Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio as predictors of survival after heart transplantation
Abstract
Aims
The aim of this study was to evaluate whether neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) predict outcome in heart failure (HF) patients undergoing heart transplantation (HTX).
Methods and results
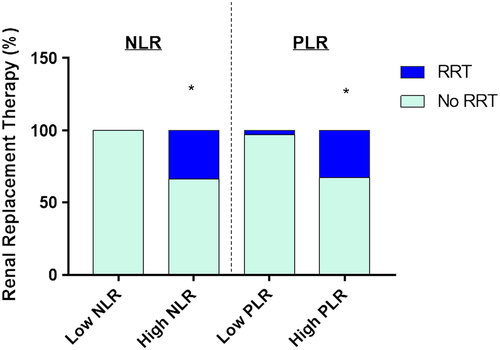
Data from 111 HF patients undergoing HTX 2010–2015 were retrospectively reviewed. NLR and PLR were calculated before HTX, immediately after HTX, and at 6 and 24 hours. Primary endpoint was in-hospital mortality, and secondary endpoints were 1 year mortality and renal replacement therapy (RRT). Prognostic factors were assessed by multivariate analysis, and the predictive values of NLR and PLR for mortality were compared. The discriminatory performance for predicting in-hospital mortality was better for NLR [area under the receiver operating characteristic curve (AUC) = 0.644, 95% confidence interval 0.492–0.797] than for PLR (AUC = 0.599, 95% confidence interval 0.423–0.776). Best cut-off value was 2.41 for NLR (sensitivity 86%, specificity 67%) and 92.5 for PLR (sensitivity 86%, specificity 68%). When divided according to best cut-off value, in-hospital mortality was significantly higher in the high NLR group (17.5% vs. 3.2%, P < 0.05), but not in the high PLR group (16.5% vs. 6.3%, P = ns). One year mortality was not significantly higher for either group (37.5% vs. 6.5% for NLR; 36.7% vs. 9.4% for PLR, P = ns for both), while RRT was significantly higher in both the NLR and PLR high groups (33.8% vs. 0%; 32.9% vs. 3.1%, respectively, P < 0.001). Multivariate analysis indicated that only high NLR (hazard ratio = 3.403, P < 0.05) and pre-transplant diabetes (hazard ratio = 3.364, P < 0.05) were independent prognostic factors for 1 year mortality.
Conclusions
High NLR was a predictor for in-hospital mortality, and an independent prognostic factor for 1 year mortality. Both high NLR and high PLR were predictors for RRT.
Introduction
Heart transplantation (HTX) has evolved as the treatment of choice for patients with heart failure (HF) who have severe symptoms despite maximum medical therapy. Survival among cardiac transplant recipients has improved as a result of improvements in treatments that suppress the immune system and prevent rejection. Despite successful transplantation, mortality remains high.1 Several factors related to both the donor and the recipient are associated with poor outcomes after transplantation.2 Inflammation plays a critical role before and after HTX. Before surgery, several inflammatory markers haven shown prognostic value in HF including tumour necrosis factor and its receptors, the interleukin (IL)-1 and IL-6 families, galectin-3, and C-reactive protein.3, 4 Besides, increased inflammation before cardiac surgery with cardiopulmonary bypass is associated with worse outcome.5, 6 After surgery, graft inflammation may respond to several mechanisms, from alloantigen-directed immune reactions of the recipient resulting in graft rejection to ischaemia/reperfusion injury of the graft.7 Inflammation of the donor before explantation is also associated with worse outcome of the recipient.8, 9
Neutrophil-to-lymphocyte ratio (NLR) is a marker of inflammation. First described in 1967 as an indicator of ozone exposure,10 NLR has shown prognostic value in different cardiovascular conditions including stable coronary artery disease, acute coronary syndromes, HF, and coronary artery bypass grafting (CABG).11 On the other hand, platelet-to-lymphocyte ratio (PLR) was first described in 2008 as a prognostic marker in periampullary cancer12 and has also shown prognostic value in patients with ST elevation acute myocardial infarction13-15 and stable coronary artery disease16, 17 and in patients with an implantable cardioverter defibrillator.18 Despite raising evidence supporting the use of NLR and PLR in cardiovascular disease, no study has evaluated the role of these markers in patients undergoing HTX.
