Surgical management of huge paratesticular rhabdomyosarcoma in a 20-year-old male: Case report and literature review
Key Clinical Message
Early diagnosis and aggressive treatment of testicular rhabdomyosarcomas including surgery and chemotherapy significantly reduce local recurrence and improve survival rates in young adults with metastases. Adjuvant chemotherapy is highly recommended to enhances prognosis and survival outcomes.
1 INTRODUCTION
Rhabdomyosarcoma (RMS) is a malignant tumor of mesenchymal origin thought to arise from cells committed to a skeletal muscle lineage. Typically, RMS presents as a large, painless, palpable mass (>5 cm) at diagnosis.1 CT scans of the thoraco-abdomino-pelvic region and technetium-99 m diphosphonate bone scans are recommended as part of the radiological evaluation to detect lymph nodes and distant metastases.2 Sites that appear abnormal on bone scans should be investigated further as warranted.1 Testicular ultrasound imaging typically reveals a solid mass, though distinguishing between benign and malignant tumors may sometimes be challenging.1
The procedure of choice- radical inguinal orchiectomy through inguinal approach with early cord ligation remains the essential procedure for histological diagnosis and constitutes the first step of treatment regardless of the stage of the disease. In adults with metastatic disease, prompt identification of testicular tumors, especially primary rhabdomyosarcomas, and aggressive surgical intervention combined with chemotherapy, are crucial for improving overall survival and reducing the incidence of local recurrence.3
Adjuvant chemotherapy is a highly recommended treatment that reduces local recurrence and improves the overall and disease-free survival rates of adult patients with metastases.4 The survival rate of patients with para-testicular rhabdomyosarcoma is approximately 50%.5 Radiotherapy is a complementary treatment to chemotherapy and surgery for eliminating residual foci and retroperitoneal lymph nodes.
We report the case of a 20-year-old male who presented with severe bilateral scrotal pain that developed over 2 weeks following previous scrotal surgery. Tumor marker investigations were negative. Surgical intervention included radical orchiectomy and retroperitoneal lymph node dissection. Histological examination of the surgical specimen confirmed paratesticular rhabdomyosarcoma. Three sessions of adjuvant chemotherapy were initiated, and the patient had a good outcome, with no signs of metastasis or residual foci within 9 months of follow-up.
2 CASE HISTORY
We present the case of a 20-year-old male who initially presented with severe bilateral scrotal pain. He was seen by a clinician at a peripheral facility, diagnosed with varicocele, and underwent bilateral varicocelectomy. The patient progressed well for 2 weeks post-surgery until he noticed gradual, painless bilateral scrotal swelling that progressively increased over time. The swelling began as a right hemi-scrotal swelling extending to the right groin, eventually involving the entire scrotum after 2 months. The patient had no history of lower urinary tract symptoms or hematuria, nor any history of chest pain, difficulty in breathing, hemoptysis, or bone pain.
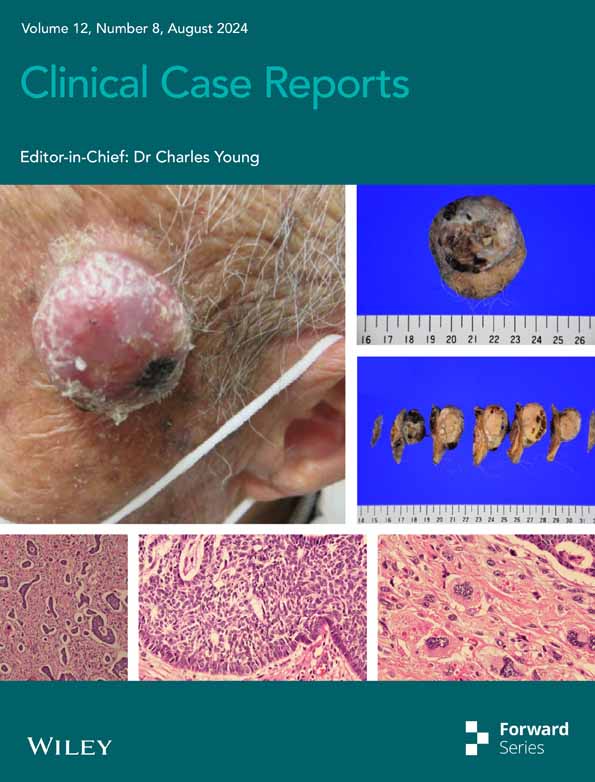
Abdominal examination revealed a normal abdominal contour and a soft abdomen that moved with respiration, with no evidence of organomegaly. Genital examination showed a hugely swollen, hard, engorged right hemi-scrotum and a spherical swelling on the left hemi-scrotum (Figure 1). Additionally, there was a protruded grade 4 right inguinal lymph node extending towards the deep inguinal ring, with normal findings on digital rectal examination.

