The lack of association between different LDL-C levels and oxidized LDL in patients with type 2 diabetes
Abstract
Background
High concentrations of low-density lipoprotein cholesterol (LDL-C) have been a known risk factor for cardiovascular diseases. Also, the role of oxidized LDL (ox-LDL) in forming atherosclerosis plaque has been proven. However, it has not yet been proven that atherogenic LDL-C by-products like ox-LDL will decrease by keeping the LDL levels at the desired level. This study aimed to examine the relationship between LDL-C and ox-LDL in different LDL-C values in patients with type 2 diabetes (T2D).
Methods
In this cross-sectional study, 347 patients with T2D who received statins were enrolled. LDL-C values were defined into four groups as LDL-C < 55 mg/dL, 55 mg/dL ≤ to <70 mg/dL, 70 mg/dL ≤ to <100 mg/dL and LDL-C ≥ 100 mg/dL. Total cholesterol, triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and ox-LDL were studied in the four defined groups.
Results
Ox-LDL levels were not different among the four groups (p = 0.30). In addition, LDL-C and ox-LDL levels had no significant correlation (r = 0.480, p = 0.376). Additionally, based on this study analysis, ox-LDL levels were significantly correlated with TG levels (r = 0.119, p < 0.05) and TG/HDL ratio (r = 0.390, p < 0.01).
Conclusions
It is concluded that ox-LDL levels were not associated with different LDL-C level categories from <55 mg/dL to >100 mg/dL in patients with T2D. However, the revealed association of ox-LDL with TG level and TG/HDL ratio may be considered in the clinic.
Key points
-
The relationship between oxidized low-density lipoprotein (ox-LDL) and chronic diseases such as atherosclerosis and cancer has been proven previously, however, guidelines target low-density lipoprotein cholesterol (LDL-C) levels in lipid profiles for therapeutic purposes. Therefore, it is important to examine the changes in ox-LDL levels while reducing LDL-C levels.
-
By lowering LDL-C levels with statin treatment, no change in ox-LDL levels was found. However, ox-LDL levels had an association with triglyceride (TG) levels and TG/high-density lipoprotein (HDL) ratio.
1 INTRODUCTION
Atherosclerotic cardiovascular disease is the main cause of morbidity and mortality in patients with diabetes.1 Additionally, cardiovascular disease deaths are two to six times more common than in individuals without diabetes.2 Low-density lipoprotein cholesterol (LDL-C) is a modifiable risk factor for cardiovascular disease, and maintaining serum LDL-C at lower levels is a major concern in managing dyslipidemia in patients with diabetes.3, 4 However, in the Fourier trial, the reduction in cardiovascular events was less than expected, despite lowering LDL-C concentrations below the current targeted levels.5
About 30 years ago, the hypothesis that oxidized LDL (ox-LDL) is necessary for atherosclerosis was developed after observing that macrophages do not transform into foam cells by the uptake of LDL-C, conversely, the abnormal accumulation of lipids occurs due to the uptake of ox-LDL via scavenger receptors.6, 7
LDL-C particles are likely to damage by oxidation. The oxidation of native LDL-C occurs in three stages, including the lag phase, the proliferation phase, and the decomposition stage, which lead to the formation of new epitopes. These epitopes prevent LDL-C from binding to LDL-C receptors on macrophages.8 This alteration of native LDL-C shifts the identification and absorption of the lipoprotein to scavenger receptors from the LDL-C receptors expressed on macrophages and other vascular cells.9
Cholesterol accumulation due to the uptake of ox-LDL by macrophages converts macrophages to foam cells and promotes the development of atherosclerotic plaque.10 Ox-LDL is an independent predictor of endothelial dysfunction, with prothrombotic, pro-inflammatory, and pro-apoptotic functions in patients with diabetes.11, 12 Guidelines for lipid management in patients with diabetes are mainly focused on controlling LDL-C, total cholesterol, high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG) for cardiovascular risk reduction.13-16
It is not clear yet that maintaining serum LDL-C at an optimal level is appropriate to reduce atherogenic LDL-C derivatives such as ox-LDL. It would be interesting to evaluate how the ox-LDL levels change in different levels of LDL-C in patients with type 2 diabetes (T2D) in our routine practice. In this study, we investigated the ox-LDL levels among the categorized level of LDL-C in patients with T2D.
