Predicting the clinical course in hypertrophic cardiomyopathy using thallium-201 myocardial scintigraphy
Abstract
Aims
This study aimed to evaluate the changes in left ventricular remodelling with time in patients with hypertrophic cardiomyopathy (HCM) using thallium-201 myocardial scintigraphy.
Methods and results
Forty-eight patients with HCM participated in the study. The extent score (ES) and a newly devised index termed the ‘mean count change’ (MCC) were used to evaluate the myocardial perfusion defects. Using the amount of thallium-201 uptake (TU), MCC (%) was calculated using the following formula: (last TU − initial TU)∕initial TU × 100. To confirm the site of the lesion, the left ventricle was divided into five segments: anterior, septal, inferior, lateral, and apex. Cardiovascular complications and deaths were recorded. The mean follow-up period was 8.6 ± 2.0 years. ES increased from 17.4 ± 13.7% to 44.0 ± 22.3% (P < 0.0001). MCC increased from 0% to 12.0 ± 9.0% (P < 0.0001). The apex was the most frequent site of lesion. Twenty-seven patients (56.3%) had experienced left ventricular heart failure (LVHF). Both ES and MCC were greater in patients with LVHF than in those without LVHF. An overlap between the two groups was greater in ES than in MCC. Patients with LVHF had a higher incidence of atrial fibrillation and apoplexy. Nineteen patients (39.6%) died during the study period; 14 died from LVHF, 3 from sudden cardiac death, and 2 from cancer.
Conclusions
Thallium-201 myocardial scintigraphy is useful for detecting the severity of myocardial damage and for confirming the lesion site in patients with HCM. MCC may be superior to ES in the evaluation of these changes with time.
Introduction
Sudden cardiac death (SCD) and left ventricular heart failure (LVHF) are two major causes of death in patients with hypertrophic cardiomyopathy (HCM). A genetically transmitted myocardial defect such as hypertrophied and disorganized cardiac muscle cells1 may be the cause of SCD. Left ventricular (LV) hypertrophy is known to be accompanied by progressive myocardial ischaemia.2 Chronic myocardial ischaemia appears to be associated with progressive myocardial cell death, resulting in LVHF in patients with HCM.3
Thallium-201 single-photon emission computed tomography (SPECT) is known to sensitively detect myocardial viability and can clearly indicate the lesion site.4 It is also reported that in patients with HCM, myocardial viability is associated with a regional perfusion defect in thallium-201 SPECT.5 However, to the best of our knowledge, no studies have evaluated the natural history of patients with HCM using thallium-201 SPECT.
Thus, this study aimed to evaluate the changes in LV remodelling with time and to confirm the lesion site in patients with HCM using thallium-201 SPECT.
Methods
Study patients
Forty-eight patients with HCM participated after providing informed consent. This study was approved by the Human Investigations Committee of Ehime University Hospital (No. 14-25 in 2002). All patients met the cardiomyopathy criteria of the World Health Organization/International Society and Federation of Cardiology.6 In short, all patients are characterized by LV hypertrophy, which is usually asymmetric and involves the interventricular septum. Typically, the LV volume is normal or reduced. Of the 48 patients with HCM, 36 had hypertrophic non-obstructive cardiomyopathy and 12 had hypertrophic obstructive cardiomyopathy. Patients with history of coronary artery stenosis, atrial fibrillation or LVHF, and a plasma creatinine level ≧1.2 mg/dL at the start of the study were excluded. All patients were followed up for at least 6 years using thallium-201 SPECT. A total of 96% and 90% of patients used beta-blockers and calcium antagonists, respectively.
