Clinical phenotypes of cardiogenic shock survivors: insights into late host responses and long-term outcomes
Abstract
Aims
An elevated risk of adverse events persists for years in cardiogenic shock (CS) survivors with high mortality rate and physical/mental disability. This study aims to link clinical CS-survivor phenotypes with distinct late host-response patterns at intensive care unit (ICU) discharge and long-term outcomes using model-based clustering.
Methods and results
In the original prospective, observational, international French and European Outcome Registry in Intensive Care Units (FROG-ICU) study, ICU patients with CS on admission were identified (N = 228). Among them, 173 were discharged alive from the ICU and included in the current study. Latent class analysis was applied to identify distinct CS-survivor phenotypes at ICU discharge using 15 readily available clinical and laboratory variables. The primary endpoint was 1 year of mortality after ICU discharge. Secondary endpoints were readmission and physical/mental disability [short form-36 questionnaire (SF-36) score] within 1 year after ICU discharge. Two distinct phenotypes at ICU discharge were identified (A and B). Patients in Phenotype B (38%) were more anaemic and had higher circulating levels of lactate, sustained kidney injury, and persistent elevation in plasma markers of inflammation, myocardial fibrosis, and endothelial dysfunction compared with Phenotype A. They had also a higher rate of non-ischaemic origin of CS and right ventricular dysfunction on admission. CS survivors in Phenotype B had higher 1 year of mortality compared with Phenotype A (P = 0.045, Kaplan–Meier analysis). When adjusted for traditional risk factors (i.e. age, severity of illness, and duration of ICU stay), Phenotype B was independently associated with 1 year of mortality [adjusted hazard ratio = 2.83 (95% confidence interval 1.21–6.60); P = 0.016]. There was a significantly lower physical quality of life in Phenotype B patients at 3 months (i.e. SF-36 physical component score).
Conclusions
A phenotype with sustained inflammation, myocardial fibrosis, and endothelial dysfunction at ICU discharge was identified from readily available data and was independently associated with poor long-term outcomes in CS survivors.
Background
Improvements in cardiogenic shock (CS) management in the last few decades (i.e. broader early revascularization) decreased early mortality, thus increasing the number of CS survivors.1 Nonetheless, long-term mortality risk after CS persists for years with critical illness sequelae that impacts patients' quality of life.2 Attempts to implement preventive interventions to improve long-term outcomes are limited by an incomplete understanding of the late heterogeneous pathways of CS.3
Aims
The current study aims were to characterize the CS survivors underlying heterogeneity using a clustering approach (i.e. phenotyping).4-6 Accordingly, we applied latent class analysis (LCA) in a population of CS survivors [French and European Outcome Registry in Intensive Care Units (FROG-ICU) cohort]7 to identify distinct clinical phenotypes at intensive care unit (ICU) discharge, used host-response biomarkers to characterize them (i.e. pathway enrichment), and assessed their association with long-term outcomes.
Methods
A reanalysis of the prospective, observational, international FROG-ICU cohort (trial registration: NCT01367093) was performed. The original study design details were summarized in Supporting Information, Methods S1 and published previously.7, 8
Current reanalysis of the FROG-ICU cohort was performed in compliance with Unity Health Toronto (Toronto, Ontario, Canada) Research Ethics Board (No. 19-138), which conforms with the principles outlined in the Declaration of Helsinki.
The identification of CS patients was performed retrospectively in the FROG-ICU cohort based on the reported main cause of admission, clinical notes, and clinical, biological, and echocardiography data within the first 24 h after inclusion (flowchart, Supporting Information, Figure S1). The selected CS study population (n = 228) met the Society for Cardiovascular Angiography and Interventions (SCAI) definition of shock (SCAI shock stages C, D, and E).9 Among the identified CS population, 173 were discharged alive from the ICU and included in the current study. For CS survivors who had multiple admissions to ICU, only the first ICU admission was considered for reanalysis.
The primary outcome was 1 year of mortality after ICU discharge. Secondary outcomes were mortality 3 and 6 months after ICU discharge, readmissions within the first year after ICU discharge, and health-related quality of life assessed by the short form-36 questionnaire (SF-36) with its physical and mental component scores (PCS and MCS) within 1 year after ICU discharge.10
Fifteen readily available clinical and biological variables at ICU discharge were included in LCA based on the prior published literature (Supporting Information, Methods S1) and a consensus among three cardiology and critical care medicine experts: C. d. S., A. M., and P. L. (Supporting Information, Table S1).11, 12
Latent class analysis was used (R-package ‘depmixS4’, ‘mix’ function)13 to identify phenotypes of CS survivors independently of clinical outcome. The selection criteria of the optimal number of classes are based on both statistical and clinical criteria (detailed in Supporting Information, Methods S1).
