Sudden cardiogenic shock mimicking fulminant myocarditis in a surviving teenager affected by severe acute respiratory syndrome coronavirus 2 infection
Abstract
In the context of the coronavirus disease 2019 pandemic, myocardial injury is a relatively frequent finding. Progression to cardiogenic shock has been rarely described, especially in healthy young patients. The underlying mechanisms are to date controversial. A previously healthy 18-year-old female teenager affected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) developed fulminant cardiogenic shock requiring a prompt extracorporeal membrane oxygenation support. Cardiac involvement was predominant compared with the pulmonary one. Myocardial biopsies were performed; and in order to clarify the pathophysiology of the acute heart failure, optical and transmission electron microscopy study was realized. Two additional immunohistology techniques were developed in order to (i) detect a SARS-CoV-2 recombinant fusion nucleoprotein by using a specific antibody and (ii) study fractalkine expression induced by activated endothelium because this molecule is well known to be elevated in patients with severe cytokine release syndrome. SARS-CoV-2 genome was not detected in the myocardium. Even if the clinical presentation, laboratory markers, and cardiac imaging techniques strongly suggested fulminant myocarditis, histology and immunohistology were not fully consistent with this diagnosis according to the Dallas criteria. Although rare suspected coronavirus particles were found by transmission electron microscopy in the cardiac endothelium, neither significant immunoreactivity for the viral nucleocapsid protein nor image suggestive of endotheliitis was detected. Intense endothelial immunoreactivity pattern for fractalkine expression was observed. From a clinical point of view, the left ventricular systolic function gradually improved, and the patient survived after a long stay in the intensive care unit. Our observations suggest that a massive cytokine storm induced by SARS-CoV-2 infection was the main cause of the cardiogenic shock, making a direct viral injury pathway very unlikely.
Introduction
The frequency of myocardial injury (defined by increased cardiac troponin levels) is variable among hospitalized coronavirus disease 2019 (COVID-19) patients, with a reported prevalence of 7–28%.1-4 However, progression to cardiogenic shock (CS) is uncommonly reported in adults and exceptionally described in healthy children or adolescent patients.5 Prognosis in this setting is often ominous, and therapeutic options are limited. We described a case of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-related CS in a surviving female teenager who required an extracorporeal membrane oxygenation (ECMO) support in the acute phase.
Case report
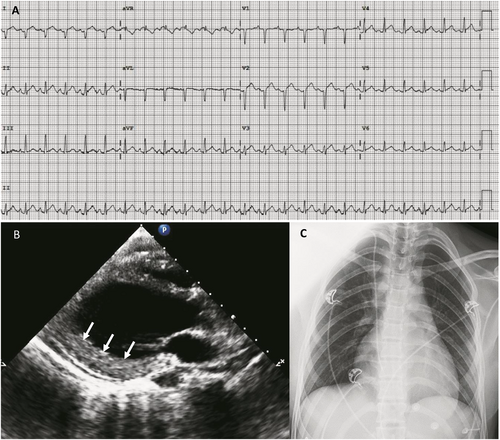
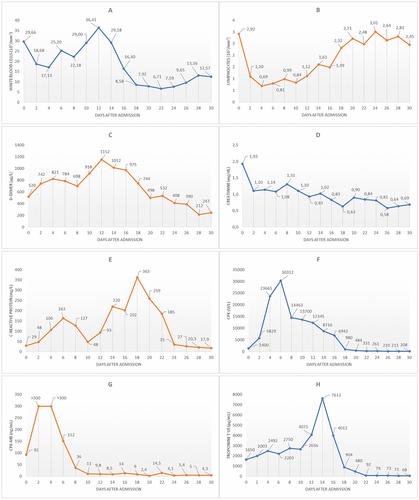
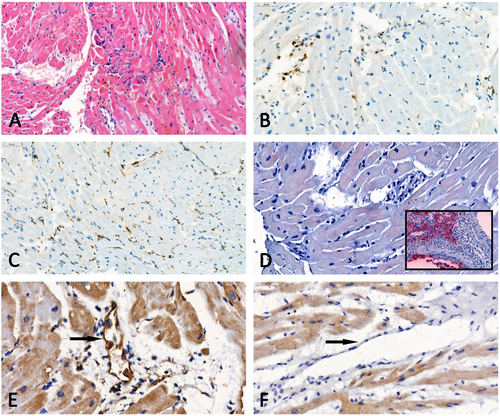
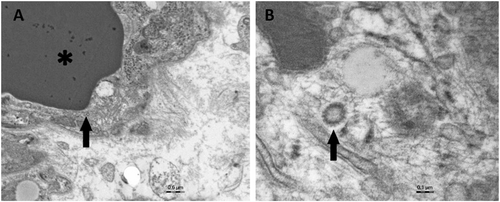
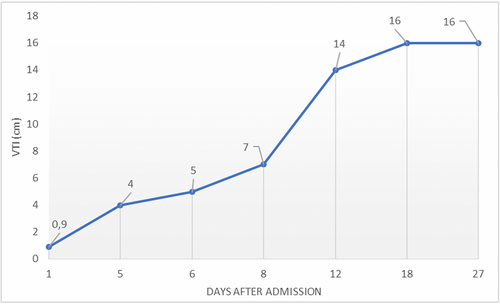
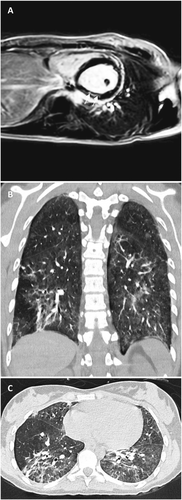
A previously healthy 18-year-old woman was admitted to the emergency department of our hospital complaining of nausea and vomiting. These symptoms occurred the day before she was admitted. No fever was reported. Upon admission, clinical features of impending shock were observed: body temperature was 32°C and blood pressure 85/50 mmHg, with cold extremities and confusion. Electrocardiogram revealed sinus tachycardia at 140 b.p.m., with subtle diffuse ST segment elevation and PR segment depression (Figure 1). Arterial blood gas analysis showed severe metabolic acidosis with serum lactates at 11 mmol/L (n.v. <1 mmol/L). Laboratory tests revealed marked leucocytosis and neutrophilia, with