A Simple and Effective Method for Flow Cytometric Study of Lymphoid Malignancies Using Needle Core Biopsy Specimens
Conflict of interest: The authors declare no conflict of interest.
Abstract
Objectives
We developed a simple and effective rinsing technique (RT) of needle biopsies to produce cell suspensions for flow cytometry (FCM) and evaluated whether the RT is comparable to the conventional tissue cell suspension (TCS) technique.
Methods
We retrieved 93 needle core biopsy cases employing the RT for FCM and 25 needle biopsy cases using TCS for FCM.
Results
The diagnostic concordance between the FCM results and the morphologic diagnoses of both groups was compared. The diagnostic concordance was comparable in the RT group (92.6%) to the TCS group (71.4%). Furthermore, the diagnostic concordance in the RT group was associated with number of isolated cells. The diagnostic accuracy increased significantly when the cell number was above 30,000 in the RT group.
Conclusions
The RT for FCM not only maximizes the tissue utilization, but also is a simple and effective method to obtain cell suspension as compared to traditional cell suspension technique. © 2018 International Clinical Cytometry Society
Over the last several years, hematopathologists have seen a dramatic increase in the number of needle core biopsy specimens from patients with suspected lymphoid malignancies. Such practice has its benefits. For instance, patients avoid an excisional biopsy which requires surgery with general anesthesia and a longer hospital stay with potentially increased morbidity 1, 2. Meanwhile, there is an increasing expectation for hematopathologists to provide a definitive diagnosis with smaller amount of tissue. A general agreement in the literature is that ancillary studies such as immunohistochemistry, cytogenetics, molecular studies, and flow cytometry (FCM) are often necessary for making definitive diagnosis in needle core biopsy specimens 1-5. The benefits of FCM as an ancillary study in the diagnosis of lymphoma is well established 4-6. Sacrificing tissue for ancillary studies, however, is often problematic. Splitting the specimen poses the threat of disparate sampling: the core sent for FCM may not be representative of the core sent for histology, and vice versa. Likewise, the remaining tissue may be insufficient in quantity or quality for an accurate and definitive histologic diagnosis. For many of these reasons, hematopathologists have been cautious of utilizing ancillary studies such as FCM in the setting of triaging and diagnosing lymphoid malignancies using needle core biopsy specimens.
Since 2014, our institution started to adopt a cell suspension “rinsing” technique of the core biopsy specimens within RPMI media to maximize the benefit of FCM as an ancillary study while preserving the maximum amount of diagnostic tissue for microscopic examination. Herein, we demonstrated that a cell suspension within RPMI medium, devoid of tissue, is sufficient for accurate flow cytometric analysis and the results are comparable to traditional tissue cell suspension (TCS) technique. To our knowledge, very little information is published regarding the rinsing technique (RT) for FCM as we described here, although a couple of studies using “vortex” method, especially for bone marrow core biopsy specimens, have been reported 7, 8. Most of the literature pertains to the advantageous benefits of FCM for lymphoma diagnosis 1, 4, 6. Our findings suggest this simple RT would maximize the benefit of both microscopic diagnosis and FCM analysis.
MATERIALS AND METHODS
Patient Cohorts and Study Design
We retrospectively reviewed 118 needle core biopsy specimens with a suspected diagnosis of lymphoma and with concurrent FCM analysis performed at our institution from September 1, 2014 to July 5, 2016. These included 93 cases in which a cell suspension for FCM was obtained using the RT and 25 cases in which it was obtained using conventional TCS. A total of 16 cases (12 cases of the RT group, 12.9%; and 4 cases of the TCS group, 16.0%) yielded an insufficient cell number for FCM within the cohorts. FCM was performed on the rest of cases, including 81 cases (81/93; 87.1%) within the RT group and 21 cases (21/25; 84%) of the TCS group. All the biopsies were obtained under imaging (ultrasound or computed tomography) guidance. We classified the lesion site into superficial versus deep-seated, and lymph node versus extranodal lesions. The superficial lesions included the cervical and clavicular regions, axilla, and groin; the deep-seated lesions included the thorax, abdomen, retroperitoneum, and pelvis regions.