2 METHODS
A total of 347 patients with T2D were studied in this cross-sectional analysis based on the consecutive sampling who were referred to the outpatient diabetes clinic of Vali-Asr hospital, affiliated with Tehran University of Medical Sciences. The research was carried out according to the principles of the Declaration of Helsinki. The ethical committee of the National Institutes for Medical Research Development (NIMAD) approved the study with the registered number of IR. NIMAD. REC.1399.314.
This study was conducted in a large tertiary referral center. The studied participants were mainly homogenous, middle to high school education, middle-class; most had insurance and access to health care facilities and had usual physical activity. Diabetes was diagnosed according to the criteria of the American Diabetes Association. Inclusion criteria were patients with T2D on a moderate-intensity statin (atorvastatin 20 mg daily).
Exclusion criteria were age lower than 18 years, smoking, pregnancy, TG level > 400 mg/dL, end-stage renal disease, glomerulonephritis, congestive heart failure, cancer, use of antioxidants, hormone replacement therapy, and hospital admission in the recent 3 months.
Patient characteristics, including age, sex, weight, height, history of hypertension, duration of diabetes, history of coronary artery diseases (CAD), and history of antidiabetic medications, were recorded. CAD was defined as a coronary artery bypass graft, percutaneous coronary intervention, acute coronary syndrome, or myocardial infarction. Systolic and diastolic blood pressure measurements were performed in the sitting position after 10 min of resting with a standard sphygmomanometer.
We measured weight with a portable digital scaling device with an accuracy of 0.1 kg without shoes with minimally clothed participants. We measured height using a tape measure with the standard method. The body mass index (BMI) (kg/m2) was calculated by the Quetelet formula, defined as the weight (kg) divided by the squared height (m2). Pulse pressure was obtained by subtracting systolic blood pressure from diastolic blood pressure. The estimated glomerular filtration rate (eGFR) was calculated by the Cackroftgult formula in each participant. A urine albumin excretion rate of more than 30 mg over 24 h was defined as albuminuria. Urine albumin concentrations were measured by an immunoturbidimetric commercial kit (Randox).
We collected blood samples after 12 h of fasting, then centrifuged them, and kept them at −70°C until analysis. Laboratory measurements, including fasting blood sugar (FBS) using enzymatic calorimetric methods, total cholesterol, TG, HDL-C, and LDL-C with enzymatic methods, and hemoglobin A1c using high-performance liquid chromatography were measured for all participants. Based on LDL-C category defined as LDL-C < 55 mg/dL, 55 ≤ LDL-C to <70 mg/dL, 70 ≤ LDL-C to <100 mg/dL, and LDL-C ≥ 100 mg/dL, patients were divided into four groups. A commercially available sandwich enzyme-linked immunometric assay (Cayman) was used for measuring ox-LDL levels. The inter- and intra-assay coefficient of variation for the assay varied between 3.4% and 6.4%.
2.1 Statistical analysis
Statistical software IBM SPSS version 24.0 (IBM Corp.) was used for statistical analysis. Data were presented as mean ± standard deviation for continuous variables and number (percentage) for categorical variables. One-way analysis of variances (ANOVA) and the χ² test were used as appropriate for between-group comparisons. Also, the Spearman test was performed to evaluate the correlation of serum levels of ox-LDL with other lipid markers, including HDL-C, LDL-C, TG, and Total Cholesterol. Statistical significance was defined as a p < 0.05.