a C-reactive protein raised at 29 mg/L (n.v. <5 mg/L). Cardiac markers were elevated: creatine kinase (CK) 1400 U/L, CK-MB 92 U/L, and high-sensitivity troponin T 1650 pg/mL (n.v. <14 pg/mL). Serum creatinine elevation at 1.9 mg/dL and mild hyperkalaemia were compatible with concomitant acute kidney injury (Figure 2). Urgent transthoracic echocardiogram (TTE) showed left ventricular (LV) wall thickening without dilation and a speckled myocardial appearance suggesting myocardial oedema as well as mild inferior pericardial effusion and severe bi-ventricular dysfunction with LV ejection fraction (LVEF) of 10% (Figure 1 and Videos S1 and S2). Chest X-ray was unremarkable (Figure 1). Fulminant myocarditis was suspected, and the patient was transferred to the intensive care unit (ICU). Increased infusion rates of dobutamine and additional vasopressors were needed. Unfortunately, despite pharmacological treatment, the patient remained in shock and developed acute respiratory failure. Mechanical ventilation was started; and considering refractory CS, a percutaneous venoarterial ECMO (VA-ECMO) was inserted 8 h after admission. TTE showed an aortic valve hardly opening in systole. Therefore, an intra-aortic balloon pump (IABP) was inserted. A coronary angiogram showed normal coronary arteries, and ventriculography confirmed a very poor LV contractility (Video S3). Endovascular myocardial biopsies showed a low density of inflammatory cells without myocyte degeneration or necrosis (Figure 3). The patient was extensively evaluated for any underlying infectious or autoimmune aetiologies (Table 1). Multiple blood cultures were negative. SARS-CoV-2 nucleic acid was present in the nasopharyngeal swab. Transmission electron microscopy (TEM) was performed on the myocardial tissue, demonstrating suspected coronavirus particles in endothelial cell cytoplasm (Figure 4A, B). Upon admission, the patient was treated empirically with hydroxychloroquine, (400 mg b.i.d. at Day 1 and then 200 mg b.i.d. from Day 2 to 5), high doses of methylprednisolone (200 mg/day from Day 1 to 8), and intravenous immunoglobulin (cumulative dose 2 mg/kg, from Day 1 to 3) and antibiotics. Her ICU stay was complicated by the following: (i) pulmonary oedema and acute respiratory distress syndrome requiring a switch in the ECMO configuration from VA-ECMO to venoartero-venous ECMO (VAV-ECMO) on Day 5; (ii) bilateral significant pleural effusion requiring drainage (Days 7 and 9); (iii) severe coagulopathy (fibrinogen 160 mg/dL and platelets 27 × 103/mm3); and (iv) severe rhabdomyolysis (CK level up to >30 000 U/L) possibly related to ECMO-induced haemolysis. After 12 days of mechanical circulatory support, bedside TTE demonstrated a gradual improvement in cardiac contractility, with an LV outflow tract velocity time integral of 14 cm (Figure 5). The arterial VAV-ECMO cannula was removed the same day, and the patient was weaned from VV-ECMO and IABP on Day 17. The ICU stay lasted 34 days. Before discharge, 45 days after admission, a cardiac magnetic resonance revealed a non-dilated LV with moderate global hypokinesia and LVEF close to 40% (Videos S4, S5). A non-ischaemic pattern of late gadolinium enhancement was obvious in basal to mid-inferior and inferoseptal segments (Figure 6). Although the patient had stable resting oxygen saturation in the range of 95–97% while breathing room air, chest computed tomography still showed diffuse, bilateral infiltrates, suggestive of moderate persistent lung involvement (Figure 6B and C). An evidence-based, guideline-recommended heart failure medical therapy was started. The TTE performed 2 months after discharge confirmed progressive improvement in LV systolic function with triplane LVEF of 48% (Video S6).