Thallium-201 myocardial scintigraphy
Thallium-201 SPECT was performed using a previously described method.7 Briefly, after overnight fasting, patients were injected with 111 MBq of thallium-201, and imaging was performed 5 h after the injection. Tomographic images were acquired using a triple-headed gamma camera (GCA 9300; Toshiba, Tokyo, Japan) equipped with a low-energy, high-resolution, parallel-hole collimator. Thirty-six projections were obtained over 90 s each over a 360° orbit, and data were stored in a 128 × 128 matrix. Fifteen per cent of the energy window was centred on the 72 keV photopeak. A series of 3.5-mm-thick trans-axial slices were reconstructed with filtered backprojection by a Ramp–Hanning filter. Short-axis slices were reconstructed from the trans-axial slices. Attenuation correction was performed using Chang's method,8 and scatter correction was performed.
Thallium-201 myocardial scintigraphy was usually performed every 1 year in almost all patients.
Estimation of myocardial perfusion defects
In this study, two indices were used to evaluate myocardial perfusion defects. One was the extent score (ES). To quantify the size of myocardial perfusion defects, the computerized thallium-201 tomographic method produced by Garcia et al. was used.9 To formulate polar maps, the normalized maximal count value at each point was compared with the normal value at the corresponding point. The extent polar map depicted the extent points with subnormal counts of 2 standard deviations (SDs) under the mean. The ES was defined as the number of points that fell 2 SDs under the mean and was expressed as a percentage of the total LV points on the extent polar map.
The ‘mean count change’ (MCC) was devised to estimate the amount of myocardium in jeopardy as another index. MCC was calculated as the following formula: MCC (%) = (mean thallium-201 uptake at the first study) − (mean thallium-201 uptake at the next study)∕(mean thallium-201 uptake at the first study) × 100.
Figure 1 shows the changes in ES and MCC in a patient with HCM. Column ① represents the data at the first examination, and columns ②, ③, and ④ represent the data at 2, 6, and 8 years after the first examination, respectively. Over time, the uptake of thallium-201 significantly decreased as shown in the original map; the real decrease in its uptake was expressed by the change in the mean count. In fact, the ES and the MCC gradually increased over time.
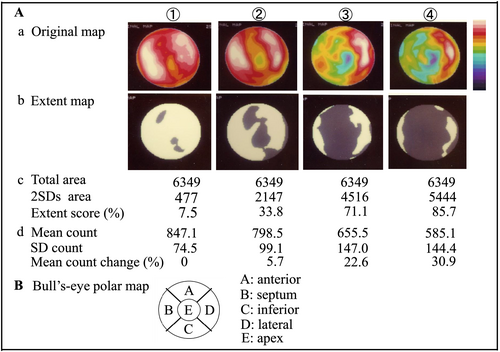
Site of the lesion
For a semi-quantitative analysis of the regional thallium-201 uptake, the LV myocardium was divided into five segments on a bull's-eye polar map as shown in Figure 1: anterior, septal, inferior, lateral, and apex. Of these five segments, a segment filled with an area of uptake >2 SDs was regarded as the site of lesion.
Left ventricular remodelling estimated by echocardiography and electrocardiography
Echocardiographic and electrocardiographic changes were also estimated with a SEQUIA-512 (ACUSON Inc, CA, USA) or ProSound II SSD-6500SV (Hitachi-Aloka Inc, Japan) ultrasound system. LV end-diastolic and end-systolic dimensions, interventricular septal wall thickness, LV posterior wall thickness, and left atrial dimension were measured. In addition, LV fractional shortening was calculated. To estimate the severity of LV hypertrophy with an electrocardiogram, the ‘total 12-lead QRS voltage’ was measured.10
Prognosis and cardiovascular complications
All deaths were recorded during the follow-up period. Cardiovascular complications, such as LVHF, atrial fibrillation, apoplexy, valve replacement, pacemaker implantation, implantable cardioverter defibrillator implantation, myocardial infarction, and cancers, were confirmed. LVHF was defined as Class III or IV by the New York Heart Association functional classification.
Statistical analysis
All values are expressed as mean ± SD. Data obtained before and after the determination of the sample were compared using Student's t-test for paired samples. Groups were compared in both univariate and multivariate analyses using the Cox regression model. A value of P < 0.05 was statistically significant.