3 RESULTS
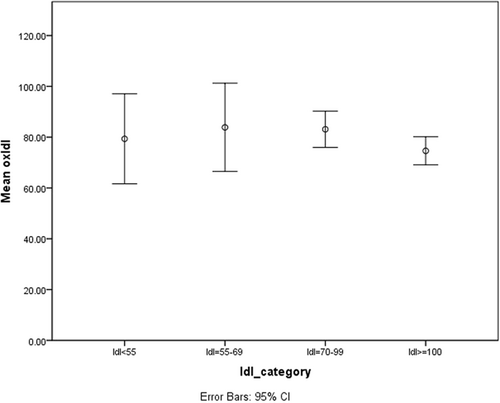
After applying exclusion criteria, 26 patients were excluded due to malignancy, end-stage renal disease, and recent hospitalization, and 347 patients with T2D were enrolled in this cross-sectional study. The mean age of the participants was 55.93 ± 10.29 years, and 57% were female. After division based on the LDL-C level, 26 participants enrolled in the group with LDL-C < 55 mg/dL, 34 participants entered the group with 55 mg/dL ≤ to <70 mg/dL, 145 participants joined the group with 70 mg/dL ≤ to <100 mg/dL, and 142 participants formed the highest LDL-C group (LDL-C ≥ 100 mg/dL). After determining each group's minimum, maximum, and average values of ox-LDL, a comparison chart was depicted (Figure 1).
The groups had no significant differences concerning age, gender, weight, height, BMI, eGFR, blood pressure (systolic and diastolic), pulse pressure, history of hypertension, duration of diabetes, and cardiovascular diseases (p > 0.05) (Table 1).
| Characteristics | LDL < 55 mg/dL, n = 26 | LDL 55 ≤ to < 70 mg/dL, n = 34 | LDL 70 ≤ to < 100 mg/dL, n = 145 | LDL ≥ 100 mg/dL, n = 142 | p Value |
|---|---|---|---|---|---|
| Age (years) | 55.9 ± 10.0 | 58.5 ± 9.2 | 56.1 ± 9.9 | 55.4 ± 10.8 | 0.46 |
| Female/male | 14/12 (54/46) | 17/17 (50/50) | 87/58 (60/40) | 76/66 (54/46) | 0.60 |
| Weight (kg) | 72.92 ± 11.07 | 68.89 ± 11.40 | 73.04 ± 14.81 | 72.32 ± 12.26 | 0.43 |
| Height (cm) | 162.86 ± 11.39 | 163.75 ± 10.79 | 163.34 ± 9.61 | 163.38 ± 8.59 | 0.99 |
| BMI | 27.70 ± 5.31 | 25.40 ± 3.89 | 26.97 ± 5.49 | 26.81 ± 4.55 | 0.56 |
| eGFR (cc/min) | 82.65 ± 31.66 | 63.23 ± 19.48 | 75.16 ± 21.569 | 69.34 ± 23.89 | 0.09 |
| SBP (mmHg) | 139.21 ± 19.82 | 130.66 ± 21.52 | 129.23 ± 16.60 | 133.20 ± 19.18 | 0.56 |
| DBP (mmHg) | 84.34 ± 11.43 | 77.20 ± 12.43 | 80.37 ± 10.27 | 82.73 ± 11.26 | 0.87 |
| Pulse pressure (mmHg) | 54.86 ± 13.77 | 53.45 ± 15.16 | 58.43 ± 97.25 | 50.47 ± 13.61 | 0.05 |
| DM duration (month) | 128.22 ± 66.80 | 121 ± 119.16 | 115.57 ± 74.28 | 107.47 ± 92.45 | 0.79 |
| History of HTN (%) | 62.5 | 58.3 | 38.8 | 50.0 | 0.23 |
| CAD history | 1 (3.8) | 1 (2.9) | 5 (3.4) | 4 (2.8) | 0.99 |
| Statin use | 100% | 100% | 100% | 100% | |
| DM drug | |||||
| OAD | 18 (70) | 22 (65) | 118 (81) | 130 (91) | <0.01 |
| Insulin | 7 (27) | 3 (9) | 21 (15) | 5 (4) | |
| Insulin + OAD | 1 (3) | 9 (26) | 6 (4) | 7 (5) |
- Note: Data are presented as mean ± SD or n (%).