The “RT” was performed as the following. When fresh tissue cores were received in the lab, one to three representative cores were submerged and stirred gently (rinse) for three to four times in RPMI 1640 medium using sterile forceps at room temperature before processed in 24-h-formalin fixation for histology. Other cores were directly fixed for histology. The fresh specimens were handled within an hour upon receiving. The cell suspension in RPMI medium, devoid of tissue, was sent for FCM analysis within 24 h of collection. If the cell suspension arrived before 15:00, it was processed immediately at the room temperature. If the cell suspension arrived after 15:00, it was kept at 4°C in the refrigerator overnight and was processed next morning. The TCS technique was performed using the traditional protocol in which a single representative tissue core or a portion of the representative tissue core was disaggregated mechanically with knives and needles to produce a cell suspension for FCM analysis. The rest of the submitted tissue or other cores were processed for histology.
Morphological and Flow Cytometric Analyses
Morphologically, the cases of needle core biopsy with adequate material were evaluated by hematopathologists based on the World Health Organization (WHO) classification of tumors of hematopoietic and lymphoid tissues 2008 9. The specimen was designated as insufficient for morphologic evaluation if it was too small or unreadable due to extensive necrosis, severe crush, or fixation artifact. An excisional biopsy was recommended if a specific diagnosis could not be made.
The cell suspensions derived from the RT and the TCS were submitted for FCM. Eight-color flow cytometric analysis was performed on FACSCanto II (BD Bioseciences, San Jose, CA) according to the standard procedures 10, and data were analyzed using the Kaluza analysis software (Beckman Coulter, Indianapolis, IN). Based on the cell number recovered, one B-cell tube including CD45, CD19, CD5, CD10, CD23, CD38, and surface immunoglobulin light chains (kappa and lambda) or two tubes including both B-cell tube and T/NK-cell tube (CD3, CD7, CD4, CD8, CD14, CD16, CD45, and CD56) were performed. Cells were also permeabilized for intracytoplasmic staining of immunoglobulin light chains for cases suspicious for plasma cell neoplasm. A diagnosis of B-cell non-Hodgkin lymphoma (B-NHL) was made in the presence of a monotypic B-cell population with a restricted (monotypic) light chain expression and/or aberrant antigen expression. T-cell lymphoproliferative disorder was diagnosed if there was a T-cell population with aberrant phenotypes such as lacking and/or abnormal distribution of one or more T-cell antigens. A case was considered suspicious for lymphoproliferative disorder if analysis detected a borderline light-chain excess or a small subset of monotypic B-cells or abnormal T-cells.
Statistical Analysis
All statistical analyses were performed using SPSS 17.0 statistical software package (SPSS Inc., Chicago, IL). The unpaired Student's t test was used to evaluate the difference of age distribution between the RT group and the TCS group. The comparisons of the cell number, cores for FCM, and length of the core tissue between the two groups were analyzed by Mann–Whitney U test. The distribution of lesion sites and tubes for FCM in the two groups of the entire cohort was analyzed using Pearson's χ2 test. Fisher's exact test was used to analyze the difference in diagnostic concordance between the two groups, because χ2 test assumptions were not met. Likewise, the association between the length of core tissues and cell number for FCM and the diagnostic concordance in the total cohort and the WT group was also analyzed by χ2 test. The data with a normal distribution were expressed as the mean ± standard deviation, and the median (range) was used to express the data with a non-normal distribution. All tests were two-tailed, and a P value of <0.05 was considered significant.