Therefore, the objective of this study was to determine the role of NLR and PLR as markers of prognosis in patients undergoing HTX.
Methods
Study design and immunosuppressive therapy
A single-centre, retrospective cohort study was performed evaluating all consecutive cardiac transplantation recipients between January 2010 and December 2015, at Hospital Italiano de Buenos Aires, Argentina. Inclusion criteria was first orthotopic HTX, while exclusion criteria were patients younger than 18 years, second transplantation, and multi-organ transplants. The study was approved by the institutional review board (#3200) and conforms with the principles outlined in the Declaration of Helsinki.
All patients received methylprednisolone intraoperatively (15 mg/kg when the aortic cross clamp was released) followed by 100 mg b.i.d. intravenous for the first 48 h, and basiliximab (20 mg loading dose in the operating room and 20 mg the fourth day).
Inflammatory markers
All patients were in-hospital at the time of transplantation. Venous blood was drawn at the forearm and stored in plastic tubes containing EDTA. Absolute and relative white blood cell counts were generated automatically by volumetric impedance (UniCel® DxH 800 Coulter cellular Analysis System, Beckman, Brea, CA). The NLR or PLR was calculated as follows: NLR = (neutrophil absolute count)/(lymphocyte count), and PLR = (platelet count)/(lymphocyte count). Patients were stratified into high or low NLR and PLR groups based on the cut-off value obtained at receiver operating characteristic (ROC) curve analysis for predicting the primary composite endpoint according to Youden index. Baseline laboratory was performed few hours before transplantation, immediately after surgery, and 6 and 24 h after surgery.
Study endpoints
The primary endpoint was in-hospital mortality. Secondary outcomes included in-hospital renal replacement therapy (RRT) and 1 year mortality. Indications for RRT were performed by the attending nephrologist owing to oliguria or anuria despite maximum doses of intravenous diuretics, increase in renal retention parameters, and/or hydroelectrolytic imbalance. Patients that required RRT were treated with continuous veno-venous haemofiltration, continuous arteriovenous haemodialysis, or intermittent haemodialysis. One year mortality was assessed through electronic records. If no follow-up data were available, patients were contacted by phone to assess follow-up status.
Statistical analysis
Continuous variables were expressed as mean and standard deviation and compared using Student's t-test. Categorical data were presented as frequency and were analysed using the Pearson χ2 test or Fisher's exact test. Survival curves were estimated using Kaplan–Meier analyses, and the differences in survival rates between groups were compared using the log-rank test. Univariate analysis was performed to assess significant differences in characteristics that influence overall survival after HTX. Multivariate analysis was performed using Cox regression analysis for significant variables identified by univariate analysis. To estimate the predictive value of NLR and PLR for the primary endpoint, ROC curves were constructed, and the area under the ROC curve (AUC) was calculated to compare the discriminatory performance of NLR or PLR for the prediction of the primary endpoint, with 95% confidence interval (CI95). All statistical tests were performed using statistical software SPSS 23.0 for Microsoft (SPSS Inc; an IBM Company, Chicago, IL) and Graph Pad Prism version 7.0 for Microsoft (GraphPad Software, La Jolla, CA). A P < 0.05 was considered statistically significant.
Results
A total of 118 patients underwent orthotopic HTXs over the study period. Two patients were excluded for second transplantation, and five were excluded for multi-organ transplantation. Final analysis included 111 patients for whom complete data were available. The study group was composed of 71 men (78.8%) and 40 women (21.2%). Median age was 52 years (range, 43–59 years). Baseline (prior to HTX) white blood cell absolute and relative count, platelet count, NLR, and PLR are shown in Table 1. Mean baseline NLR was 4.37 and mean PLR was 146.1.