Subsequently, basic characteristics and host-response biomarker (Supporting Information, Table S2) level comparisons between phenotypes were conducted. The associations between phenotypes and long-term outcomes were analysed (Supporting Information, Methods S1).
Results
Patients' characteristics are presented in Table 1. CS was due to ischaemic aetiology in 38% of the cases. One-year mortality after ICU discharge was 17.3% overall.
| All patients (n = 173) | Phenotype A (n = 108) | Phenotype B (n = 65) | P-value | |
|---|---|---|---|---|
| Age, yearsa | 61 [50–72] | 58 [49–71] | 64 [52–73] | 0.150 |
| Male gender, n (%) | 117 (67.6) | 73 (67.6) | 44 (67.7) | 1.000 |
| BMI, kg/m2a | 26 [23–29] | 25 [23–28] | 27 [24–29] | 0.224 |
| Comorbiditiesa | ||||
| Charlson age-comorbidity index | 2 [1–4] | 2 [0–4] | 3 [1, 5] | 0.007 |
| Diabetes mellitus, n (%) | 28 (16.2) | 13 (12.0) | 15 (23.1) | 0.090 |
| Chronic heart failure, n (%) | 16 (9.2) | 7 (6.5) | 9 (13.8) | 0.178 |
| Coronary artery disease, n (%) | 27 (15.6) | 12 (11.1) | 15 (23.1) | 0.060 |
| Hypertension, n (%) | 68 (39.3) | 40 (37.0) | 28 (43.1) | 0.531 |
| Chronic renal disease, n (%) | 24 (13.9) | 6 (5.6) | 18 (27.7) | <0.001 |
| COPD, n (%) | 9 (5.2) | 7 (6.5) | 2 (3.1) | 0.486 |
| Chronic liver disease, n (%) | 3 (1.7) | 2 (1.9) | 1 (1.5) | 1.000 |
| Active cancer, n (%) | 11 (6.4) | 7 (6.5) | 4 (6.2) | 1.000 |
| Organ dysfunction | ||||
| SAPS IIa | 59 [48–71] | 58 [48–68] | 59 [48–76] | 0.085 |
| SOFA at inclusion | 7 [5–9] | 6 [5–9] | 8 [5–9] | 0.285 |
| SOFA at ICU discharge | 0 [0–2] | 0 [0–2] | 1 [0–4] | 0.008 |
| Cerebral performance category > 3 at ICU discharge, n (%) | 3 (2.3) | 1 (1.2) | 2 (4.5) | 0.268 |
| SCAI shock stage, n (%)a | 0.103 | |||
| C | 122 (70.5) | 82 (75.9) | 40 (61.5) | |
| D | 27 (15.6) | 15 (13.9) | 12 (18.5) | |
| E | 24 (13.9) | 11 (10.2) | 13 (20.0) | |
| Admission diagnoses (not mutually exclusive) | ||||
| ACS, n (%) (n = 171) | 65 (38.0) | 48 (44.9) | 17 (26.6) | 0.026 |
| Prior CA, n (%) | 74 (42.8) | 55 (50.9) | 19 (29.2) | 0.008 |
| Prior OHCA, n (%) | 67 (38.7) | 50 (46.3) | 17 (26.2) | 0.013 |
| Echocardiographic data | ||||
| RV dysfunction, n (%)b | 11 (11.1) | 3 (5.7) | 8 (17.4) | 0.106 |
| LVEF (%) | 30 [20–50] | 32 [20–47] | 30 [20–50] | 0.974 |
| ICU stay and treatments/organ support | ||||
| Duration of ICU stay, days | 7 [5–13] | 6 [5–10] | 11 [6–18] | 0.001 |
| Mechanical ventilation, n (%)a | 149 (86.1) | 93 (86.1) | 56 (86.2) | 1.000 |
| PCI | 53 (31.0) | 40 (37.4) | 13 (20.3) | 0.030 |
| PCI in patients with ACS on admission (n = 65) | 52 (80.0) | 39 (81.2) | 13 (76.4) | 0.720 |
| Vasopressors/inotropes use, n (%)a | 148 (85.5) | 93 (86.1) | 55 (84.6) | 0.962 |
| IABP, n (%) | 10 (5.8) | 7 (6.5) | 3 (4.6) | 0.745 |
| ECLS/LVAD, n (%) | 17 (9.9) | 5 (4.6) | 12 (18.8) | 0.006 |
| RRT during ICU stay, n (%) | 32 (18.5) | 13 (12.0) | 19 (29.2) | 0.009 |
| Primary outcome | ||||
| One-year mortality, n (%) | 30 (17.3) | 14 (13.0) | 16 (24.6) | 0.050 |
| Secondary outcomes | ||||
| Rehospitalization at 3 months, n (%)c | 31 (31.0) | 23 (35.9) | 8 (22.2) | 0.231 |
| SF-36 PCS at 3 monthsd | 52 [30–70] | 60 [40–78] | 39 [20–52] | 0.006 |
| SF-36 MCS at 3 monthsd | 55 [35–77] | 63 [37–79] | 49 [32–57] | 0.068 |
| Mortality at 3 months, n (%)e | 17 (9.8) | 8 (7.4) | 9 (13.8) | 0.265 |
| Rehospitalization at 6 months, n (%)f | 34 (31.8) | 22 (31.0) | 12 (33.3) | 0.979 |