RESULTS
Patient Cohorts and Tissue Biopsy
The patient age, biopsy site, and amount of core biopsy tissue are summarized in Table 1. No significant difference was found in age, total length of tissue, isolated cell number, and number of tubes performed for FCM between the RT and the TCS groups. The RT group had more cases from superficial and nodal lesion than the TCS group (P = 0.045 and P = 0.021, respectively).
| Variables | Rinsing group | Tissue cell suspension group | P-value |
|---|---|---|---|
| n = 81 | n = 21 | ||
| Age, mean ± SD, years | 57 ± 18 | 55 ± 17 | 0.62 |
| Lesion site, no. (%) | |||
| Superficial | 43 (53.1) | 6 (28.6) | 0.05 |
| Deep-seated | 38 (46.9) | 15 (71.4) | |
| Lesion site, no. (%) | |||
| Nodal | 46 (56.8) | 6 (28.6) | 0.02 |
| Extranodal | 35 (43.2) | 15 (71.4) | |
| Total length of core tissue, median (range), mma | 21.5 (4.0–90.0) | 17.0 (3.0–90.0) | 0.18 |
| Cell number, median (range), ×106 | 0.10 (0.001–2.3) | 0.20 (0.007–10.57) | 0.54 |
| Tubes for flow, no. (%) | |||
| 1 tube | 44 (54.3) | 9 (42.9) | 0.35 |
| 2 tubes | 37 (45.7) | 12 (57.1) |
- a mm, millimeter.
Diagnostic Concordance of the Two Cell Suspension Techniques
We compared the concordance between FCM results and morphologic diagnosis in the RT and the TCS groups (Table 2). The diagnostic concordance rate of the RT group (92.6%) was higher than or at least not inferior to the TCS group (71.4%) (P = 0.016; Table 2). More specifically, the concordance between FCM and morphology reached 100% in low-grade B-cell lymphomas in both the RT group (21 cases) and the TCS group (5 cases). Twenty-one cases of low-grade B-cell lymphomas in the RT group include ten follicular lymphoma, five mantle cell lymphoma, four marginal zone lymphoma, and two chronic lymphocytic leukemia/small B-cell lymphocytic lymphoma. In these cases, FCM studies provided strong support to the final diagnosis, with much shorter turn-round time (24 h for FCM studies, 24–48 h for immunohistochemical (IHC) stains, and three–four days for molecular studies), and less expenses (eliminate the necessities for extensive IHC panels, and possible molecular and cytogenetic studies). For reactive and atypical lymphadenopathies, FCM and morphologic evaluation also showed high concordance rate [25/26, (96.2%) in RT and 5/6 (83.3%) in TCS group, respectively]. For those less common entities, including classical Hodgkin lymphoma, unclassified B cell lymphoma, myeloid sarcoma, post-transplantation lymphoproliferative disorder, plasma cell dyscrasia, follicular dendritic cell neoplasm, and others, FCM may also be helpful but the number of cases in each of these entities were too small for a definitive conclusion. A negative FCM finding for cases of classical Hodgkin lymphoma and follicular dendritic cell neoplasm was considered concordant to morphologic diagnosis given limited panels with B- and T-cell markers were used for analyses and difficulties to detect rare Hodgkin cells by FCM. In the case of metastatic adenocarcinoma, a significant CD45-negative population of intermediate-to-large sized cells consistent with non-hematopoietic cells was identified by FCM. Two cases deemed inadequate by morphology were both negative by FCM. Discordance between FCM and morphologic diagnosis was mainly identified in diffuse large B-cell lymphoma (DLBCL), in both RT and TCS groups. In RT group, 13 of 17 cases (76.5%) of DLBCL were successfully identified by FCM studies; whereas in TCS group, FCM studies were negative in four of six cases (66.6%) of DLBCL. Overall, there were 8 of 23 DLBCL cases (34.8%) had a negative FCM diagnosis, probably due to those large neoplastic cells did not survive the harsh of tissue sampling and FCM processing. In our study, one ALK-positive anaplastic large cell lymphoma case was also missed by FCM in the RT group as only one B-cell tube, but not the T-cell tube, was performed due to the low cell yield and lack of prior clinical history.
