Explosive-Onset Epilepsia Partialis Continua and Chorea
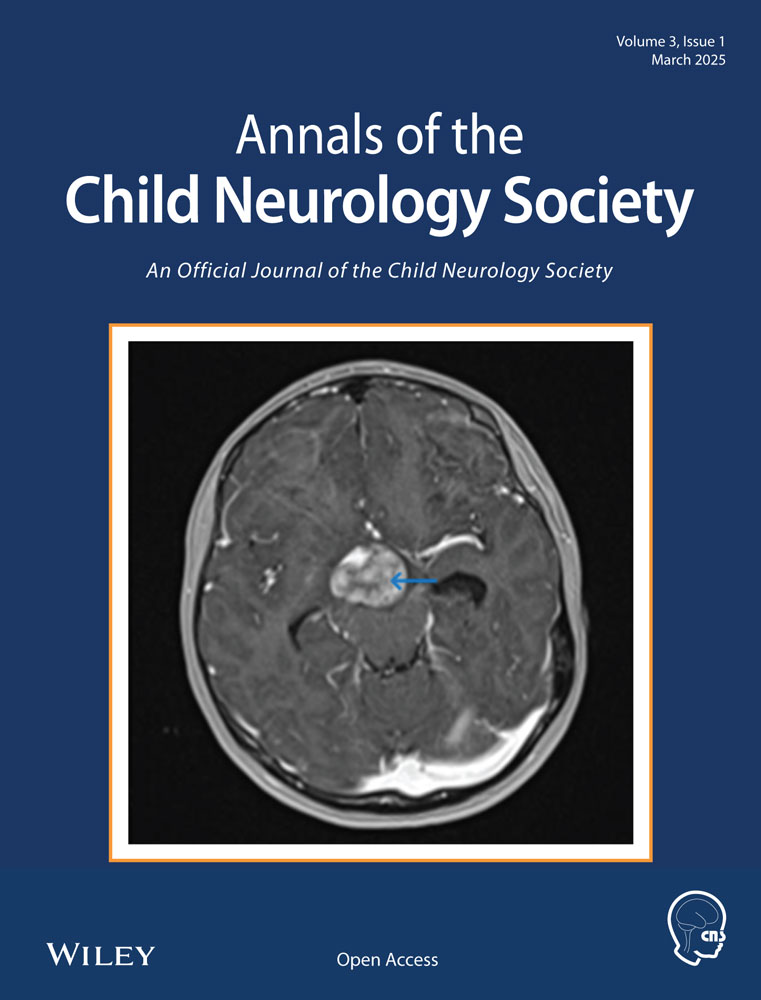
This 2-year-old neurodevelopmentally normal boy presented with abrupt onset of multiple leg clonic seizures with retained awareness (Video 1). Video-electroencephalography confirmed epileptic spikes and ictal onset arising from the vertex region, with an otherwise normal background. Initially controlled with levetiracetam, the seizures evolved to right leg epilepsia partialis continua (EPC). Two weeks later, he developed a hyperkinetic movement disorder reminiscent of chorea-ballismus. One week later, he exhibited developmental regression with encephalopathy, mutism, and insomnia. Anti-N-methyl-d-aspartate receptor (anti-NMDAR) antibody was positive in serum and cerebrospinal fluid, and oligoclonal bands were present. He received intravenous high-dose steroids and intravenous immune globulin and had incremental improvement. By 9 weeks from presentation he had made a remarkable recovery with almost complete symptom resolution.
The vast majority (95%) of children with anti-NMDAR encephalitis will develop a movement disorder, most commonly orofacial-lingual dyskinesias, but these may manifest broadly as chorea, athetosis, ballismus, dystonia, stereotypies, opisthotonus, oculogyric crisis, or bradykinesia [1]. Compared with adults, EPC and movement disorders occur more often as the initial presenting manifestation in children [2]. A diagnosis of anti-NMDAR encephalitis should be considered in young children with new-onset movement disorders and seizures (in particular, EPC), even in the absence of classically associated psychiatric or cognitive symptoms.
Author Contributions
Peter F. Sarnacki: conceptualization, investigation, writing–original draft, methodology, visualization, writing–review and editing, formal analysis, project administration, data curation. Gary Hsich: investigation, visualization, supervision, writing–review and editing. Aaron Abrams: conceptualization, writing–review and editing, visualization, supervision. Sumit Parikh: conceptualization, writing–review and editing, visualization, supervision.
Conflicts of Interest
The authors declare no conflicts of interest.