| Blood components | Mean ± SD | Median | Minimum | Maximum | Normal values |
|---|---|---|---|---|---|
| Total white blood cells (×109/L) | 8.37 ± 2.89 | 7.95 | 3.13 | 22.04 | 4.00–10.00 |
| Absolute neutrophil count (×109/L) | 5.60 ± 2.64 | 5.25 | 1.70 | 19.15 | 1.80–6.40 |
| Absolute lymphocyte count (×109/L) | 1.61 ± 0.66 | 1.55 | 0.52 | 3.24 | 1.00–3.30 |
| Total platelets (×109/L) | 199.61 ± 74.82 | 189.60 | 31.30 | 528.00 | 100–300 |
| Neutrophil-to-lymphocyte ratio | 4.37 ± 3.66 | 3.06 | 0.9 | 24.00 | |
| Platelet-to-lymphocyte ratio | 146.10 ± 89.74 | 124.02 | 33.6 | 512.7 |
As shown in Figure 1, the discriminatory performance for predicting the primary endpoint (all-cause in-hospital mortality) was better for NLR (AUC = 0.644, CI95 0.492–0.797) than for PLR (AUC = 0.599, CI95 0.423–0.776). Both baseline NLR and PLR presented better AUC compared with that 6 h (AUC = 0.377, CI95 0.234–0.519 and AUC = 0.302, CI95 0.181–0.423, respectively) and 24 h after HTX (AUC = 0.440, CI95 0.266–0.615 and AUC = 0.407, CI95 0.227–0.587, respectively). The discriminatory performance of other baseline inflammatory markers was worse than NLR or PLR for predicting the primary endpoint such as absolute white blood cell (AUC = 0.465, CI95 0.190–0.741), absolute neutrophil count (AUC = 0.502, CI95 0.233–0.772), and absolute platelet count (AUC = 0.423, CI95 0.162–0.683).
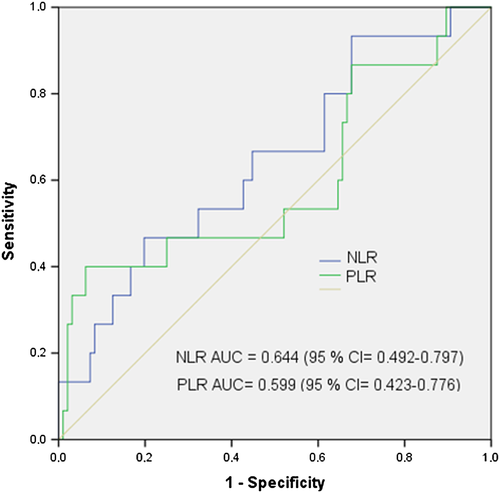
Best cut-off value was 2.41 for NLR, with a sensitivity of 86% and specificity of 67%. Best cut-off value for PLR was 92.5 (sensitivity 86%, specificity 68%). When patients were divided according to the best cut-off value, no significant differences in demographic features were observed between the low and high groups for either NLR or PLR (Table 2), although high NLR patients showed increased leucocytes, and both high NLR and PLR groups showed reduced estimated glomerular filtration rate, but values were within normal range for all the groups. Surgical variables like total bypass time were not significantly different among groups (Table 2).