| SF-36 PCS at 6 monthsg | 52 [35–77] | 56 [36–85] | 50 [33–59] | 0.148 |
| SF-36 MCS at 6 monthsg | 57 [34–73] | 63 [36–79] | 43 [33–64] | 0.076 |
| Mortality at 6 months, n (%)e | 25 (14.5) | 11 (10.2) | 14 (21.5) | 0.067 |
| Rehospitalization at 12 months, n (%)h | 48 (40.0) | 30 (39.0) | 18 (41.9) | 0.907 |
| SF-36 PCS at 12 monthsi | 59 [36–86] | 61 [42–86] | 54 [31–75] | 0.124 |
| SF-36 MCS at 12 monthsj | 62 [42–81] | 65 [44–85] | 51 [39–76] | 0.111 |
- ACS, acute coronary syndrome; BMI, body mass index; CA, cardiac arrest; COPD, chronic obstructive pulmonary disease; ECLS, extracorporeal life support; IABP, intra-aortic balloon pump; ICU, intensive care unit; LVAD, left ventricular assist device; LVEF, left ventricular ejection fraction; MCS, mental component score; OHCA, out-of-hospital cardiac arrest; PCI, percutaneous coronary intervention; PCS, physical component score; RRT, renal replacement therapy; RV, right ventricular; SAPS II, Simplified Acute Physiologic Score II; SCAI, Society for Cardiovascular Angiography and Interventions; SF-36, short form-36 questionnaire; SOFA, Sequential Organ Failure Assessment.
- Continuous variables were expressed as median (interquartile range) and compared with the Mann–Whitney U test. Categorical variables were expressed as numbers (percentages) and were compared with the Fisher exact test or the χ2 test as appropriate. Primary outcome is presented at 1 year after ICU discharge. Secondary outcomes are presented at 3, 6, and 12 months after ICU discharge. A higher SF-36 score indicated a better mental and physical function.
- a At inclusion.
- b RV dysfunction was defined as an RV enlargement associated or not with a systolic dysfunction as assessed by echocardiography on admission.
- c Values calculated for 100 patients.
- d Values calculated for 73 patients.
- e After ICU discharge.
- f Values calculated for 107 patients.
- g Values calculated for 74 patients.
- h Values calculated for 120 patients.
- i Values calculated for 76 patients.
- j Values calculated for 75 patients.
A two-class LCA model was selected as the optimal fit clustering solution for our population in all the imputed datasets. Correlation coefficients (Spearman) between the variables included in the LCA model are presented in Supporting Information, Figure S2.
At ICU discharge, 108 patients (62.4%) were assigned to Phenotype A and 65 patients (37.6%) were assigned to Phenotype B. The mean (standard deviation) posterior class-membership probability (i.e. the probability to belong to the assigned phenotype) was 0.94 (0.12) for Phenotypes A and B, suggesting that the two phenotypes are well separated.
The phenotype characteristics and outcomes are summarized in Table 1 and Supporting Information, Table S3. Standardized mean difference plot of phenotype-defining variables is shown in Figure 1.
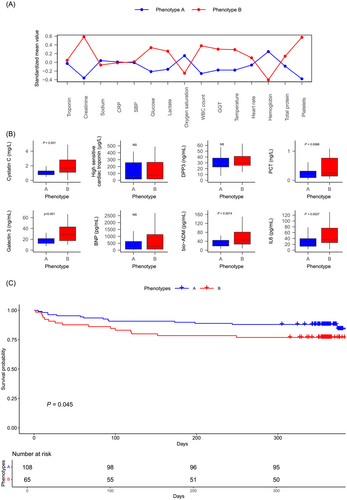
When comparing host-response biomarkers at ICU discharge, patients in Phenotype B demonstrated sustained elevation in levels of markers of inflammation (procalcitonin and interleukin-6), endothelial dysfunction (bio-adrenomedullin), myocardial fibrosis (galectin 3), and renal dysfunction (plasmatic cystatin C) compared with Phenotype A (Figure 1). Differences in biomarker levels persisted after subgroup analysis stratified by age terciles, SCAI shock stage, and cause of CS (ischaemic vs. non-ischaemic origin) (Supporting Information, Figures S3–S5).