| Morphological diagnosisa | Rinsing group | Tissue cell suspension group | ||||
|---|---|---|---|---|---|---|
| No. | Concordant (%) | Discordant (%) | No. | Concordant (%) | Discordant (%) | |
| Low grade B-cell lymphomab | 21 | 21 (100) | 0 | 5 | 5 (100) | 0 |
| Diffuse large B-cell lymphoma | 17 | 13 (76.5) | 4 (23.5) | 6 | 2 (33.3) | 4 (66.7) |
| Reactive | 14 | 13 (92.9) | 1 (7.1) | 4 | 3 (75.0) | 1 (25.0) |
| Atypical/Suspicious | 12 | 12 (100) | 0 | 2 | 2 (100) | 0 |
| CHLc | 4 | 4 (100) | 0 | 2 | 1 (50) | 1 (50) |
| B-UCLd | 2 | 2 (100) | 0 | |||
| T-cell Lymphoma | 2 | 1 (50.0) | 1 (50.0) | |||
| Myeloid Sarcoma | 2 | 2 (100) | 0 | 1 | 1 (100) | 0 |
| PTLDe | 2 | 2 (100) | 0 | |||
| INADf | 2 | 2 (100) | 0 | 1 | 1 (100) | 0 |
| Plasma cell dyscrasia | 1 | 1 (100) | 0 | |||
| FDCNg | 1 | 1 (100) | 0 | |||
| Adenocarcinoma | 1 | 1 (100) | 0 | |||
| Total | 81 | 75 (92.6) | 6 (7.4) | 21 | 15 (71.4) | 6 (28.6) |
- a Diagnosis category referred to the overall final histologic diagnosis.
- b Low grade B-cell Lymphoma included chronic lymphocytic leukemia/small B-cell lymphocytic lymphoma (CLL/SLL), mantle cell lymphoma (MCL), marginal zone lymphoma (MZL), and follicular lymphoma (FL).
- c CHL, classical Hodgkin lymphoma.
- d B-UCL, unclassified B-cell lymphoma.
- e PTLD, post-transplantation lymphoproliferative disorder.
- f INAD, inadequate for evaluation by histology.
- g FDCN, follicular dendritic cell neoplasm.
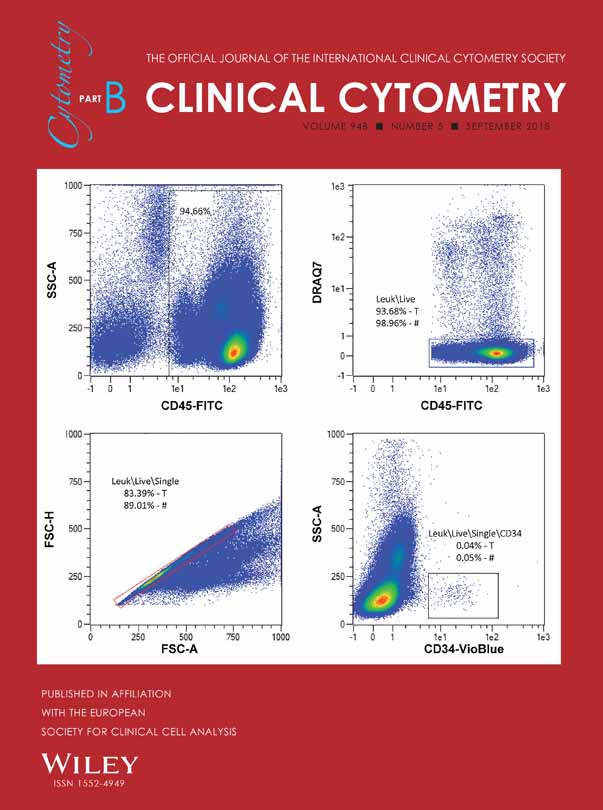
Herein, we presented a representative case of nodal marginal zone lymphoma detected by morphology and FCM using the rinsing method in Figure 1. Two specimen containers including one in formalin (two cores) and one in RPMI media (one core) were received. The core identified within the RPMI container measures 0.4 cm × 0.2 cm × 0.1 cm. The specimen was “dipped” or “stirred” gently (rinsing method) in RPMI-1640 medium. The biopsy fragment was then submitted to pathology department for histologic evaluation while the RPMI media was sent for FCM. The number of cells isolated from RT for FCM were 200,000 with >85% viability, adequate for one B-cell tube of eight antibody panel. A clonal mature B-cell population was detected in 60% of lymphocytes. Morphology evaluation shows that both the cores fixed in formalin and the core in the RPMI media (after rinsing method) show adequate morphology with similar appearance, and were diagnostic for marginal zone lymphoma.