- Abbreviations: BMI, body mass index; CAD, coronary artery disease; DBP, diastolic blood pressure; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; HTN, hypertension; LDL, low-density lipoprotein; OAD, oral agent drug; SBP, systolic blood pressure.
Among all four groups, there was no significant difference in HbA1c, FBS, and the presence of albuminuria (p > 0.05) (Table 2).
| Characteristics | LDL < 55 mg/dL, n = 26 | LDL 55 ≤ to < 70 mg/dL, n = 34 | LDL 70 ≤ to < 100 mg/dL, n = 145 | LDL ≥ 100 mg/dL, n = 142 | p Value |
|---|---|---|---|---|---|
| HbA1c | 8.21 ± 1.83 | 8.20 ± 1.89 | 8.44 ± 2.02 | 7.97 ± 1.70 | 0.22 |
| FBS (mg/dL) | 183.50 ± 77.20 | 190.67 ± 82.62 | 179.63 ± 51.66 | 174.57 ± 64.73 | 0.56 |
| TG (mg/dL) | 237.46 ± 87.35 | 186.29 ± 93.88 | 185.20 ± 72.54 | 187.42 ± 112.86 | 0.06 |
| Chol (mg/dL) | 183.57 ± 58.40 | 157.47 ± 41.71 | 182.93 ± 44.88 | 210.92 ± 41.57 | <0.01 |
| LDL-C (mg/dL) | 38.07 ± 13.13 | 62.82 ± 3.98 | 85.01 ± 8.70 | 121.92 ± 17.09 | <0.01 |
| HDL-C (mg/dL) | 40.65 ± 31.10 | 34.82 ± 9.93 | 38.33 ± 10.79 | 40.99 ± 10.74 | 0.06 |
| TG/HDL | 7.68 ± 3.89 | 6.07 ± 3.77 | 5.33 ± 2.80* | 4.82 ± 3.37* | <0.01 |
| ox-LDL (U/L) | 79.35 ± 43.78 | 83.86 ± 49.79 | 83.10 ± 43.30 | 74.61 ± 33.31 | 0.30 |
| Albuminuria | 6 (23) | 7 (20.5) | 40 (27.5) | 34 (23.9) | 0.44 |
- Note: Data are presented as mean ± SD or n (%).
- Abbreviations: Chol, cholesterol; FBS, fasting blood sugar; HbA1c, hemoglobin A1c; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; ox-LDL, oxidized low-density lipoprotein; TG, triglyceride.
- * p ≤ 0.05 versus LDL < 55 mg/dL.
Also, among lipid profile markers, including TG, total cholesterol, and HDL-C, only total cholesterol revealed a significant difference between groups (p < 0.01).
The mean ox-LDL and LDL-C levels among patients with diabetes were 78.6 ± 39.8 U/L and 94.4 ± 29.1 mg/dL, respectively. Also, the mean of ox-LDL levels and LDL levels in ANOVA analysis had no significant difference (p > 0.05).
The present study utilized ANOVA test (F = 6.290) to compare the TG/HDL ratio in different categories of LDL-C, and the results were added to Table 2. The analysis revealed that only groups with LDL-C ≥ 100 mg/dL and 70 mg/dL ≤ to <100 mg/dL showed significant differences in ox-LDL levels compared to the group with LDL-C < 55 mg/dL, while no other significant differences were observed between groups. Furthermore, a multivariable multinomial logistic regression was conducted to assess the confounding effect of TG/HDL on the absence of ox-LDL association with LDL-C categories. The findings indicated that after adjusting for TG/HDL ratio, the ox-LDL relation with LDL-C categories remained unchanged (p > 0.05).