Cardiogenic shock survivors in Phenotype B had higher 1 year of mortality [Table 1 and Supporting Information, Figure S3; P (log-rank test) = 0.045]. In a Cox model adjusted for confounders (age, severity of illness, and duration of ICU stay), membership in Phenotype B at ICU discharge was independently associated with 1 year of mortality [adjusted hazard ratio = 2.83 (95% confidence interval 1.21–6.60); P = 0.016] (Supporting Information, Table S4). There was a significant difference in the SF-36 PCS between the two phenotypes at 3 months (i.e. lower physical quality of life in Phenotype B patients) (Table 1).
Conclusions
A phenotype with persistent elevation in circulating markers of inflammation, myocardial fibrosis, and endothelial dysfunction at ICU discharge was identified using readily available data in CS survivors. While selection bias is a potential limitation of this study (mostly tertiary centres), these result strongly suggest that heterogeneity exists within the CS-survivor population with different underlying late host-response patterns and long-term outcomes.14
Previous studies have used a phenotyping approach including variables measured on admission to identify CS clinical phenotypes.11, 15, 16 While most of these studies have focused on short-term survival after CS, long-term survival and quality of life are important patient-centred outcomes.14, 17
Zweck et al. used consensus k-means clustering to identify three clinical phenotypes on admission in CS patients with different early outcomes.11, 15 The same three CS phenotypes were replicated by Jentzer et al., with differences in 1 year of mortality observed between phenotypes.16 In contrast to previous studies, our analysis examined host-response biomarkers that provide novel insights into the underlying pathophysiological processes.
The identification of clinical phenotypes at ICU discharge may allow for a better understanding of late host response in stabilized CS patients. This approach may increase the probability of identifying a treatment benefit (e.g. inflammation/endothelium modulation) and follow-up strategy for each given phenotype.18, 19
Relevant limitations of our study include its observational design that precluded causal inference and the absence of replication in an external cohort. Nonetheless, large CS cohorts with clinical and biomarker data at ICU discharge were not available for external validation.
Future adaptive trials using phenotype-based intervention should be designed to allow for a more effective identification of therapeutic/prevention strategies to improve long-term outcome in CS survivors.14, 20
Acknowledgements
We are very thankful for the FROG-ICU network and all our collaborators who contributed to set up this research project.
Conflict of interest
None of the authors of this paper has a financial or personal relationship with other persons or organizations that could inappropriately influence or bias the content of the paper. Dr P.R.L. has received unrelated research funding from the Canadian Institutes of Health Research, the U.S. National Institutes of Health (National Heart, Lung, and Blood Institute), the Peter Munk Cardiac Centre, the LifeArc Foundation, the Thistledown Foundation, the Ted Rogers Centre for Heart Research, the Medicine by Design Fund, the University of Toronto, and the Government of Ontario. He also received unrelated consulting honoraria from Novartis, Corrona, and Brigham and Women's Hospital, as well as unrelated royalties from McGraw-Hill Publishing. Dr A.M. has received speaker's honoraria from Abbott (Chicago, Illinois), Orion (Auckland, New Zealand), Roche (Basel, Switzerland), and Servier (Suresnes, France) and fees as a member of the advisory boards and/or steering committees and/or research grants from BMS (New York, New York), Adrenomed (Hennigsdorf, Germany), Neurotronik (Durham, North Carolina), Roche (Basel, Switzerland), Sanofi (Paris, France), Sphingotec (Hennigsdorf, Germany), Novartis (Basel, Switzerland), Otsuka (Chiyoda City, Tokyo, Japan), Philips (Amsterdam, Netherlands), and 4TEEN4 (Hennigsdorf, Germany). Dr E.G. received fees as a member of the advisory boards and/or steering committees and/or from research grants from Magnisense (Paris, France), Adrenomed (Hennigsdorf, Germany), and Deltex Medical (Chichester, UK). The remaining authors declare no competing interests.
Funding
The original FROG-ICU (ClinicalTrials.gov Identifier NCT01367093) was supported by the Programme Hospitalier de la Recherche Clinique (AON 10-216) and by a research grant from the Société Française d'Anesthésie–Réanimation (design of the study, sample collection, and collection, analysis, and interpretation of data). Dr Sabri Soussi was awarded the Canadian Institutes of Health Research (CIHR) Doctoral Foreign Study Award (DFSA) and the Merit Awards Program (Department of Anesthesiology and Pain Medicine, University of Toronto, Canada) for the current study.