Impact of beta-blocker use on the long-term outcomes of heart failure patients with chronic obstructive pulmonary disease
Abstract
Aims
The number of patients with both chronic obstructive pulmonary disease (COPD) and heart failure (HF) is increasing in Asia, and these conditions often coexist. We previously revealed a tendency of beta-blocker underuse among patients with HF with reduced ejection fraction (HFrEF) and COPD in Asian countries other than Japan. Here, we evaluated the impact of cardio-selective beta-blocker use on the long-term outcomes of patients with HF and COPD.
Methods and results
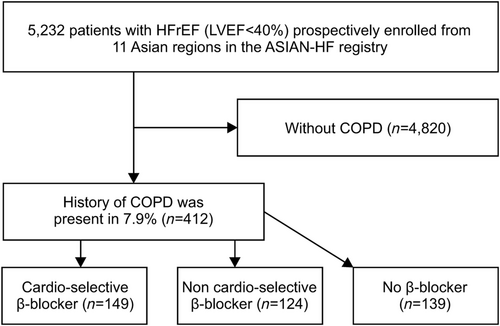
Among the 5232 patients with HFrEF (left ventricular ejection fraction of <40%) prospectively enrolled from 11 Asian regions in the ASIAN-HF registry, 412 (7.9%) had a history of COPD. We compared the clinical characteristics and long-term outcomes of the patients with HF and COPD according to the use and type of beta-blockers used: cardio-selective beta-blockers (n = 149) vs. non-cardio-selective beta-blockers (n = 124) vs. no beta-blockers (n = 139). The heart rate was higher, and the outcome was poorer in the no beta-blocker group than in the beta-blocker groups. The 2 year all-cause mortality was significantly lower in the non-cardio-selective beta-blocker group than in the no beta-blocker group. Further, the cardiovascular mortality significantly decreased in the non-cardio-selective beta-blocker group before (hazard ratio: 0.36; 95% confidence interval: 0.18–0.73; P = 0.004) and after adjustments (hazard ratio: 0.37; 95% confidence interval: 0.19–0.73; P = 0.005), but not in the cardio-selective beta-blocker group.
Conclusions
Beta-blockers reduced the all-cause mortality of patients with HFrEF and COPD after adjusting for age and heart rate, although the possibility of selection bias could not be completely excluded due to multinational prospective registry.
Introduction
In Asia, the increase in the prevalence of patients with congestive heart failure (CHF) constitutes a medical and financial burden on the society.1 Chronic obstructive pulmonary disease (COPD) is a common co-morbidity that worsens the clinical course of CHF and considerably impacts its therapeutic management and prognosis.2, 3 Beta-blockers, which are recommended by international guidelines for the first-line treatment of heart failure (HF),4-6 are often avoided in patients with CHF and COPD because of concerns regarding precipitating respiratory deterioration.3, 7-10 However, several guidelines state that COPD is not a contraindication for the use of beta-blockers, as it indeed reduces all-cause mortality in patients with HF and COPD.11, 12 Cardio-selective beta-blockers are usually recommended to avoid bronchospasm or attenuation of the benefit of inhaled β2 agonists; however, previous studies have revealed no association between selectivity and outcomes.3, 12-14
Nevertheless, the impact of cardio-selective beta-blocker use on long-term outcomes has not been sufficiently evaluated in Asian patients with CHF and COPD. The ASIAN-HF registry offers a unique opportunity to investigate the impact of beta-blocker selectivity from a multinational perspective. Thus, this study evaluated the impact of cardio-selective beta-blocker use on the long-term outcomes of patients with CHF and COPD.
Methods
Study design
The ASIAN-HF registry is a prospective observational registry of symptomatic patients with HF with reduced ejection fraction (HFrEF) from 44 centres in 11 Asian regions (China, Hong Kong, India, Indonesia, Japan, Korea, Malaysia, Philippines, Singapore, Taiwan, and Thailand), which enrolled patients between 2010 and 2015. Detailed methods were published previously.15 For this study, patients from the ASIAN-HF registry with both HF and COPD were identified, and health data, including vital signs and other diagnosed illnesses, were analysed. Heart rate was measured at rest using electrocardiography. Hypertension was defined as the presence of a clinical diagnosis of hypertension (blood pressure ≥140/90 mmHg) or treatment with antihypertensive medications. Diabetes was defined as the presence of a clinical diagnosis of diabetes (fasting plasma glucose level ≥7 mmol/L, random plasma glucose level ≥11.1 mmol/L, or HbA1c level ≥6.5%) or treatment with anti-diabetic therapy. COPD was diagnosed in accordance with the Global Initiative for Chronic Obstructive Lung Disease criteria.16 The use of beta-blockers was evaluated at the study registration.