Results
Mean follow-up period
The mean follow-up period was 8.6 ± 2.0 years (range 6.3 to 12.8 years).
Thallium-201 single-photon emission computed tomography data
The mean count significantly decreased from the first to the last study, and the SD of the last study significantly increased compared with that of the first study (Table 1). Thus, the MCC of the last study significantly increased compared with that of the first study. In addition, areas with uptake >2 SDs significantly increased from the first to the last study; thus, the ES significantly increased from the first to the last study.
| First study | Last study | P-value | |
|---|---|---|---|
| n | 48 | 29 | |
| Mean age (years) | 54.6 ± 11.5 | 65.2 ± 9.2 | |
| Mean count | 830.9 ± 41.6 | 731.6 ± 73.2 | <0.0001 |
| SD count | 75.5 ± 20.0 | 112.8 ± 35.7 | <0.0001 |
| Mean count change (%) | 0 | 12.0 ± 9.0 | <0.0001 |
| Total area | 6349 | 6349 | |
| 2 SDs area | 1074.8 ± 890.9 | 2795.8 ± 1418.7 | <0.0001 |
| Extent score (%) | 17.4 ± 13.7 | 44.0 ± 22.3 | <0.0001 |
| IVST (mm) | 20.1 ± 4.5 | 14.0 ± 3.9 | <0.0001 |
| LVPWT (mm) | 13.2 ± 2.4 | 11.4 ± 2.5 | <0.0001 |
| LVDD (mm) | 43.2 ± 5.0 | 51.7 ± 6.2 | <0.0001 |
| LVED (mm) | 24.9 ± 5.3 | 35.5 ± 8.1 | <0.0001 |
| LVFS (%) | 42.8 ± 8.1 | 31.9 ± 9.6 | <0.0001 |
| Left atrial dimension (mm) | 37.5 ± 5.2 | 45.9 ± 6.6 | <0.0001 |
| Total QRS voltage (mm) | 297.5 ± 91.0 | 206.9 ± 58.0 | <0.0001 |
- IVST, interventricular septal wall thickness; LVDD, left ventricular diastolic dimension; LVED, left ventricular end-diastolic dimension; LVFS, left ventricular fractional shortening; LVPWT, left ventricular posterior wall thickness; SD, standard deviation.
Echocardiographic and electrocardiographic data
Interventricular septal wall thickness and LV posterior wall thickness in the last study were significantly decreased compared with those in the first study (Table 1). LV end-diastolic and end-systolic dimensions significantly increased from the first to the last study. LV fractional shortening in the last study significantly decreased compared with that in the first study. Left atrial dimension significantly increased from the first to the last study. On the contrary, the total 12-lead QRS voltage significantly decreased from the first to the last study.
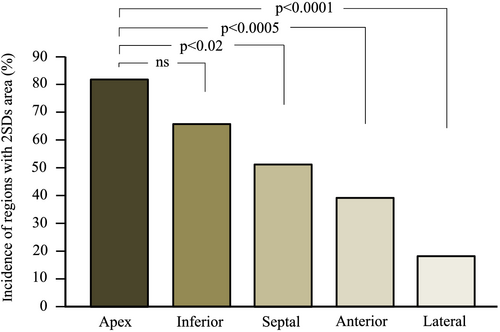
Incidence of location of the 2 standard deviations area
Thirty-three patients had areas with a thallium uptake >2 SDs in more than one segment (Figure 2). Figure 2 shows the incidence of a lesion site. Lesions were more frequent at the apex region with significant differences over the septal, anterior, and lateral regions.