| Value | Normal value | |
|---|---|---|
| Adenovirus serology | Negative | Negative |
| Influenza virus serology | Negative | Negative |
| HBV and HCV serology | Negative | Negative |
| CMV serology | Negative | Negative |
| B19V serology | Negative | Negative |
| Echo/Coxsackie virus serology | Negative | Negative |
| EBV serology | Negative | Negative |
| Rubella virus serology | Negative | Negative |
| Measles virus serology | Negative | Negative |
| Rickettsia serology | Negative | Negative |
| Mycoplasma pneumoniae serology | Negative | Negative |
| Chlamydia serology | Negative | Negative |
| Borrelia serology | Negative | Negative |
| EMB PCR Panela | Negative | Negative |
| Nasopharyngeal swab PCR SARS-CoV-2 | Positive | Negative |
| ANA (titre) | 1:80 | <1:80 |
| Anti-ds-DNA | 9.8 UI/mL | < 27 UI/mL |
| ANCA (p-ANCA and c-ANCA) | <0.20/ <0.20 UI/mL | <3.50/ <2.00 UI/mL |
| Rheumatoid factor | 10.7 U/mL | <14 U/mL |
- Abbreviations: ANA, anti-nuclear antibody; ANCA, anti-neutrophil cytoplasmic antibodies; Anti-ds-DNA, anti-double stranded DNA antibody; B19V, parvovirus B19; CMV, cytomegalovirus; EBM, endomyocardial biopsy; EBV, Epstein–Barr virus; HBV, hepatitis B virus; HCV, hepatitis C virus; PCR, polymerase chain reaction.
- a EMB PCR Panel: enterovirus, adenovirus, CMV, B19V, and SARS-CoV-2 genome were searched.
Discussion
The pathophysiology of cardiac involvement in COVID-19 remains unclear but likely involves increased cardiac stress due to respiratory failure/hypoxaemia6 and indirect injury related to cytokine storm and systemic inflammatory response.7, 8 SARS-CoV-2 binds to the transmembrane angiotensin-converting enzyme 2 protein. Because this receptor is largely expressed in the cardiovascular system (mainly in the pericytes and endothelial cells), direct cardiomyocyte infection is a third postulated mechanism.9-11 However, direct evidence confirming the last mechanism is still lacking. We presented a case of CS successfully supported by ECMO in a teenage patient affected by SARS-CoV-2 infection. Rare suspected coronavirus particles were found in the cardiac endothelium. Despite that their morphology consistent with that of Coronaviridae, we were unable to certify that those particles corresponded to actual Coronaviridae in the absence of associated cytoplasmic vacuoles and immunogold techniques applied on TEM sections. In addition, we developed an immunohistology technique using an antibody against a SARS-CoV-2 recombinant fusion nucleoprotein and a lung tissue specimen of an infected hamster as positive control. No significant immunoreactivity (in either myocytes or endothelial cells) was detected (Figure 3). Interestingly, also in other myocarditis reports, SARS-CoV-2 genome was not detected in the myocardium.12-14 Even if the clinical presentation, laboratory markers, and cardiac imaging techniques strongly suggested fulminant myocarditis, histology and immunohistology were not fully consistent with this diagnosis according to the Dallas and World Health Organization/International Society and Federation of Cardiology criteria.15-17 Although recent findings suggest that SARS-CoV-2 infection might induce endotheliitis as a direct consequence of viral involvement, endotheliitis signs were not found in our patient.18 We therefore assumed that a massive cytokine storm and inadequate host inflammatory response leading to diffuse myocardial oedema were probably the main causes of CS. To support this hypothesis, we analysed fractalkine expression by immunohistology on myocardial biopsy. The chemokine receptor CX3CR1 is able to bind to fractalkine, which is expressed by activated endothelium in response to TNFα and IFN-γ.19 This molecule is well known to be elevated in patients with severe cytokine release syndrome,20 and CX3CR1-mediated inflammation has been demonstrated in several inflammatory disorders.21 Immunohistology sections showed an endothelial immunoreactivity in our patient and no staining in the myocardium of a patient who died from a COVID-19-unrelated cause (Figure 3). CS is a rare and life-threatening presentation of SARS-CoV-2 infection that might require a mechanical circulatory support and a very long ICU stay. Our case adds another element to the pathophysiology understanding of the SARS-CoV-2-related myocardial injury.
Acknowledgements
The authors are grateful to Dr D. Desmecht and M. Sarlet (Animal Medicine Faculty, Liège University) for providing the infected-hamster lung control tissue specimens.
Conflict of interest
Giovanni Garau, Sabrina Joachim, Guy-Loup Duliere, Maria Melissopoulou, Sandrine Boccar, Vincent Fraipont, Christophe Dugauquier, Pierre Troisfontaines, Olivier Hougrand, Philippe Delvenne, and Etienne Hoffer declare that they have no conflict of interest.