Population selection
Among the 5232 patients with HFrEF (left ventricular ejection fraction <40%) prospectively enrolled from the 11 Asian regions in the ASIAN-HF registry, 412 (7.9%) had a history of COPD. We compared the clinical characteristics and long-term outcomes of the patients with HF and COPD according to the use and type of beta-blockers used: cardio-selective beta-blockers (n = 149) vs. non-cardio-selective beta-blockers (n = 124) vs. no beta-blockers (n = 139) (Figure 1).
Primary endpoint
The primary endpoint was all-cause mortality among the cardio-selective beta-blocker, non-cardio-selective beta-blocker, and no beta-blocker groups.
Secondary endpoints
The secondary endpoints were cardiovascular (CV) mortality and rehospitalization for HF among the cardio-selective beta-blocker, non-cardio-selective beta-blocker, and no beta-blocker groups.
Ethical approval/informed consent
Ethical approval was obtained from the local institutional review board of each participating centre, and the investigation conformed to the principles outlined in the Declaration of Helsinki. All subjects provided written informed consent to participate in the study.
Statistical analysis
The primary analysis involved the evaluation of the association of beta-blocker use with 2 year all-cause mortality in patients with HFrEF and COPD. Kaplan–Meier curves of the clinical outcomes were evaluated for cumulative survival rate over time among the cardio-selective beta-blocker, non-cardio-selective beta-blocker, and no beta-blocker groups. Cox regression was used to assess the hazard ratios (HRs) for the association of beta-blocker use with mortality.
The secondary analysis involved the evaluation of the association of beta-blocker use with 2 year rehospitalization or 2 year CV mortality in patients with HFrEF and COPD. Continuous variables were expressed as means ± standard deviations and categorical variables as numbers (percentages). To compare the baseline characteristics among patients with HF and COPD, we used χ2 tests and independent t-tests for categorical and continuous variables, respectively.
A P-value ≤0.05 was considered statistically significant. Stata software Version 14 (StataCorp., College Station, TX) was used for the statistical analyses.
Results
Clinical characteristics
The registry included 5232 patients with HFrEF (left ventricular ejection fraction <40%) prospectively enrolled from the 11 Asian regions. The physician-reported COPD prevalence was 7.9% (n = 412) in this cohort of patients. Among the patients with HFrEF and COPD, 36% (n = 149) received cardio-selective beta-blockers, 30% (n = 124) received non-cardio-selective beta-blockers, and 34% (n = 139) received no beta-blockers (Figure 1). Table 1 shows the main clinical characteristics of the patients with HFrEF and COPD who received cardio-selective and non-cardio-selective beta-blockers and no beta-blockers at study entry. The patients who received beta-blockers were younger (no beta-blockers: 66.8 ± 12.7 years; non-cardio-selective beta-blockers: 61.4 ± 14.4 years; and cardio-selective beta-blockers: 63.3 ± 13.6 years, P = 0.005) and had a lower heart rate (no beta-blockers: 83.8 ± 15.9 b.p.m.; non-cardio-selective beta-blockers: 77.2 ± 14.2 b.p.m.; and cardio-selective beta-blockers: 79.0 ± 14.0 b.p.m., P < 0.001) than the patients who did not receive beta-blockers (Table 1). The patients who received cardio-selective beta-blockers had a larger left atrial volume and higher use of implantable cardioverter-defibrillator or cardiac resynchronization therapy than those who received non-cardio-selective beta-blockers.
