Symmetric multiple ulceration in a patient diagnosed with Munchausen syndrome
Abstract
We experienced a rare case of Munchausen syndrome with peculiar symmetric ulcers on the whole body. When encountering similar cases with factitious ulceration of the skin, a thorough understanding of the patient's psychiatric condition and a cordial consultation to present illness rather than physical medication might lead to disease stability.
Dear Editor,
A 42-year-old woman had suffered from ulcers over her whole body for the past 2 years. Schizophrenia, hypothyroidism, and trigeminal neuralgia had been under well control by oral medication. Before consulting our hospital, she had continued hospital traveling because multiple ulcers were not improved regardless of immunosuppressive treatments such as systemic steroids and cyclosporine.
A physical examination revealed coappearance of numerous superficial ulcers of artificially similar oval shape and size with re-epithelized scars and pigmented macules across her whole body, except for the upper back (Figure 1A–C). Autoimmune bullous diseases and infectious diseases were excluded based on the laboratory examination findings, and the data related to delay wound healing were within the normal limit. The histopathological findings of the lesion edge on the left thigh (Figure 1D) showed a flattened, superficial skin defect and perivascular neutrophil infiltration in the upper dermis without vasculitis (Figure 1E). Immune deposition of IgG and C3 was not detected. Under an initial diagnosis of pyoderma gangrenosum, oral diphenyl sulfone, a low dose of betamethasone sodium phosphate, and potassium iodine in addition to antibiotics were administered but failed to achieve a cure. Thereafter, we suspected self-induced skin injury since the symptom onset and progression were vague and incoherent.
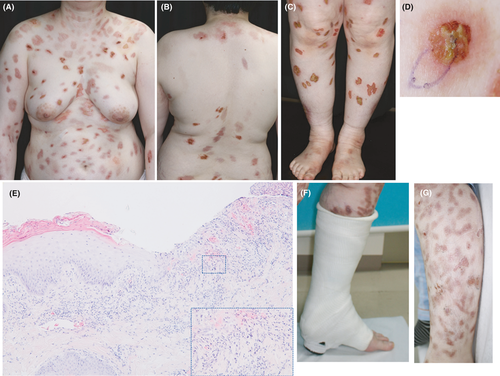
Under her and her mother's approval, we applied a circular cast to her left thigh without providing additional treatment for pyoderma gangrenosum (Figure 1F). A dramatic re-epithelization of all ulcers was observed at the covered site 1 week later (Figure 1G), while new lesions arose at uncovered sites, such as the buttock. This finding, along with clinical course and a notable improvement in the covered lesions, allowed us to reach a final diagnosis of self-injuring ulceration based on Munchausen syndrome, although we could not encounter how she made the presented ulcers even during hospitalization. Currently, further severe exacerbation is prevented owing to deep and cautious care of mental status by a well-contactable psychiatrist.
Munchausen syndrome was first proposed as an adaptive disorder in 1951,1 and such patients sometimes self-induce factitious injuries as a way of complaining or garnering attention from medical staff by reporting a plausible and dramatic history of illness.2 The patients also tend to visit several hospitals, feigning spectacular illnesses without receiving any visible benefit and lack of insight. Aside from the cutaneous type shown in the present case, the associated disorders include acute stomach symptom type, bleeding type, neural type, heart type, respiratory type, and foreign substance type.3 Twenty cases of patients with Munchausen syndrome mutilating their own skin, such as by injecting foreign objects and cutting themselves with a knife, have been reported.4 Numerous scratched ulcers with a symmetrical distribution were noted in the present case. Cutaneous self-injury arose on patients with Munchausen syndrome is difficult to cure, as most patients generally lack an illness and seldom consent to treatment.5 When encountering similar cases with factitious ulceration of the skin, a thorough understanding of the patient's psychiatric condition and a cordial consultation to present illness rather than physical medication might lead to disease stability.
ACKNOWLEDGMENT
None.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest. Dr. Manabu Fujimoto is Editor in Chief for the Journal of Cutaneous Immunology and Allergy. Management of the peer review process, and all editorial decision making, for this article was undertaken by an associate editor.
DECLARATION SECTION
Approval of the research protocol: No human participant was involved in this study.
Informed Consent: N/A.
Registry and the Registration No. of the study/trial: N/A.
Animal Studies: N/A.