| Low NLR (≤2.41), n = 31 | High NLR (≥2.41), n = 80 | P | Low PLR (≤92.5), n = 32 | High PLR (≥92.5), n = 79 | P | |
|---|---|---|---|---|---|---|
| Recipient age (years) | 47.03 ± 10.49 | 51.36 ± 2.28 | 0.08 | 47.78 ± 13.04 | 51.11 ± 11.38 | 0.18 |
| Male sex (%) | 65 | 73 | 0.40 | 81 | 66 | 0.10 |
| Body mass index | 25.61 ± 4.46 | 25.29 ± 3.72 | 0.70 | 25.98 ± 4.44 | 25.14 ± 3.69 | 0.31 |
| Pre-transplantation hypertension (%) | 39 | 40 | 0.90 | 47 | 37 | 0.32 |
| Pre-transplantation diabetes (%) | 16 | 13 | 0.61 | 19 | 11 | 0.30 |
| History of smoking (%) | 45 | 46 | 0.91 | 44 | 47 | 0.76 |
| Ischaemic cardiomyopathy (%) | 29 | 35 | 0.55 | 34 | 33 | 0.88 |
| Pulmonary vascular resistance (Woods units) | 2.56 ± 1.02 | 2.58 ± 1.08 | 0.94 | 2.55 ± 1.11 | 2.58 ± 1.04 | 0.88 |
| Status on waiting list | 0.17 | 0.20 | ||||
| Elective | 6 | 6 | 13 | 4 | ||
| Urgent | 87 | 73 | 69 | 80 | ||
| Emergent | 6 | 21 | 19 | 16 | ||
| White blood cell (×109/L) | 6.99 ± 2.08 | 8.91 ± 2.99 | ≤0.001 | 8.54 ± 2.25 | 8.30 ± 3.12 | 0.69 |
| Neutrophil (%) | 53.72 ± 7.05 | 69.56 ± 8.23 | ≤0.001 | 58.57 ± 11.41 | 67.79 ± 9.11 | ≤0.001 |
| Lymphocyte (%) | 31.80 ± 5.32 | 16.61 ± 6.15 | ≤0.001 | 27.31 ± 9.06 | 18.24 ± 7.66 | ≤0.001 |
| Platelets (×109/L) | 191.0 ± 54.5 | 202.9 ± 81.4 | 0.45 | 157.2 ± 53.7 | 216.7 ± 75.6 | ≤0.001 |
| Creatinine (mg/dL) | 1.01 ± 0.24 | 1.23 ± 0.49 | 0.02 | 1.07 ± 0.29 | 1.20 ± 0.49 | 0.16 |
| eGFR (mL/min per 1.73 m2) | 74.91 ± 16.36 | 64.29 ± 24.96 | 0.03 | 74.26 ± 20.23 | 64.29 ± 24.04 | 0.04 |
| Lactate (mmol/L) | 1.48 ± 0.49 | 1.54 ± 1.23 | 0.77 | 1.80 ± 1.88 | 1.41 ± 0.43 | 0.08 |
| Bypass time (min) | 112.3 ± 22.20 | 119.64 ± 35.31 | 0.28 | 115.0 ± 33.58 | 118.5 ± 31.8 | 0.60 |
| Aortic cross clamp donor-to-recipient time (min) | 168.4 ± 49.70 | 179.4 ± 46.76 | 0.28 | 171.1 ± 46.45 | 178.3 ± 48.23 | 0.47 |
| Peak glucose level (mg/dL) during first 24 h after HTX | 322.7 ± 91.47 | 306.6 ± 94.19 | 0.41 | 317.6 ± 106.7 | 308.5 ± 87.89 | 0.64 |
| Peak lactate level (mmol/L) during first 24 h after HTX | 8.16 ± 3.05 | 7.65 ± 2.93 | 0.41 | 8.54 ± 3.11 | 7.49 ± 2.86 | 0.09 |
- eGFR, estimated glomerular filtration rate; HTX, heart transplantation; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio.
Overall in-hospital mortality was 13.5%. The most frequent cause of death during early recovery was sepsis (4.5%), followed by primary graft dysfunction (3.6%), right ventricular failure (3.6%), and cellular rejection (1.8%). In-hospital mortality, the primary endpoint of the study, was significantly higher in the high NLR group (17.5% vs. 3.2%, P < 0.05), while PLR showed a non-significant trend (16.5% vs. 6.3%, P = ns). One year mortality was more than two times increased for both high NLR and high PLR groups, although it did not reach statistical significance (25% vs. 9.7% for NLR; and 25.3% vs. 9.4% for PLR, P = ns) for any marker. After hospital discharge, most frequent causes of death were cellular rejection (1.8%) and sudden death (1.8%). Log-rank test of the Kaplan-Meier curves (Figure 2) showed a trend towards an increase in 1 year mortality for both the high NLR group and the high PLR group, although it did not reach statistical significance (P = ns for both). RRT (Figure 3) was significantly higher in both the high NLR group (33.8% vs. 0%, P < 0.001) and the high PLR group (32.9% vs. 3.1%, P < 0.001).