The correlation of ox-LDL with other lipid profile parameters, including LDL-C, HDL-C, total cholesterol, TG, and TG/HDL was investigated among all participants. The results revealed that ox-LDL is significantly correlated with TG (r = 0.119, p < 0.05) and TG/HDL (p < 0.01); there was no significant correlation between ox-LDL and LDL-C (p = 0.376) (Table 3).
| Lipid profiles | Correlation coefficient to ox-LDL (r) | p Value |
|---|---|---|
| LDL-C | 0.48 | 0.376 |
| HDL-C | 1.02 | 0.057 |
| TG | 0.119 | <0.05 |
| Total Cholesterol | 0.093 | 0.082 |
| TG/HDL | 0.390 | <0.01 |
- Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; ox-LDL, oxidized low-density lipoprotein; TG, triglyceride.
To enhance the robustness of our analysis, we merged the initial two groups and performed an ANOVA test (F = 1.733) examination on three distinct LDL-C level categories (LDL-C < 70 mg/dL, 70 mg/dL ≤ to <100 mg/dL, and LDL-C ≥ 100 mg/dL) to evaluate the association of ox-LDL and LDL-C. The outcomes verified our earlier findings, demonstrating that there is no substantial difference in ox-LDL levels among the three categories of LDL-C in patients with T2D.
Furthermore, we executed a multivariable multinomial logistic regression to evaluate the confounding effect of TG/HDL on the absence of association between ox-LDL and LDL-C categories which remained unchanged (p > 0.05).
4 DISCUSSION
In the present study, we evaluated the levels of ox-LDL in four groups with different LDL-C levels in patients with T2D who were taking an equal dosage of statin treatment. This study revealed that LDL-C levels are not associated with ox-LDL levels in patients with T2D. However, this study showed that ox-LDL levels had a positive and significant correlation with serum TG levels and TG/HDL ratio in patients with T2D.
Previously, the association between ox-LDL and T2D has been examined and it was concluded that prolonged hyperglycemia causes the overproduction of free radicals.17 Consequently, these free radicals attack the lipid molecules in a chain reaction manner, causing structural changes in lipid molecules.18 Banerjee et al. revealed that in an Indian age-matched population, ox-LDL concentrations were higher in patients with T2D than in normal individuals. However, LDL-C levels were not significantly different between the two groups, indicating that more LDL-C molecules will be oxidized in chronic hyperglycemia and insulin resistance state.19
Another harmful role of ox-LDL is its effect on the incidence of specific cancers, such as colon, breast, and bladder cancers, as evaluated in various studies.20, 21 Additionally, another study investigated the relationship between ox-LDL and the occurrence of endometrial cancer in patients with T2D. It indicated a positive association between this index and endometrial cancer in patients with T2D.22
In previous studies, the association between ox-LDL and atherosclerosis has been investigated, and it has been reported that the presence of ox-LDL is essential for atherosclerosis.23 After oxidation of LDL-C, macrophages swallow ox-LDL molecules by scavenger receptors and become foam cells due to the inability to digest these molecules. These cells are now out of their normal state and no longer have their previous capabilities. Eventually, they deposit in the walls of the arteries and gradually form atherosclerotic plaques.24 Different treatment protocols have always been tried to reduce LDL-C and cholesterol levels to limit cardiovascular complications. However, recent studies have proven the undeniable role of ox-LDL in the pathogenesis and occurrence of various complications.24, 25 According to these findings and this study's results, using statins alone may not be enough to prevent hyperlipidemia complications; it might be due to the lack of association between LDL-C and ox-LDL.
In the Fourier study, it was found that lowering LDL-C levels to an average of 30 mg/dL with Evolocumab in patients receiving statins reduced the risk of cardiovascular complications; however, this reduction seemed lower than expected, associated with a hazard ratio of 0.85.5 On the other hand, in an open letter by Hayward et al., different reasons have been stated against treating based on LDL-C targeting, including insufficient scientific evidence regarding targeting LDL-C levels for treatments and concerns regarding its safety.26 However, this letter did not grab enough attention.