Influence of left ventricular heart failure on the patterns of thallium-201 single-photon emission computed tomography, echocardiography, and electrocardiography
Patients were subdivided into two groups according to LVHF: Group A: patients who experienced LVHF during the follow-up period (n = 27), and Group B: patients who did not experience LVHF during the follow-up period (n = 21) (Table 2 and Figure 3). The mean follow-up periods were 8.8 ± 1.8 years in Group A and 8.3 ± 2.2 years in Group B, respectively.
| Group A | First study | Last study | P-value |
|---|---|---|---|
| n | 27 | 13 | |
| Mean age (years) | 54.3 ± 12.6 | 64.8 ± 9.3 | |
| Mean count | 832.2 ± 47.5 | 689.4 ± 45.2 | <0.0001 |
| SD count | 78.0 ± 23.5 | 131.0 ± 29.8 | <0.0001 |
| Mean count change (%) | 0 | 17.4 ± 4.8 | <0.0001 |
| 2 SDs area | 1112.6 ± 910.2 | 3411.8 ± 1127.5 | <0.0001 |
| Extent score | 17.5 ± 14.3 | 53.7 ± 17.8 | <0.0001 |
| IVST (mm) | 19.8 ± 4.8 | 12.1 ± 2.5 | <0.0001 |
| LVPWT (mm) | 12.6 ± 2.0 | 11.0 ± 3.8 | <0.0001 |
| LVDD (mm) | 43.9 ± 4.8 | 54.1 ± 4.7 | <0.0001 |
| LVSD (mm) | 25.8 ± 5.4 | 39.6 ± 6.5 | <0.0001 |
| LVFS (%) | 41.5 ± 7.9 | 27.0 ± 7.4 | <0.0001 |
| Left atrial dimension (mm) | 37.2 ± 5.4 | 48.0 ± 6.5 | <0.0001 |
| Total QRS voltage (mm) | 308.4 ± 94.7 | 186.1 ± 39.2 | <0.0001 |
| Group B | First study | Last study | P-value |
|---|---|---|---|
| n | 21 | 16 | |
| Mean age (years) | 55.0 ± 10.4 | 65.0 ± 9.4 | |
| Mean count | 829.1 ± 33.3 | 785.9 ± 66.5 | <0.02 |
| SD count | 72.5 ± 14.4 | 89.5 ± 28.5 | <0.05 |
| Mean count change (%) | 0 | 4.9 ± 8.5 | <0.0001 |
| 2 SDs area | 1026.2 ± 885.2 | 2003.9 ± 1380.7 | <0.01 |
| Extent score | 17.2 ± 13.1 | 31.6 ± 21.7 | <0.02 |
| IVST (mm) | 20.5 ± 4.1 | 16.3 ± 4.2 | <0.001 |
| LVPWT (mm) | 14.0 ± 2.7 | 12.8 ± 2.9 | <0.01 |
| LVDD (mm) | 42.4 ± 5.3 | 48.6 ± 6.5 | <0.0001 |
| LVSD (mm) | 23.7 ± 5.1 | 30.2 ± 6.9 | <0.0001 |
| LVFS (%) | 44.3 ± 8.3 | 38.2 ± 8.4 | <0.0001 |
| Left atrial dimension (mm) | 37.7 ± 5.0 | 43.1 ± 5.8 | <0.0005 |
| Total QRS voltage (mm) | 284.0 ± 86.6 | 233.1 ± 67.6 | <0.02 |
- IVST, interventricular septal wall thickness; LVDD, left ventricular diastolic dimension; LVFS, left ventricular fractional shortening; LVPWT, left ventricular posterior wall thickness; LVSD, left ventricular end-systolic dimension; SD, standard deviation.
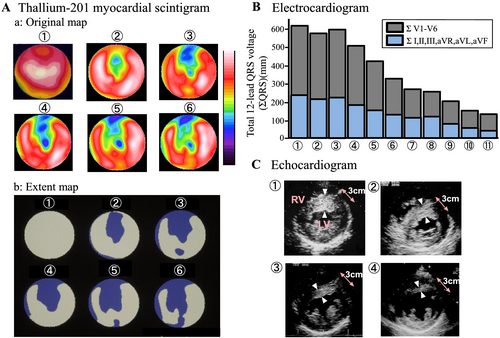
Figure 3 shows the changes in the original and extent maps in (A) thallium-201 SPECT, (B) total 12-lead QRS voltage, and (C) short-axial echocardiogram in a patient who had LVHF during the 11.6 year follow-up period. In each figure, ① corresponds to the first examination and ⑥, ⑪, and ④ correspond to the last examination in Figure 3–3, respectively. With time, thallium-201 uptake decreased on the original map and perfusion defects on the extent map increased, while total 12-lead QRS voltage and wall thickness decreased. As shown in Table 2, all data in both groups significantly deteriorated. Additionally, almost all P-values indicated the presence of a more severe condition in Group A than in Group B.