| Characteristics | Beta-blocker use | P-value | ||
|---|---|---|---|---|
| None (N = 139) | Non-cardio-selective (N = 124) | Cardio-selective (N = 149) | ||
| Age (years) | 66.8 (12.7) | 61.4 (14.4) | 63.3 (13.6) | 0.005 |
| Women | 26 (18.7%) | 27 (21.8%) | 27 (18.1%) | 0.720 |
| Enrolled as inpatient | 75 (54.0%) | 62 (50.4%) | 81 (54.4%) | 0.780 |
| BMI (kg/m2) | 24.3 (4.6) | 25.3 (6.2) | 24.7 (6.9) | 0.450 |
| Heart rate (b.p.m.) | 83.8 (15.9) | 77.2 (14.2) | 79.0 (14.0) | <0.001 |
| Systolic BP (mmHg) | 118.8 (17.1) | 121.5 (18.9) | 117.9 (20.1) | 0.260 |
| Diastolic BP (mmHg) | 71.5 (12.3) | 71.7 (12.2) | 70.6 (11.8) | 0.750 |
| NYHA Class III/IV | 54 (43.6%) | 44 (40.0%) | 68 (48.9%) | 0.359 |
| Coronary artery disease | 72 (51.8%) | 58 (46.8%) | 71 (47.7%) | 0.680 |
| Atrial fibrillation/flutter | 21 (15.1%) | 22 (17.7%) | 37 (24.8%) | 0.097 |
| Hypertension | 81 (58.3%) | 73 (58.9%) | 75 (50.3%) | 0.270 |
| Diabetes | 64 (46.0%) | 44 (35.5%) | 51 (34.2%) | 0.084 |
| History of hospitalization for HF | 82 (59.0%) | 90 (72.6%) | 110 (73.8%) | 0.020 |
| eGFR (mL/min/1.73 m2) | 57.5 (42.9–73.5) | 65.4 (43.2–85.6) | 62.2 (43.6–83.0) | 0.210 |
| CKD (eGFR of <60 mL/min/1.73 m2) | 59 (52.7%) | 46 (40.0%) | 64 (48.1%) | 0.150 |
| LVEF (%) | 27.9 (7.2) | 27.5 (7.5) | 27.9 (6.8) | 0.870 |
| LV end-diastolic volume (mL) | 171.3 (66.5) | 190.5 (76.6) | 183.7 (87.9) | 0.245 |
| LV end-systolic volume (mL) | 124.0 (56.4) | 139.9 (68.3) | 134.7 (75.7) | 0.269 |
| LA volume (mL) | 65.0 (32.0) | 72.6 (30.4) | 89.8 (41.6) | <0.001 |
| ACE inhibitor or ARB | 95 (68.3%) | 94 (75.8%) | 103 (69.1%) | 0.350 |
| MRA | 65 (54.2%) | 49 (53.8%) | 97 (65.1%) | 0.110 |
| Diuretics | 115 (82.7%) | 96 (77.4%) | 119 (79.9%) | 0.557 |
| ICD/pacemaker/CRT | 13 (9.4%) | 31 (25.0%) | 39 (26.2%) | <0.001 |
| ICD/CRT | 12 (8.6%) | 27 (21.8%) | 38 (25.5%) | 0.003 |
- ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; BMI, body mass index; BP, blood pressure; CKD, chronic kidney disease; CRT, cardiac resynchronization therapy; eGFR, estimated glomerular filtration rate; HF, heart failure; ICD, implantable cardioverter-defibrillator; LA, left atrial; LV, left ventricular; LVEF, left ventricular ejection fraction; MRA, mineralocorticoid receptor antagonist; NYHA, New York Heart Association.
- Data are presented as numbers of cases and relative percentages of the group's total in parentheses, except for eGFR presented as a median with inter-quartile range in parentheses; admission age, BMI, heart rate, systolic and diastolic BPs, LVEF, LV end-diastolic/systolic volumes, and LA volume are presented as a mean with standard deviation in parentheses.
