Novel Pathogenic Variant in Exon 31 of the TSC2 Gene Associated With a Severe Phenotype of Tuberous Sclerosis
1 Introduction
Tuberous sclerosis complex (TSC) is an autosomal dominant neurocutaneous disorder caused by variants of the TSC1 (tuberous sclerosis complex 1) or TSC2 (tuberous sclerosis complex 2) tumor suppressor genes, which regulate cellular proliferation through the mTOR (mammalian target of rapamycin) pathway [1, 2]. TSC has complete genetic penetrance but variable expressivity between patients, which leads to a broad phenotype [1, 3]. Diagnosis is based on major and minor clinical criteria, but identification of a pathogenic genetic variant can be sufficient for early diagnosis in the absence of clinical features [4, 5]. Pathogenic variants are those that prevent protein synthesis or lead to loss of protein function; these are commonly nonsense or frameshift mutations or large deletions [5]. Pathogenic variants have been identified in all other TSC2 exons in the literature; however, variants in exons 25 and 31 have not been associated with loss of protein function or severe symptoms of disease. It has been hypothesized that this occurrence is due to alternative splicing mechanisms in these exons [2].
2 Patient Presentation
This 2-month-old boy completed genetic testing shortly after birth due to a family history of TSC. A paternal aunt with hypomelanotic macules was previously diagnosed with TSC, and additional family members had cutaneous features of the disease. Genetic testing of our patient showed a heterozygous frameshift variant in exon 31 of TSC2 (NM_000548.5) c.3786dupA p.Pro1263ThrfsTer59, classified as a likely pathogenic variant (based on the understanding that a frameshift variant is predicted to lead to loss of protein function) although no patients with this variant leading to clinical disease have been documented. Frameshift variants disrupt the reading frame, changing the downstream amino acid codons and resulting in a truncated protein or a protein that is subject to nonsense-mediated decay.
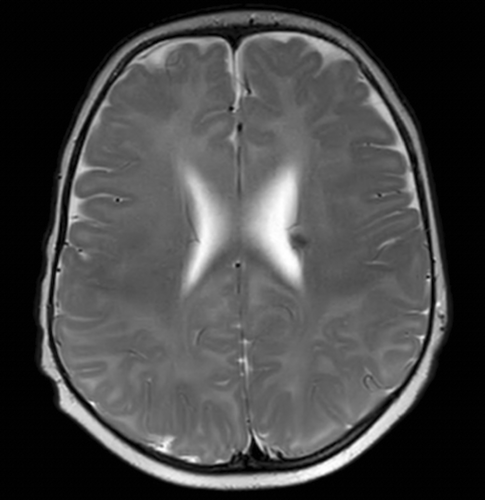
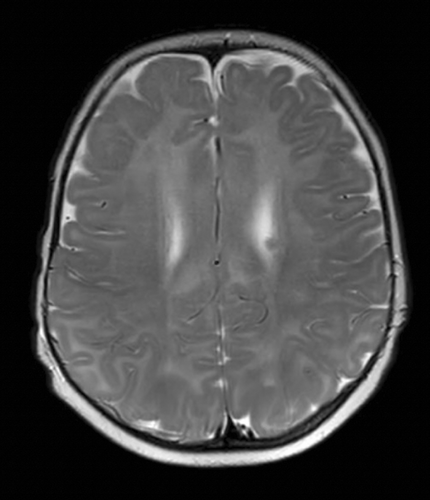
Our patient's paternal aunt had molecular confirmation of the same variant, and the father was considered an obligate carrier with a milder phenotype of the disease. However, parental testing was not completed due to a loss of follow-up. Within the next few months, this patient developed infantile spasms, which were treated with vigabatrin and adrenocorticotropic hormone. Magnetic resonance imaging of the brain at 5 months of age revealed left-sided subependymal nodules, without other abnormalities (Figures 1 and 2). Additional screening (echocardiogram, renal ultrasound, and ophthalmologic evaluation) was completed, and there were no signs of systemic involvement.
3 Discussion
The diagnosis of TSC can be challenging during early life due to broad phenotypic variability. Genetic testing can be useful as a screening tool in patients at risk for disease. Our patient, who was diagnosed with TSC by genetic testing, was initially asymptomatic and later developed severe manifestations of the disease. He had a heterozygous frameshift variant in exon 31 of TSC2, which had previously been considered nonessential to TSC protein complex function due to suspected alternate splicing mechanisms in this region [2]. No other patients with this variant leading to clinical disease have been reported. Our patient demonstrates that variants in exon 31 of TSC2 may lead to severe clinical manifestations of disease in some patients.
4 Conclusion
Tuberous sclerosis is a neurocutaneous disorder caused by variants in the TSC1 or TSC2 genes. Exons 25 and 31 of the TSC2 gene have been considered nonessential to TSC protein complex function based on prior case reports. Our patient demonstrates that variants in TSC2 may still lead to severe features of clinical disease in some patients. Further research is needed to determine the underlying mechanisms behind genotype–phenotype correlations in patients with manifestations of disease.
Author Contributions
Tabitha D'souza: writing – original draft, writing – review and editing. Laura Davids: writing – original draft, writing – review and editing. Prabhumallikarjun Patil: writing – original draft, writing – review and editing.
Conflicts of Interest
The authors declare no conflicts of interest.