3 INVESTIGATIONS AND TREATMENT
The initial blood work-up showed a normal complete blood count with a slight increase in platelet count to 425 × 109/L, and normal renal and liver function tests. Testicular tumor markers were within normal limits: α-fetoprotein level was 4.34 ng/mL, β-hCG concentration was 1.20 mIU/mL, testosterone level was 15.62 nmol/L, and LDH was 21 U/L. Metastatic work-ups including chest x-ray and contrast-enhanced CT of the chest revealed no evidence of metastases (Figure 2).

Contrast-enhanced abdomino-pelvic CT demonstrated para-aortic and para-caval lymphadenopathies with a heterogeneously enhancing testicular mass extending into the right inguinal region, measuring approximately 18.5 cm × 10 cm (Figure 3), consistent with testicular malignancy.

After thorough examinations and investigations, the patient underwent open radical orchiectomy and retroperitoneal lymph node dissection (RPLND-II), which included bilateral lymph node dissection above the renal arteries and below the inferior mesenteric artery. Through a combined midline and right inguino-scrotal incision, a vascular clamp across the cord was placed at the internal inguinal ring to prevent tumor cell spillage. Intraoperatively, extensive matted lymph nodes along the right gonadal vessel were found, spanning from pelvic lymph nodes, common iliac nodes, to interaortocaval and para-aortic nodes abutting the inferior vena cava and abdominal aorta, with encasement to the right mid ureter sparing the distal portion (Figure 4A,B).

The Cattell-Braash maneuver (right medial visceral rotation) facilitated exposure of retroperitoneal zones I and II. Dissection began with mobilization of the hepatic flexure followed by incision along the white line of Toldt. Avascular fusion between small bowel mesentery and posterior peritoneum was incised, enabling medial mobilization of the right colon and entire small bowel. Retroperitoneal lymph node dissection extended laterally from the right ureter, medially to the anterior aspect of the infrarenal abdominal aorta, and caudally to the bifurcation of the right common iliac artery, with renal vessels encompassed within the margins bilaterally in the cephalad direction (Figure 5). Resection of tumor encasement at the mid-ureter was performed, followed by ventral and distal spatulation of the ureter with DJ stent insertion.

Radical inguinal orchiectomy with high ligation of the spermatic cord 1–2 cm inside the internal ring was successfully performed (Figure 6). Haemostasis was perfectly achieved, and the wound was closed. The operation duration was 5 h and 21 min. Sperm retrieval was unsuccessful due to limited resources. Scrotal and abdominal drains were placed, and the patient underwent 48 h of ICU monitoring before transfer to the general ward.

4 RESULTS AND CONCLUSION
Following surgery, urine output was 1.5 mL/kg/h. Histological immunohistochemistry confirmed paratesticular rhabdomyosarcoma (Figure 7A–D). Adjuvant chemotherapy, consisting of vincristine, actinomycin D, and cyclophosphamide, was initiated with three sessions starting 1 month post-surgery. The patient remained recurrence-free during the 9-month follow-up.