Based on the present study's findings, we suggest that latent pathology might be attributed to ox-LDL and its effects. Thus, evaluating ox-LDL levels alongside LDL-C may help prevent complications related to high lipid levels in patients with T2D. However, more studies are needed to evaluate the beneficial effect of focusing on ox-LDL lowering alongside LDL levels on dyslipidemia complications in patients with T2D. For instance, due to the high prevalence of cardiovascular events in T2D patients, controlling ox-LDL levels, alongside LDL levels may be beneficial for cardiovascular risk reduction. This cross-sectional study cannot evaluate the causality of ox-LDL levels on cardiovascular events, however, providing basic evidence for future studies.
Holvoet et al. demonstrated an association between high TG/HDL fraction and serum ox-LDL levels even after LDL-C adjustment.27 Similarly, in this study, TG/HDL was significantly associated with ox-LDL (p < 0.05). The absence of any significant association between ox-LDL levels and LDL-C, even after various adjustments (including TG/HDL) in regression models, suggests that further investigation is necessary to identify biomarkers for estimating ox-LDL levels or using them as surrogate factors for ox-LDL in patients with T2D.
In a study of 2307 patients with T2D and CAD treated with statins, it was observed that many patients had elevated TG baseline levels. Finally, it was concluded that baseline TG levels were independently associated with adverse cardiovascular outcomes, and this association remained constant in different groups despite having low LDL-C levels.28 Similarly, the present study showed that among lipid markers, only TG correlates with ox-LDL levels among all measured lipid markers.
This study has several limitations. The study was designed as cross-sectional, which cannot explore the efficacy of statins on the ox-LDL levels. Although the number of participants in each LDL-C category was enough for statistical analysis, they were not equally divided between groups. Moreover, it should be noted that the findings of this study are applicable solely to individuals with T2D, and additional research involving the general population is warranted. Finally, the duration of diabetes varied among participants in this study.
In conclusion, in this cross-sectional study, we concluded that ox-LDL levels were not different in four LDL-C categories ranging from <55 mg/dL to >100 mg/dL in patients with T2D. This study revealed an association of ox-LDL with TG and TG/HDL. Accordingly, assessing TG level along with LDL-C as a low-cost and widely available lab test may be helpful in routine practice for estimating ox-LDL and its related complications in patients with T2D. According to this study's findings, more observational studies are needed to further investigate the association between the level of ox-LDL and LDL-C in patients of T2D treated with statins.
AUTHOR CONTRIBUTIONS
Data collection and manuscript writing: Soghra Rabizadeh, Seyed Arsalan Seyedi, and Seyed Ali Nabipoorashrafi. Study design and data analysis: Soghra Rabizadeh and Armin Rajab. Manuscript editing and tables creation: Seyed Arsalan Seyedi and Seyed Ali Nabipoorashrafi. Validation and review: Soghra Rabizadeh, Maryamossadat Omidvar Siahkalmahalleh, Fatemeh Mohammadi, and Amirhossein Yadegar. Quality control: Manouchehr Nakhjavani and Alireza Esteghamati. All authors agreed on the final version of the manuscript.
ACKNOWLEDGMENTS
Research reported in this publication was supported by Elite Researcher Grants Committee under award number 996168 from the National Institutes for Medical Research Development (NIMAD), Tehran, Iran.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
ETHICS STATEMENT
The research was carried out according to the principles of the Declaration of Helsinki. The ethical committee of the National Institutes for Medical Research Development (NIMAD) approved the study with the registered number of IR. NIMAD. REC.1399.314. Informed consent for participation and publication was obtained from all individual participants included in the study.
Open Research
DATA AVAILABILITY STATEMENT
This study's data and excel worksheets are available upon request to the corresponding author through e-mail.