A representative case of lymph node needle core biopsy with nodal marginal zone lymphoma detected by morphology and immunohistochemical stains. H&E section showing nodular lymphoid infiltrates composed of monocytoid small B-cells and scattered plasma cells (A, H&E, 200×; B, H&E, 400×). The atypical lymphocytes were positive for CD20 (C, 400×). The isolated cells from core biopsy rinsing were used for FCM with adequate viability. Findings were consistent with a low-grade B-cell lymphoproliferative disorder. A clonal mature B-cell population expressing CD19, CD20, CD24, and low to intermediate density lambda light chains (D) was detected in 60% of lymphocytes.
Association Between the Length of Tissue Core and Cell Number for FCM and the Diagnostic Concordance
We next evaluated whether the length of the core biopsy and cell number affect the diagnostic accuracy by FCM. Results are presented in Table 3. In the entire cohort (combined TCS and RT groups) and the RT group, there was no significant difference of either concordant or discordant rates among varying tissue length for FCM. However, we found that the cell number was closely associated with the diagnostic concordance in the RT group (P = 0.042). The diagnostic accuracy increased significantly when the cell number was above 30,000 (Table 3).
| Variables | Entire cohort | P-valuea | Rinsing group | P-valuea | ||
|---|---|---|---|---|---|---|
| Concordant (%) | Discordant (%) | Concordant (%) | Discordant (%) | |||
| Total length of core tissue (mm)b | ||||||
| Below 15 | 27 (87.1) | 4 (12.9) | 0.472 | 21 (95.5) | 1 (4.5) | 0.874 |
| 15–29 | 31 (83.8) | 6 (16.2) | 27 (90.0) | 3 (10.0) | ||
| Above 29 | 29 (93.5) | 2 (6.5) | 26 (92.9) | 2 (7.1) | ||
| Cell number for FCMc, ×106/mL | ||||||
| Below 0.030 | 20 (76.9) | 6 (23.1) | 0.052 | 16 (80.0) | 4 (20.0) | 0.042 |
| 0.030–0.20 | 42 (95.5) | 2 (4.5) | 37 (94.9) | 2 (5.1) | ||
| Above 0.20 | 25 (92.6) | 2 (7.4) | 21 (100) | 0 (0.0) | ||
- a P values were calculated by the χ2 test (χ2 test).
- b mm, millimeter; The lengths of tissue core of 99 cases in the total cohort, and 80 cases in the RT group, respectively, were analyzed. The lengths of three cases could not be calculated due to the minute size of the fragments; one belonged to the RT group, another two specimens were in the tissue core suspension group.
- c FCM, flow cytometry; the cell numbers of 97 cases in the total cohort, and 80 cases in the RT group, respectively, were analyzed. The cell numbers of five cases could not be calculated due to insufficient quantity; one belonged to the washing technique group, another four specimens belonged to the tissue core suspension group.