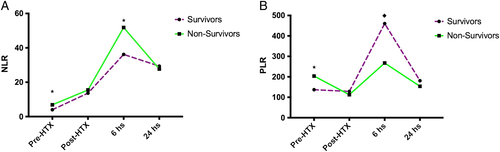
Both NLR and PLR values were increased after surgery, showing a peak at 6 h. When patients that did not survive were analysed, absolute baseline and 6 h NLR and PLR values were significantly higher than those of survivors (Figure 4). However, NLR and PLR values were not significantly lower among survivors immediately after HTX and at 24 h.
Univariate analysis (Table 3) identified the following factors significantly affecting 1 year mortality: pre-transplantation diabetes [hazard ratio (HR) = 2.943], higher baseline creatinine concentrations (HR = 3.547), lower estimated glomerular filtration rate (HR = 0.973), longer bypass time (HR = 1.019), and higher NLR (≥2.41, HR = 3.068). Multivariate analysis (Table 3) indicated that only high NLR (HR = 3.403, 95% CI95 1.039 -11.144, P < 0.05) and pre-transplant diabetes (HR = 3.364, CI95 1.041 -10.868, P < 0.05) were independent prognostic factors for 1 year mortality after adjustment.
|
Univariate analysis HR (CI95) |
Multivariate Cox regression analysis | P | |
|---|---|---|---|
| Recipient age > 50 years | 1.641 (0.680–3.957) | ||
| Male sex | 0.869 (0.339–2.224) | ||
| Pre-transplantation diabetes | 2.943 (0.960–9.025)* | 3.364 (1.041–10.868) | 0.04 |
| Ischaemic cardiomyopathy | 1.072 (0.439–2.620) | ||
| Pulmonary vascular resistance | 1.191 (0.808–1.756) | ||
| Serum creatinine (mg/dL) | 3.547 (1.283–9.806)* | ||
| eGFR (mL/min per/1.73 m2) | 0.973 (0.953–0.994)* | ||
| Bypass time (min) | 1.019 (1.004–1.035)* | ||
| NLR ≥ 2.41 | 3.068 (0.970–9.705)* | 3.403 (1.039–11.144) | 0.04 |
| PLR ≥ 92.5 | 1.086 (0.423–2.789) |
- CI95, 95% confidence interval; eGFR, estimated glomerular filtration rate; HR, hazard ratio; NLR, neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio.
- * P ≤ 0.01 at univariate analysis.
Discussion
The NLR and PLR are inflammatory markers that are widely available and at very low cost. Growing evidence has shown predictive value of these markers in several cardiac conditions including stable coronary artery disease, acute coronary syndromes, HF, and cardiac surgery.11 However, the role of these markers in HTX remains unknown.
In the present study, we have shown that higher NLR at baseline is significantly associated with increased in-hospital mortality, and the need for RRT. Moreover, baseline NLR has shown to be an independent predictor factor for 1 year mortality on multivariate analysis. On the other hand, higher PLR at baseline was not significantly associated with higher in-hospital mortality, although it was associated with the need for RRT. One year mortality was not statistically significantly associated with any of the markers. This discrepancy among in-hospital mortality and long-term mortality for NLR may be explained by the few number of patients included, considering that there was a more than two-fold absolute difference. However, long-term mortality may reflect other causes independent of baseline inflammation like graft vascular disease, chronic rejection, and/or malignancies.
Although peak inflammation as assessed through the PLR and NLR occurred 6 h after HTX, only baseline (before HTX) and 6 h levels were significantly associated with mortality and RRT, while immediately after HTX and 24 h showed no significant predictive value. Most studies evaluating NLR and PLR for cardiac surgery showed predictive value of these markers before surgery,19 similar to our study in HTX. One study, however, showed that both pre-operative and post-operative (48 h) higher NLR values were associated new atrial fibrillation in patients undergoing CABG.20 Another study in patients undergoing transcatheter aortic valve replacement showed that higher increase in NLR after valve implantation was associated with worse survival.21 Of note, baseline NLR in the same study was not associated with survival. In HTX, patients routinely receive immunosuppressive therapy including high-dose steroids, starting within surgery and continued afterwards. Steroids increase neutrophils and decrease lymphocytes, thus modifying both NLR and PLR.22 Therefore, post-surgical values may not accurately reflect inflammation in these patients. Six hours after HTX, peak inflammation was observed and was increased in non-survivors. However, the prognostic value of baseline NLR was better than that of 6 h, as expressed by both AUC and multivariate analysis. Although immunosuppressive treatment is tailored according to allograft rejection, all patients received the same high-dose steroids in the study period (first 24 h), and tailored therapy started afterwards. Therefore, individual differences in steroids treatment are unlikely to account for the results.