Association of beta-blocker use with all clinical outcomes
The analysis of the 2 year composite outcomes is shown in Table 2. Regarding all-cause mortality, we observed a significant decrease in the HR in the patients treated with beta-blockers before [HR: 0.54; 95% confidence interval (CI): 0.34–0.86; P = 0.009] and after adjustments (HR: 0.48; 95% CI: 0.30–0.78; P = 0.003) (Table 3). Similarly, the Kaplan–Meier curve analysis showed a significant difference in the all-cause mortality among the three groups (log-rank P = 0.008, Figure 2). We then compared the 2 year all-cause mortality among the three groups and found a significant decrease in the group treated with non-cardio-selective beta-blockers before (HR: 0.39; 95% CI: 0.21–0.72; P = 0.003) and after adjustments (HR: 0.37; 95% CI: 0.19–0.70; P = 0.002) (Table 3). We also observed no association between beta-blocker treatment and 2 year HF rehospitalization (Table 3).
| N | n (%) | Crude HR (95% CI) | P-value | Adjusteda HR (95% CI) | P-value | |
|---|---|---|---|---|---|---|
| Any beta-blockers | ||||||
| None | 121 | 48 (39.7%) | 1.0 (ref) | 1.0 (ref) | ||
| Yes | 254 | 91 (35.8%) | 0.81 (0.57–1.15) | 0.237 | 0.83 (0.57–1.20) | 0.316 |
| Cardio-selective beta-blockers | ||||||
| None | 121 | 48 (39.7%) | 1.0 (ref) | 1.0 (ref) | ||
| Non-cardio-selective | 115 | 39 (33.9%) | 0.74 (0.48–1.13) | 0.162 | 0.79 (0.51–1.23) | 0.306 |
| Cardio-selective | 139 | 52 (37.4%) | 0.87 (0.59–1.29) | 0.494 | 0.86 (0.57–1.29) | 0.455 |
- BMI, body mass index; BP, blood pressure; CI, confidence interval; COPD, chronic obstructive pulmonary disease; HFrEF, heart failure with reduced ejection fraction; HR, hazard ratio; N, no. of patients with HFrEF and COPD; n, no. of patients with HFrEF and COPD who experienced a composite event in 2 years.
- The crude and adjusted HRs for age, sex, BMI, systolic BP, and heart rate were calculated in reference to the group that did not receive beta-blockers. Data are presented as numbers of cases and relative percentages of the group's total in parentheses or as HRs with 95% CIs in parentheses.
- a Adjusted for age, sex, BMI, systolic BP, and heart rate.
| 2 year all-cause mortality | 2 year HF rehospitalization | 2 year CV mortality | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | Crude HR (95% CI) | P-value | Adjusteda HR (95% CI) | P-value | n (%) | Crude HR (95% CI) | P-value | Adjusteda HR (95% CI) | P-value | n (%) | Crude HR (95% CI) | P-value | Adjusteda HR (95% CI) | P-value | |
| Any beta-blockers | |||||||||||||||
| None | 33 (27.3%) | 1.0 (ref) | 1.0 (ref) | 26 (21.5%) | 1.0 (ref) | 1.0 (ref) | 28 (23.1%) | 1.0 (ref) | 1.0 (ref) | ||||||
| Yes | 42 (16.5%) | 0.54 (0.3–0.86) | 0.009 | 0.48 (0.30–0.78) | 0.003 | 62 (24.4%) | 1.1 (0.6–1.75) | 0.686 | 1.18 (0.72–1.93) | 0.523 | 36 (14.2) | 0.56 (0.3–0.91) | 0.021 | 0.53 (0.31–0.88) | 0.015 |
| Cardio-selective beta-blockers | |||||||||||||||
| None | 33 (27.3%) | 1.0 (ref) | 1.0 (ref) | 26 (21.5%) | 1.0 (ref) | 1.0 (ref) | 28 (23.1%) | 1.0 (ref) | 1.0 (ref) | ||||||
| Non-cardio-selective | 14 (12.2%) | 0.39 (0.2–0.72) | 0.003 | 0.37 (0.19–0.70) | 0.002 | 29 (25.2%) | 1.13 (0.66–1.92) | 0.65 | 1.26 (0.71–2.23) | 0.424 | 11 (9.6%) | 0.36 (0.1–0.73) | 0.004 | 0.37 (0.19–0.73) | 0.005 |
| Cardio-selective | 28 (20.1%) | 0.68 (0.4–1.13) | 0.139 | 0.58 (0.34–0.99) | 0.044 | 33 (23.7%) | 1.07 (0.6–1.80) | 0.786 | 1.11 (0.65–1.92) | 0.697 | 25 (18.0%) | 0.73 (0.4–1.26) | 0.258 | 0.66 (0.37–1.17) | 0.155 |
- BMI, body mass index; BP, blood pressure; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CV, cardiovascular; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; HR, hazard ratio; n, no. of patients with HFrEF and COPD who experienced an event in 2 years.
