A case of Stevens–Johnson syndrome-like eruption suggesting clinical importance of body temperature and serum levels of receptor-interacting kinase 3
Abstract
The present case is distinguished from Stevens–Johnson syndrome in that no elevation of serum receptor-interacting kinase 3, low level of serum granulysin, and the rather good general status, including no fever-up and rapid response to treatment.
Dear Editor,
An 80-year-old woman presented to our department with eruptions on her face, trunk, and extremities. Multiple erosions were found in the oral cavity and on the lips and vulva, but no hyperemia was evident on the conjunctiva of the eyeballs or eyelids (Figure 1A, B). Extensive diffuse erythema was present on the trunk and extremities. Multiple fused erosions and erythema were found in the middle of the back, inside the upper right arm, and on both knees. Nikolsky phenomenon was found even in areas without erosion, with total excoriation extending to 9% of the body surface area (Figure 1C, D). The first symptom observed was an oral lesion that had emerged within half a day after starting levofloxacin, acetaminophen, and ciprofloxacin for the treatment of a urinary infection. Administration of these drugs was subsequently discontinued. Two days after emergence of the first symptom, the patient visited our department. Methylprednisolone was administered at 1000 mg/day for 3 consecutive days, followed by oral prednisolone at 40 mg/day. All symptoms resolved within 3 weeks, and prednisolone was stopped 4 weeks after starting. The patient did not exhibit any fever during the entire clinical course. Histopathological findings included severe interface dermatitis with densely distributed necrotic keratinocytes and vacuolar alterations in the basal layer (Figure 1E), resulting in partial epidermal necrosis and subepidermal bullae with mild pigment incontinence (Figure 1F). Direct immunofluorescence revealed no evidence of autoimmune bullous disease. There was no medical history of drug eruptions. Drug-induced lymphocyte stimulation testing yielded positive results for levofloxacin (stimulation index [SI]: 2.5) and acetaminophen (SI: 2.1) and a negative result for ciprofloxacin, although these results alone could not determine a causative drug.
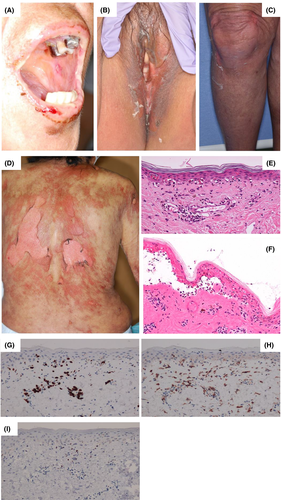
The present cutaneous and oral findings were consistent with Stevens–Johnson syndrome (SJS). However, the lack of fever throughout the clinical course was inconsistent with SJS criteria.1 In addition to the rather good general status and rapid response to treatment, the short duration (i.e., half a day) was also inconsistent with SJS.2 Further analyses using serum collected at the first visit to our department revealed the following. The low serum level of granulysin (2.5 ng/ml) was inconsistent with SJS.3 Serum galectin-7 level was 29.2 ng/ml, which was rather high for a so-called “non-severe adverse drug eruption.”4 Serum receptor-interacting kinase 3 (RIP3) level was below the limit of detection, which might not have been compatible with SJS.5 The dense distribution of epidermal necrotic keratinocytes accompanying mild lymphocytic infiltration (Figure 1G, H), including Foxp3-positive cells in the upper dermis (Figure 1I), favored SJS.2
Collectively, the present case exhibited a rather good general status and rapid response to treatment considering the clinical and histological findings, which were supported by the serum levels of biomarkers described above and that suggest pathogenesis of non-SJS/TEN. Serum levels of RIP3 have especially been reported to correlate with not only severity of SJS/TEN but also body temperature.5 Lack of fever throughout the clinical course in the present case might suggest the clinical importance of checking the body temperature for predicting clinical course.
DECLARATION SECTION
Approval of the research protocol: N/A.
Informed Consent: N/A.
Registry and the Registration No. of the study/trial: N/A.
Animal Studies: N/A.
CONFLICT OF INTEREST
The authors declare no conflicts of interest. Dr. Riichiro Abe is a member of the Journal of Cutaneous Immunology and Allergy Editorial Board. Management of the peer review process, and all editorial decision-making, for this article was undertaken by Editor in Chief.