Secondary outcomes of the present study included long-term (1 year) mortality and the need for RRT. Acute kidney injury after HTX is a strong predictor of mortality, and therefore RRT can be considered a clinically relevant endpoint.23-25 Both NLR and PLR were significantly associated with RRT.
Baseline NLR AUC for in-hospital mortality was 0.664 in our study, showing 86% sensitivity and 67% specificity. Studies in different cardiac conditions evaluating different endpoints have showed different values. NLR AUC in our study in HTX showed better performance for in-hospital mortality compared with the AUC for predicting major adverse cardiovascular events after percutaneous coronary interventions,26 or saphenous vein graft disease,27 and atrial fibrillation20 after CABG. On the contrary, other studies have showed better NLR AUC for mortality both in HF28, 29 and in non-ST elevation myocardial infarction.30 The results for PLR were different, and most studies have showed a better predictive value in ST elevation myocardial infarction,13-15 HF,28, 29 and transcatheter aortic valve replacement,21 and after percutaneous coronary interventions26 or after implantable cardioverter defibrillator placement.18 Of note, only few studies analysed the predictive value of PLR for mortality, and most showed predictive value in surrogate endpoints.
In the present study, we have also performed a head-to-head comparison of the two studied markers of inflammation: NLR and PLR. Although both markers have shown prognostic value in several cardiac conditions, few studies have compared them. We have found that NLR was a more useful marker at ROC curve, similar to studies in HF.28, 29 Besides, in our study, NLR—but not PLR—was independently associated with 1 year mortality on multivariate analysis, in accordance with one study in HF.28 Moreover, NLR was also associated with increased in-hospital mortality.
The present study has several limitations: first, this is a single-centre, retrospective analysis. Second, only few time points were analysed after HTX and within the first 24 h, and NLR/PLR values after 24 h were not analysed. Third, for the multivariate analysis, no more than two variables where analysed in order to avoid overfitting. Finally, although we found a more than two-fold increase in 1 year mortality in both the high NLR and high PLR groups, none reached statistical significance, and therefore a larger sample size may increase the predictive value for long-term mortality. However, no sample size calculation was performed in this retrospective study. Nevertheless, the results of the present study show that PLR and specially NLR are both useful, low-cost, widely available prognostic markers for patients undergoing HTX. NLR, but not PLR, was associated with in-hospital mortality and was an independent predictor for 1 year mortality on multivariate analysis. Both NLR and PLR were predictors of RRT.
Antigen-specific responses to cardiac allograft are the target for standard immunosuppressive treatment after HTX. However, the innate non-antigen-mediated immune response plays a critical role in myocardial performance and HTX.31 Several inflammatory pathways are activated both before and after HTX, including infiltrating cells like neutrophils and lymphocytes, inflammatory cytokines like IL-1 and IL-18, the NLRP3 inflammasome, and toll-like receptor activation.31, 32 Experimental studies have shown that modulating the innate inflammatory response is associated with improved survival after HTX, yet there is no specific approved treatment in this direction. Our study confirms the association between increase innate inflammation and worse outcome in HTX and strengthens the need for specific treatments. Moreover, patients with an increased baseline NLR represent a higher-risk group that may benefit the most from these treatments.
In conclusion, baseline NLR and PLR are both associated with worse outcome after HTX, although NLR was a better predictor.
Acknowledgement
Iván Constantin, MD, is acknowledged for his contribution to the database.
Conflict of interest
None declared.
Funding
None.