- The crude and adjusted HRs for age, sex, BMI, systolic BP, and heart rate were calculated in reference to the group that did not receive beta-blockers. The HR was calculated for the 2 year all-cause mortality, HF rehospitalization, and CV mortality. Data are presented as numbers of cases and relative percentages of the group's total in parentheses or as HRs with 95% CIs in parentheses.
- a Adjusted for age, sex, BMI, systolic BP, and heart rate.
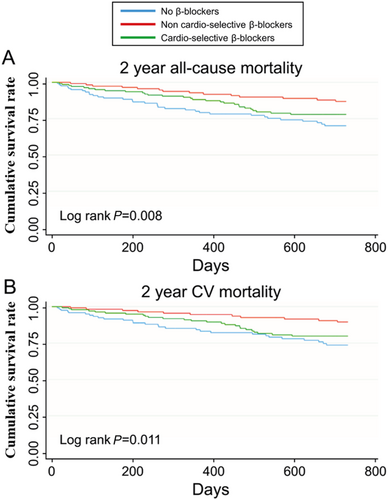
Regarding CV mortality, we observed a significant decrease in the HR in the patients treated with beta-blockers before (HR: 0.56; 95% CI: 0.34–0.91; P = 0.021) and after adjustments (HR: 0.53; 95% CI: 0.31–0.88; P = 0.015) (Table 3). This result was corroborated by the Kaplan–Meier curve analysis in which a significant difference in the CV mortality among the three groups (log-rank P = 0.011, Figure 2) was demonstrated. Further, there was a significant decrease in the CV mortality in the group treated with non-cardio-selective beta-blockers before (HR: 0.36; 95% CI: 0.18–0.73; P = 0.004) and after adjustments (HR: 0.37; 95% CI: 0.19–0.73; P = 0.005) (Table 3). For the patients treated with cardio-selective beta-blockers, no significant difference was observed (Table 3).
Dosage of beta-blockers
We then evaluated the beta-blockers used for the treatment of patients with HFrEF and COPD. The cardio-selective beta-blockers were bisoprolol (70.5%), metoprolol (24.5%), and nebivolol (5%), whereas the non-cardio-selective beta-blockers used were carvedilol (69.6%) and others (30.4%). The dosages of these drugs were low, as the median dosage was 25% of the dosage recommended by the guidelines for bisoprolol, metoprolol, and carvedilol and 50% for nebivolol (Supporting Information, Table S1). In a stratified analysis of the patients with carvedilol or bisoprolol, benefits were derived from taking either carvedilol or bisoprolol (Supporting Information, Table S2).
Factors impacting 2 year all-cause mortality
The factors impacting 2 year all-cause mortality were investigated using a multivariate logistic regression analysis. After adjustment for age, enrolment type, and beta-blocker use, we found that 2 year all-cause mortality was significantly increased in the patients with chronic kidney disease (HR: 1.80; 95% CI: 1.07–3.02; P = 0.027) (Supporting Information, Table S3). Conversely, 2 year all-cause mortality was significantly decreased among the Japanese/Korean patients (reference: Chinese patients; HR: 0.14; 95% CI: 0.04–0.45; P = 0.001), outpatients (HR: 0.36; 95% CI: 0.22–0.61; P < 0.001), patients with a higher body mass index (HR: 0.92; 95% CI: 0.87–0.98; P = 0.007), and patients treated with angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) (HR: 0.62; 95% CI: 0.39–0.99; P = 0.044) (Supporting Information, Table S3).
Discussion
The analysis of the multinational ASIAN-HF registry data revealed underuse of beta-blockers, with approximately 60% of patients with HFrEF and COPD treated compared with 80% of those without COPD.3 In the present analysis, we evaluated the impact of non-selective and cardio-selective beta-blocker use on the long-term outcomes of patients with HFrEF and COPD. We found that the baseline age and heart rate were lower in the patients receiving beta-blockers than in those not receiving beta-blockers and that beta-blockers reduced the all-cause mortality of patients with HFrEF and COPD after adjusting for age and heart rate. The observed efficiency of beta-blockers was achieved even with a low dosage in patients with COPD.