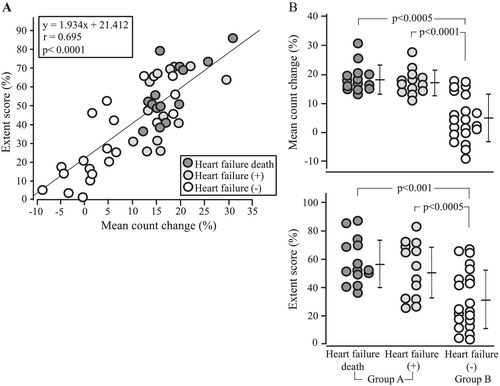
Correlation between extent score and mean count change and comparisons of mean count change (upper panel) and extent score (lower panel) between Groups A and B
As shown in Figure 4, there was a significant correlation between ES and MCC (r = 0.695, P < 0.0001). Figure 4 compares the MCC (upper panel) and the ES (lower panel) between Groups A and B. Both ES and MCC were significantly greater in Group A than in Group B. An overlap between both groups was greater in ES than in MCC.
Prognosis and cardiovascular complications
During the follow-up period, 19 patients (39.6%) had died (Figure 5). Fourteen patients died from LVHF and three from SCD. In addition, two died from cancer. The mean count of three patients with SCD indicated no decrease even in the last examination.

Figure 5 compares the cardiovascular complications in Groups A and B during the follow-up periods. The incidence of atrial fibrillation and apoplexy was significantly higher in Group A than in Group B, while other complications showed no significant difference.
Discussion
We for the first time evaluated the clinical course in patients with HCM using thallium-201 SPECT. This modality can confirm the severity of myocardial damage not only qualitatively but also quantitatively and can confirm the site of myocardial damage. The index MCC, which was newly devised, may be superior to ES in the differentiation of LV changes over time. The incidence of death due to LVHF was much higher than that due to SCD.
Clinical significance of thallium-201 single-photon emission computed tomography findings
The observation of natural history in patients with HCM by thallium-201 SPECT seems to be superior to that by electrocardiography or echocardiography. One advantage is the early detection of myocardial changes, and the other is to be able to confirm the lesion site. In addition, myocardial changes evaluated by thallium-201 SPECT can be confirmed visually by the change in colour in the bull's-eye polar map. Furthermore, this change can be evaluated not only qualitatively but also quantitatively, as shown in Figures 1 and 3. Thus, we can clearly predict the future clinical manifestations and natural history of HCM by thallium-201 SPECT.
Comparison between extent score and mean count change
In this study, we introduced a new index, termed MCC, to evaluate myocardial perfusion defects over time. We confirmed in this study that there was a significant correlation between MCC and ES. Thus, MCC can be utilized to evaluate myocardial perfusion defects in patients with HCM.
Extent score can evaluate the myocardial perfusion defects quantitatively, but its value is decided relatively. Thus, when the uptake of thallium-201 is decreased, the accuracy of ES may be limited. MCC is calculated from the real difference in thallium-201 uptake. In this study, as shown in Figure 4, the overlap between Groups A and B was greater for ES than for MCC. This may indicate that in the differentiation of LV changes, MCC may be superior to ES.