DISCUSSION
With the advent of molecular biology and medical imaging, less aggressive and more cost-effective procedures 11, such as imaging-guided needle core biopsy with FCM, have been advocated for the diagnosis of lymphoma 12-14. Though the ability to diagnose lymphoproliferative disorder by core biopsy is well established 15-18, the accuracy of this procedure alone in replacing excisional biopsies for primary diagnosis and sub-classification of lymphoma is controversial 1, 19. The major disadvantages of needle core biopsy, compared to excisional biopsy, include smaller amounts of tissue, potentially more artifacts of fixation and processing, and insufficiency for ancillary studies. These limitations of needle core biopsy are the challenges for the pathologic diagnosis 20, 21. Therefore, there is a growing need to perform ancillary studies to increase the diagnostic accuracy of lymphoma and preserve the maximum amount of tissue for microscopic evaluation and IHC stains. FCM offers rapid and objective cell surface phenotyping quantitatively and qualitatively. It is an essential adjunctive method for diagnosis and subclassification of the lymphoma in core biopsy specimens 22, 23. The routine method uses a small portion of the core biopsy tissue to produce cell suspensions for FCM and the rest of the tissue is processed for histology. This method has several drawbacks: 1 the tissue core sent for FCM may not be representative of those sent for histology by splitting the specimen, and vice versa; 2 the rest of tissue core may not be sufficient in quantity or quality for histologic diagnosis; and 3 FCM technologists need to spend additional time on preparing cell suspension from tissue.
The RT for FCM used in our study avoids the aforementioned drawbacks. It is a simple and quicker way to acquire the cell suspension and it maximizes the tissue for histology evaluation while obtaining sufficient number of cells for FCM. Moreover, simply rinsing the tissue core in RPMI medium prevented the processing artifacts and potential morphologic distortion which may be encountered in “vortex” method 7, 8. In our study, the number of cells recovered and total length of core tissue in the RT group were comparable to the TCS group. The percentage of cases with sufficient cell number for FCM was also similar, 87% in the RT group and 84% in the TCS group. These results indicate that the cell acquisition ability of the RT is equivalent to the traditional TCS technique. Surprisingly, the RT group showed a better, or at least equivalent, diagnostic concordant rate (92.6%) compared to the TCS group (71.4%) between morphologic and FCM diagnoses. However, there were case selection biases including more cases from deep-seated sites and a higher percentage of DLBCL cases in the TCS group compared to the RT group (28.6% in TCS vs. 21.0% in RT group), which might result in a lower concordant rate in the TCS group. The diagnostic concordance rate in the TCS group is comparable to that reported in the literature. Dong et al. found that morphology coupled with FCM analysis provided definitive diagnoses of lymphoma in 77% of the cases and 82% of NHLs in the fine-needle aspiration biopsy (FNAB) specimen 1. Meda et al. also found cytology combined with FCM in FNAB specimens were able to correctly diagnose and to subclassify lymphoma in 77% of NHL 19. Whereas the concordance between morphologic review and FCM in low-grade B-cell lymphoma was very high, the majority of the discordant cases were DLBCL in both RT and TCS groups. It has been well recognized that DLBCL would be missed by FCM due to a number of reasons, such as cell necrosis, tissue fibrosis, dying of large cells during the FCM process, sampling bias, etc. 19, 24, 25.
Some studies showed that the diagnostic accuracy increased with tissue core length and volume for the TCS method 2, 5, 26, 27. One study recommended that the size of the biopsy needle should be 19 gauge or larger, and there should be at least 3 to 4 tissue cores at least 5–10 mm in length each (total length, 15–30 mm or longer) for histologic diagnosis 2. Another study suggested 4 or 5 cores with 14- to 18-gauge needles for morphologic review 5. We tried to determine whether there was a cutoff value of the tissue length and cell number to increase the diagnostic accuracy using the RT for FCM. Our results showed that the number of cells recovered was more important than the tissue length for FCM. The cell number, but not tissue length, was associated with the diagnostic concordance (P = 0.042). When the cell number was above 30,000, the diagnostic accuracy increased significantly (Table 3).
Herein, we demonstrated that the RT had a high sensitivity and specificity on assisting diagnosis using the needle core biopsy for the cases with clinically suspected lymphoma. Flow cytometric RT in needle core biopsies is an effective way to maximize tissue utilization and is a favorable simple method as compared to the traditional TCS technique. Therefore, we advocate that the simple RT could replace the TCS in core biopsy cases, especially in the cases with minimal amount of tissue. Nevertheless, our study is a mere retrospective study of the cases, larger scale of prospective and potential double blind study to directly compare the sensitivity and specificity of both RT and TCS techniques is warranted.