Treatment of patients with heart failure with reduced ejection fraction and chronic obstructive pulmonary disease
The high prevalence of smoking, coupled with the ageing population and increased levels of air pollution in Asia, threatens to further increase the burden of COPD.17-19 Numerous studies have shown that COPD frequently coexists with CHF, worsens the clinical course of the disease, and considerably impacts its therapeutic management and prognosis.2, 3, 20-24 Although recent guidelines have stated that COPD is not a contraindication for the use of beta-blockers, its use indeed reduces the all-cause mortality in patients with HF and COPD11, 12, 25, 26; patients with HF and COPD still do not receive such medications because of safety concerns, which are not justified in most cases. Because of concern regarding respiratory deterioration, the presence of COPD is an important cause of the underuse of beta-blockers.3 Cardio-selective beta-blockers are usually recommended to avoid attenuation of the benefit of inhaled β2 agonists27; however, previous studies have revealed no association between selectivity and outcomes.3, 12-14 Moreover, in a previous study, we reported that beta-blockers, including non-cardio-selective beta-blockers, reduce mortality, thereby supporting their use in patients with HF and COPD.11 In this study, we provide evidence that non-cardio-selective beta-blockers decrease all-cause mortality in patients with HF and COPD. This result contradicts that of a previous study in which it was demonstrated that the use of non-cardio-selective beta-blockers should be avoided in patients with COPD.27-29 One possible explanation is that in the cohort of patients in the ASIAN-HF registry, the dosages of both cardio-selective and non-cardio-selective beta-blockers were lower than those recommended by the guidelines. Beta-blockers have a cardioprotective effect through reduced heart rate, sympathetic activity, and reverse remodelling.13, 14 Therefore, we propose that a low dosage of non-cardio-selective beta-blockers is beneficial for reducing mortality in patients with HF and COPD. Notably, beta-blockers reduced all-cause mortality and CV mortality to a similar extent, suggesting that the reduction of all-cause mortality results from a decrease in CV mortality. Unexpectedly, we observed that the 2 year mortality decreased in patients with a high body mass index. This result could be considered an illustration of the obesity paradox regarding CV diseases.30 The current study revealed that the use of ACE inhibitors or ARBs is associated with a reduction in 2 year mortality. We previously showed that these drugs were underused in this cohort.3 The use of ACE inhibitors or ARBs might be determined by the treating physicians because renal artery stenosis was significantly higher in the COPD group than in the non-COPD group.3 This result advocates a more aggressive use of not only beta-blockers but also ACE inhibitors or ARBs as much as possible among patients with both HFrEF and COPD. The 2 year all-cause mortality was significantly decreased among Japanese/Korean patients. Among the Japanese cohort, the use of beta-blockers was remarkably higher (95.2%) and the average heart rate was lower than that of registry patients with other ethnicities.3 This study is novel in that we demonstrated that beta-blockers reduced all-cause mortality and CV death in Asian patients with both HFrEF and COPD. However, this study was based on a multinational prospective registry; therefore, further studies are needed to confirm whether cardio-selective beta-blockers affect all-cause mortality in patients with HFrEF and COPD.
Strengths and limitations
The present results are based on a large contemporary multinational prospective registry; the study was specifically designed to collect detailed 2 year outcomes in hospitalized and ambulatory patients with HF across Asia. Nevertheless, several limitations associated with the present study warrant consideration. The baseline registry data were cross-sectional, and we were unable to exclude the possibility of selection bias. Bias is inevitable in the selection of sites in each region, and the willingness of patients to participate in a prospective protocol influences enrolment. Furthermore, the use of beta-blockers was left to the discretion of the treating physicians, and the COPD grades and medications for COPD were unclear; thus, patients who received cardio-selective beta-blockers might have had more progressed COPD and more severe HF. Importantly, we were unable to include COPD exacerbation as an event. This might have diminished the identification of the deleterious effect of non-cardio-selective beta-blockers on adverse events, including on respiratory function. The definitions of events in this study excluded left ventricular assist device implantation and cardiac transplantation. Additionally, this was a relatively small observational study with a non-randomized design. Prospective randomized trials that compare cardio-selective and non-cardio-selective beta-blockers in patients with COPD are needed.
