recently reported that the prevalence of hypertension and diabetes has increased in patients with dilated cardiomyopathy in Japan,53 indicating that primary prevention for CAD is also needed for non-ischaemic HF in the current and future era.
Increased prevalence of heart failure with preserved ejection fraction
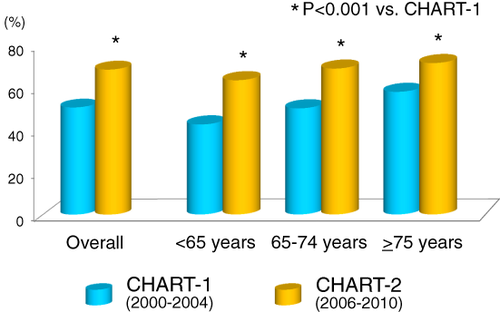
In addition to the burden of ischaemic HF, the increasing prevalence of HF with preserved ejection fraction (HFpEF) has been reported in Western countries.54 In Asia, however, limited data are available on the prevalence of HFpEF except for Japan. In Japan, we reported that the prevalence of HFpEF, defined as HF with LVEF ≥50% in Stage C/D, was increased from 50.6% in the CHART-1 Study to 68.7% in the CHART-2 Study (P < 0.01) (Figure 2).16 The all-cause mortality rate was 14.1% in HFpEF, which was better than in HF with reduced ejection fraction (HFrEF) (18.7%) during the median follow-up of 3.4 years in the CHART-2 Study.55 In contrast, in patients hospitalized for HF in the JCARE-CARD study, unadjusted risk of in-hospital mortality (6.5 vs. 3.9%; P = 0.03) and post-discharge mortality (22.7 vs. 17.8%; P = 0.058) was slightly higher in patients with preserved EF, although there were no difference after multivariable adjustment.20
Despite the marked increase in the prevalence of HFpEF, effective strategies still remain to be established for the disorder.56-59 Furthermore, it is interesting to note that geographic variation is also evident in the characteristics and outcomes of HFpEF patients, but not in patients with HFrEF.60, 61 For example, the post-hoc analysis of the TOPCAT (Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist) Trial showed a marked difference in the incidence of primary endpoints between HFpEF patients in Russia and Georgia and those in the USA, Canada, Brazil, and Argentina, which could be explained by the differences in clinical backgrounds between the two regions.60 Indeed, the HFpEF patients enrolled in our recent SUPPORT (Supplemental Benefit of Angiotensin Receptor Blocker in Hypertensive Patients with Stable Heart Failure Using Olmesartan) Trial,62 in which a total of 1147 Japanese hypertensive patients with symptomatic HF (mean age 66 years, 75% male) were randomized to the addition of olmesartan to baseline therapy (n = 578) vs. control (n = 569), had different baseline characteristics and all-cause mortality from those enrolled in the TOPCAT Trial (Supplementary material online, Table S1). Thus, effective strategies for HFpEF in Asia remain to be established in a different manner from those in Western countries. We have recently reported that the use of statins was associated with improved mortality in HFpEF patients, but not in HFrEF patients.55 Interestingly, this beneficial impact of statins was mainly attributed to reduction in sudden death and non-cardiovascular death.55 Thus, although caution is needed to interpret the results with regard to other populations, the potential benefit of statins remains to be examined for the management of HFpEF in clinical practice.
Heart failure in the elderly in Asia
The incidence of HF increases with age. In the Framingham study,63 the annual incidence of HF in men (per 1000) was increased from 3 in 50–59 years to 27 in 80–89 years, while women had a relatively lower incidence of HF (approximately one-third lower) than men. Also, it is important to note that more than half (54%) of the world's population over the age of 65 years lives in Asia in 2015.64 Furthermore, the most explosive ageing will occur in Asia, particularly in India and China; the proportion of the elderly population aged ≥65 years is currently 8.2% in 2015 and will be increased to 11.0% by 2030 in the world, while the proportion will increase from 7.4% in 2015 to 10.9% in 2030 in Asia.64 Thus, management of elderly HF patients is an emerging issue along with prolongation of life expectancy, not only in developed countries such as Japan, Hong Kong, South Korea, and Singapore, but also in other Asian developing countries.
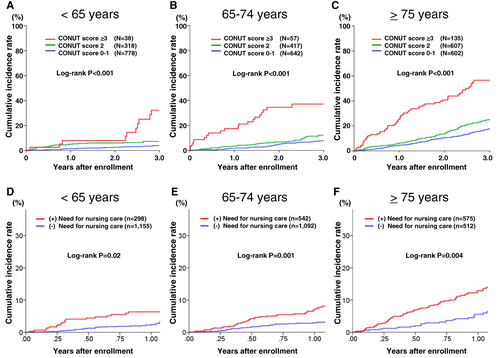
In the elderly population, HF conditions are more likely to depress appetite and gastrointestinal functions and decrease muscle volumes and physical activity, resulting in malnutrition and frailty, both of which are associated with a poor prognosis of HF.65, 66 Thus, special attention should be paid to nutrition and physical conditions in the management of elderly HF patients. Indeed, in our CHART-2 Study, poor nutritional status in the elderly population, assessed by the controlling nutritional status (CONUT) score (Supplementary material online, Table S2)67 was associated with poor prognosis in HF patients in Stage C/D (Figure 3A–C), a finding consistent with asymptomatic Stage B patients with structural and/or functional heart disease,68 and the need for nursing care, which was associated with increased mortality, was very high in HF patients (Figure 3D–F).69 Furthermore, we also have reported that the baseline level of physical activity and its yearly changes were significantly associated with all-cause death and major cardiovascular events in HF patients.70 These lines of evidence indicate that nutrition, frailty, and physical inactivity are important therapeutic targets to improve the prognosis of HF patients, particularly for the elderly population.
Conclusion
The burden of HF is a global pandemic worldwide, including in Asia. The characteristics of HF patients are not homogenous even among Asian countries due to different environments. However, to better manage the burden of HF in Asia, both primary prevention of underlying diseases of HF and secondary prevention, including management of ischaemic HF, HFpEF, and HF in the elderly, are important. Further evidence in Asia is needed in order to overcome the HF pandemic in Asia.
Conflict of interest: H.S. received lecture fees from Bayer Yakuhin, Ltd (Osaka, Japan), Daiichi Sankyo Co., Ltd (Tokyo, Japan), and Novartis Pharma K.K. (Tokyo, Japan). All other authors have no conflicts of interest to declare. The Department of Evidence-based Cardiovascular Medicine, Tohoku University Graduate School of Medicine, is supported in part by unrestricted research grants from Daiichi Sankyo Co., Ltd (Tokyo, Japan), Bayer Yakuhin, Ltd (Osaka, Japan), Kyowa Hakko Kirin Co., Ltd (Tokyo, Japan), Kowa Pharmaceutical Co., Ltd (Tokyo, Japan), Novartis Pharma K.K. (Tokyo, Japan), Dainippon Sumitomo Pharma, Co., Ltd (Osaka, Japan), and Nippon Boehringer Ingelheim Co., Ltd (Tokyo, Japan).