Site of the lesion
In this study, myocardial perfusion defects evaluated by ES were identified most commonly in the apex region, as shown in Figure 2. The site of the involved lesion depends on tissue and haemodynamic characteristics. Tissue characteristics include the severity of LV hypertrophy and the severity of disarrayed cardiac muscle cells, while haemodynamic characteristics are mainly related to the severity of wall motion. Septal and anterior regions usually have worse tissue characteristics but less wall motion. The apex region usually has worse tissue characteristics reflected by negative T-waves on electrocardiogram and a stronger wall motion, resulting in the highest incidence of lesions. In a histological study of 30 explanted hearts with end-stage HCM, the replacement into the myocardial fibrosis was preferentially observed at the LV apex.11 In addition, recent reports about LV thrombus in apical aneurysm in patients with HCM12, 13 may support our finding.
Prognosis and cardiovascular complications
The highest incidence of death was due to LVHF (73.7%), followed by SCD (15.8%). Many previous studies have indicated that the incidence of SCD was higher than that of LVHF-related death. Thaman et al. reported that LV remodelling process in patients with HCM is a time-related phenomenon and thus depends on the following duration.14 The mean follow-up period from the first visit to the hospital to the occurrence of LVHF was approximately 10 to 15 years.15, 16 In fact, in studies with a follow-up period of ≧10 years, the incidence of death due to LVHF was higher than that of SCD.15, 17
Recently, a paper about LVHF in cardiomyopathies was published in the European Society of Cardiology.18 In the European Society of Cardiology guidelines, LVHF patients, especially those with non-obstructive HCM, should receive medical therapy first according to the guideline, and in patients who progress to advanced LVHF, heart transplantation should be considered.19, 20 It has already been reported that there is no intervention capable of impeding or preventing progression from typical HCM to LVHF.21 Thus, it is important to find a therapy that prevents the progression from typical HCM to LVHF. Recently, we reported for the first time that drug therapy with cibenzoline could decrease the LV pressure gradient, induce a regression of LV hypertrophy, and improve LV diastolic dysfunction in patients with hypertrophic obstructive cardiomyopathy.22 It is expected that this therapy can lower the occurrence of LVHF in patients with HCM.
The ESs in patients with SCD in this study were 1.7%, 4.6%, and 11.2%, and the MCCs were −0.6%, −9.0%, and 1.2%, respectively. These data indicate that SCD in this study is not related to LV systolic dysfunction. It is hypothesized that a genetically transmitted myocardial defect may be closely related to SCD. Thus, it seems to be very difficult to reduce the occurrence of SCD in patients with HCM.
In this study, 27 patients (56.3%) experienced LVHF during the follow-up period, and 17 patients (35.4%) had atrial fibrillation. In a contemporary registry of 1417 patients with HCM in Europe, the prevalence of symptomatic LVHF was 49.9% in NYHA Class II and 17.4% in Classes III and IV.23 The occurrence of atrial fibrillation significantly increases the risk of a detrimental clinical course.24, 25 Medical therapy with cibenzoline is known to markedly improve LV diastolic dysfunction.22, 26, 27 This drug may reduce the occurrence of atrial fibrillation in patients with HCM.
Relationship between thallium-201 single-photon emission computed tomography, electrocardiography, and echocardiography
Changes in thallium-201 SPECT, electrocardiography, and echocardiography showed the same changing patterns, as shown in Figure 3. This indicates that each modality can follow the LV myocardial changes on its own. However, we believe that thallium-201 SPECT is superior to electrocardiography and echocardiography in the early detection and in the confirmation of the lesion site and provides visual feedback through changes in colour regarding LV myocardial changes.
Limitations
The number of patients who participated in this study was reduced. Evaluation by thallium-201 SPECT is time consuming, as opposed to electrocardiographic or echocardiographic estimation. In addition, thallium-201 SPECT is expensive. In this study, to estimate the amount of myocardium at risk, MCC was introduced as another index. According to our experience, MCC is extremely useful in the evaluation of the LV changing pattern.
Scope for future studies
Different from the evaluations by electrocardiography and echocardiography, the early detection of myocardial changes as well as knowing the site of the lesion by thallium-201 SPECT can help with understanding the future clinical manifestation as well as complications of HCM.
Conflict of interest
None declared.