Conclusions
Beta-blockers reduced the all-cause mortality of patients with HFrEF and COPD after adjusting for age and heart rate. This analysis of the ASIAN-HF registry data advocates a more aggressive use of beta-blockers among patients with HFrEF and COPD.
Acknowledgements
We would like to acknowledge the ASIAN-HF Executive Committee. The current site investigators of the ASIAN-HF study are the following: Ruijin Hospital, Shanghai Jiaotong University School of Medicine: Liqun Wu; Fuwai Hospital: Shu Zhang; Jiangsu Province People's Hospital: Xinli Li; Zhongshan Hospital Fudan University: Yangang Su (China). The Chinese University of Hong Kong: Cheuk Man Yu (Hong Kong). Sir Gangaram Hospital: Jitendra Sawhney; West Fort Hi-Tech Hospital Ltd.: Mohanan Padinhare Purayil; Dayanand Medical College and Hospital: Gurpreet Singh Wander; Medanta The Medicity: Vijay Chopra; Care Institute of Medical Sciences: Ajay Naik; Care Hospital: Narasimhan Calambur (India). Rumah Sakit Khusus Jantung Binawaluya: Muhammad Munawar; Rumah Sakit Hasan Sadikin: Pintoko Tedjokusumo; Harapan Kita National Cardiovascular Center: Bambang Budi Siswanto; Siloam Karawaci Hospital: Antonia A. Lukito (Indonesia). Korea University Anam Hospital: Jaemin Shim; Korea University Guro Hospital: Jin Oh Na; Severance Hospital, Yonsei University Health System: Boyoung Joung; Chonnam National University Hospital: Hyung-Wook Park; Hyewon Medical Foundation SeJong General Hospital: Suk Keun Hong; Korea University Ansan Hospital: Seong Hwan Kim (Korea). Institut Jantung Negara: Razali Omar; University Malaya Medical Centre: Imran Zainal Abidin; Hospital Queen Elizabeth II: Houng Bang Liew; Sarawak General Hospital: Tiong Kiam Ong (Malaysia). Philippine Heart Center: Eleanor Lopez; Makati Medical Center: Raul Lapitan; Manila Doctors Hospital: Eugenio Reyes (Philippines). National Heart Centre: Carolyn S.P. Lam; Kheng Leng David Sim; Tan Tock Seng Hospital: Poh Shuan Daniel Yeo; Changi General Hospital-Parent: Kui Toh Gerard Leong; Singapore General Hospital-Parent: Fazlur Rehman Jaufeerally; Khoo Teck Puat Hospital: Hean Yee Ong (Singapore). Mackay Memorial Hospital: Chung-Lieh Hung; National Taiwan University Hospital: Juey-Jen Hwang; Taipei Veterans General Hospital: Wen-Chung Yu; China Medical University Hospital: Hsin-Yueh Liang (Taiwan). Phramongkutklao Hospital: Waraporn Tiyanon; Maharaj Nakorn Chiang Mai Hospital: Wanwarang Wongcharoen; Ramathibodi Hospital: Tachapong Ngarmukos (Thailand). National Cerebral and Cardiovascular Center: Ikutaro Nakajima, Mitsuru Wada, and Kohei Ishibashi; Tokyo Women's Medical University: Takeshi Suzuki; Toho University Omori Medical Center: Shunsuke Kiuchi and Takayuki Kabuki; Nippon Medical School Hospital: Koji Murai (Japan). Editorial support, in the form of medical writing, assembling tables, and creating high-resolution images based on the authors' detailed directions, collating author comments, copyediting, fact checking, and referencing, was provided by Editage, Cactus Communications.
Conflict of interest
T.I. has received grant support through his institution from Daiichi Sankyo and honoraria for lectures from Ono Pharmaceutical, Bayer Healthcare, and Bristol Myers Squibb. N.H. reports grants from Daiichi Sankyo Company, Limited and grants from Nippon Boehringer Ingelheim Co., Ltd, during the conduct of the study. The rest of the authors declare no conflicts of interest.
Funding
This work was supported by the Investigator-Sponsored Research Program of Boston Scientific Corporation, via a competitive grant for investigator-initiated studies awarded to the Cardiovascular Research Institute, Singapore. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.