5 DISCUSSION
Rhabdomyosarcoma (RMS) is a highly aggressive tumor and the most common soft tissue sarcoma in children and adolescents, with an annual incidence of 4–7 cases per million children aged 15–20 years.1 The etiology of pure primary testicular rhabdomyosarcoma remains unknown6 and is exceptionally rare, with only a few cases reported in the literature.4 RMS most frequently occurs in the head, neck, and genitourinary tract, with the genitourinary system commonly affected in locations such as the bladder and paratesticular organs.
Histologically, rhabdomyosarcoma (RMS) exhibits several variants classified under the international RMS classification: embryonal, botryoidal (a variation of embryonal), alveolar (including its solid variant), pleomorphic, and subtypes such as fusocellular and sclerosing pseudovascular. Alveolar rhabdomyosarcoma is particularly aggressive, characterized by rapid progression and frequent early metastases, resulting in higher mortality rates compared to embryonal rhabdomyosarcoma.7 Rhabdomyosarcoma (RMS) is primarily sporadic, although associations with familial conditions such as Li-Fraumeni syndrome (LFS) and neurofibromatosis have been observed. LFS, characterized by germline mutations in the p53 tumor suppressor gene, manifests with early-onset breast carcinoma and adrenocortical carcinoma in adult relatives, alongside familial clustering of RMS and other soft-tissue sarcomas in children.8
Primary intratesticular rhabdomyosarcomas typically manifest as painless intrascrotal masses in adult patients. Multidisciplinary treatment approaches may enhance good prognosis.9 In rhabdomyosarcoma, tumor markers such as alpha-fetoprotein, beta-human chorionic gonadotropin, and carcinoembryonic antigen are usually within normal limits, consistent with our patient's findings. Lymph node involvement is frequently observed at the time of diagnosis in rhabdomyosarcomas.
Macroscopic, microscopic, and immunohistochemical studies constitute the gold standard for diagnosing rhabdomyosarcoma and distinguishing between intratesticular, paratesticular, or spermatic variants.1, 5 Muscle-specific markers such as anti-desmin, actin, and myoglobin antibodies are employed in these studies. Myoglobin, known for its sensitivity, is present in differentiated rhabdomyoblasts but may test negative in poorly differentiated rhabdomyosarcomas. Sarcomeric actin is specific to well-differentiated rhabdomyoblasts and has been observed in leiomyosarcomas on rare occasions. Immunostains for nuclear proteins like myogenin and MyoD1, members of the transcription factor family, are both sensitive and specific for identifying rhabdomyosarcomas.10, 11
Surgery, chemotherapy, and radiation therapy constitute the primary treatment modalities for rhabdomyosarcoma (RMS). Radical orchiectomy is essential for complete tumor resection in all patients. In adults with testicular cancer, retroperitoneal lymphadenectomy is recommended due to the higher risk of retroperitoneal disease in this population. Preoperative imaging studies are crucial for assessing disease extent, even in cases with clinically disease-free lymph nodes.12
There is ongoing debate regarding the role of retroperitoneal lymph node dissection (RPLND) in the precise staging and initial treatment of non-metastatic rhabdomyosarcomas, especially in cases where radiological examinations show no evidence of positive lymph nodes. However, in situations where nodes continue to enlarge despite chemotherapy, RPLND has been suggested to aid in tumor debulking and prevent lymph node regrowth.2 Preoperative imaging (CT, MRI) and tumor staging are crucial in determining the appropriateness of RPLND. In clinical stage I–II patients without retroperitoneal lymph node metastases, retroperitoneal radiation therapy may be used instead of RPLND.
For cases involving metastasis, local recurrence, unresectable tumors, or residual disease (microscopic or macroscopic), particularly in unfavorable histology types like alveolar rhabdomyosarcoma, radiotherapy may be indicated.6 Systemic chemotherapy plays a pivotal role in eradicating both gross and micrometastatic disease and has been evaluated extensively in collaborative trials such as the Intergroup Rhabdomyosarcoma Study Group (IRSG), contributing to the development of combined modality therapy.13
Radiation therapy is essential in the treatment of rhabdomyosarcoma, particularly in anatomically challenging locations such as the head, neck, or pelvis where complete surgical resection may be difficult. Historical guidelines recommended high doses ranging from 5500 to 6000 cGy for primary tumor site management.2, 4, 14 However, evolving intergroup studies have revised these recommendations, suggesting that local control can often be achieved with doses of 4000–4500 cGy for microscopic residual disease, while doses between 4500 and 5000 cGy may be necessary for larger tumors or cases with extensive residual disease.1
Chemotherapy should be routinely administered since rhabdomyosarcoma is chemosensitive. With the advent of adjuvant and neoadjuvant therapy, individuals with localized disease now have a 60% higher chance of survival. Treatment regimens for rhabdomyosarcomas continue to be based on agents with proven efficacy in the management of RMS, such as vincristine (V), actinomycin D (A), doxorubicin (Dox), cyclophosphamide (C), ifosfamide (I), and etoposide (E).1 Currently, VAC and IVA regimens remain the cornerstone of treatment for RMS.15 However, when these regimens are applied to adult-onset patients, the administration of high-dose vincristine (maximal dose 2 mg/body) is essential.4 Consequently, vincristine doses are often relatively reduced (low relative dose intensity), impacting the chemotherapy's efficacy in adults with rhabdomyosarcoma and leading to a notably poor prognosis in these cases. In randomized trials including patients with clinical group III or IV cancer, melphalan and cisplatin were assessed for their potential application in combination chemotherapy for patients with locally widespread or metastatic disease; however, they did not enhance prognosis when compared with complementary therapies.16 For combined chemotherapy, VAC has been the gold standard in treating the majority of RMS cases. This case underscores the importance of early diagnosis, comprehensive surgical intervention, and adjuvant therapy in achieving favorable outcomes for paratesticular rhabdomyosarcoma.
AUTHOR CONTRIBUTIONS
Charles John Nhungo: Conceptualization; investigation; writing – original draft; writing – review and editing. Naomi Herbert Mtafu: Conceptualization; investigation; supervision. Joachim Kulwa Mhaya: Conceptualization; formal analysis; investigation. Fransia Arda Mushi: Writing – review and editing. Gabriel Mtaturu: Writing – review and editing. Advera Isaac Ngaiza: Data curation; formal analysis; investigation. Ally Hamis Mwanga: Writing – review and editing. Charles A. Mkony: Writing – original draft; writing – review and editing.
ACKNOWLEDGMENTS
We would like to thank the whole surgical urological team for the total support of our patient recovery.
FUNDING INFORMATION
There was no funding for this article.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
ETHICS STATEMENT
This case report study was exempt from ethical approval at our institution, as this paper reports a single case that emerged during normal surgical practice.
CONSENT
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
DISCLOSURE
This report has been published in accord with CARE criteria.
Open Research
DATA AVAILABILITY STATEMENT
This is not applicable to this article because this is a case report.