A Rare Case of Nitroglycerin Resistant Coronary Arterial Vasospasm During Coronary Artery Bypass Surgery
ABSTRACT
Background
Coronary artery vasospasm following coronary artery bypass grafting (CABG) is a rare but potentially life-threatening complication that can lead to myocardial ischemia, arrhythmias, and cardiogenic shock. Nitroglycerin-resistant vasospasm, particularly involving the left main coronary artery (LMCA), poses significant diagnostic and therapeutic challenges.
Case Presentation
We report the case of a 47-year-old female with a history of hypertension, hyperlipidemia, and ADHD on dextroamphetamine-amphetamine, who presented with chest pain and was found to have a suspected severe LMCA lesion. Coronary angiography revealed a 95% LMCA stenosis that was unresponsive to intracoronary nitroglycerin, raising concern for catheter-induced vasospasm versus true stenosis. The patient underwent urgent CABG. Intraoperatively and postoperatively, she experienced recurrent, diffuse coronary vasospasm refractory to nitroglycerin, necessitating multiple interventions including mechanical circulatory support with intra-aortic balloon pump and percutaneous ventricular assist device. Coronary angiography confirmed severe diffuse coronary and peripheral vasospasm. The patient was managed with intravenous vasodilators, vasopressors, and supportive care, and eventually recovered with restoration of cardiac function and discharge to cardiac rehabilitation.
Discussion
This case underscores the difficulty in differentiating vasospasm from true atherosclerotic disease in the LMCA, the potential for nitroglycerin resistance, and the risk of severe complications during CABG. The use of adjunctive imaging modalities, vasodilators beyond nitroglycerin, and early mechanical circulatory support may be critical in managing such complex cases.
Conclusion
Nitroglycerin-resistant coronary vasospasm, especially in the LMCA, can mimic fixed stenosis and lead to inappropriate surgical intervention and life-threatening complications. A multidisciplinary, imaging-guided approach is essential for accurate diagnosis and optimal management.
1 Introduction
Persistent graft or native coronary vasospasm in the postoperative period is a rare but potentially fatal complication of coronary artery bypass graft (CABG) with high morbidity and mortality [1]. This condition can lead to significant myocardial ischemia, hemodynamic instability, and even cardiogenic shock. A spasm can develop not only in the internal mammary artery but also occurs more frequently in the right gastroepiploic and radial arteries since they tend to have greater muscular components and less endothelial nitric oxide synthase expression [2]. Hence, the left internal mammary artery (LIMA) is preferred over other arteries [3]. Severe LIMA spasms can precipitate angina, acute hypotension, ST-segment elevation myocardial infarction (STEMI), and ventricular fibrillation. The diagnosis is typically confirmed through coronary angiography, which reveals diffuse or focal spasms of the coronary arteries or grafts. Management of severe post-CABG vasospasm includes the administration of vasodilators such as nitroglycerin and calcium channel blockers directly into the coronary arteries. In cases of refractory spasm and cardiogenic shock, mechanical support with intra-aortic balloon pump (IABP), Percutaneous Ventricular Assist Device (PVAD), or extracorporeal membrane oxygenation (ECMO) may be necessary to stabilize the patient and restore adequate coronary perfusion. No consensus exists in terms of appropriate management. We present a case of severe coronary vasospasm during CABG refractory to intracoronary nitroglycerin therapy.
2 Patient Presentation
A 47-year-old female with a medical history of hypertension, hyperlipidemia, and former tobacco use presented to an outside hospital with complaints of cardiac chest pain associated with shortness of breath. The symptoms commenced 12 h before presentation and were partially relieved by sublingual nitroglycerin; however, the patient required eight doses for symptom control. Her home medications included oral diltiazem (240 mg daily), isosorbide mononitrate (30 mg daily) for anginal chest pain, and dextroamphetamine–amphetamine (20 mg daily) for attention-deficit hyperactivity disorder (ADHD).
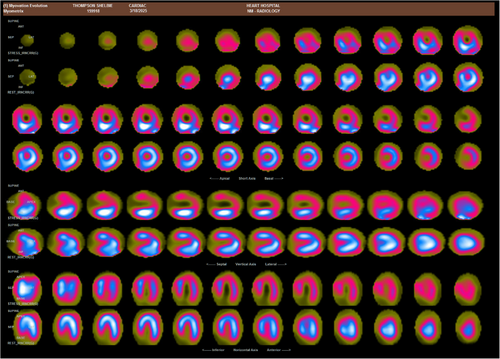
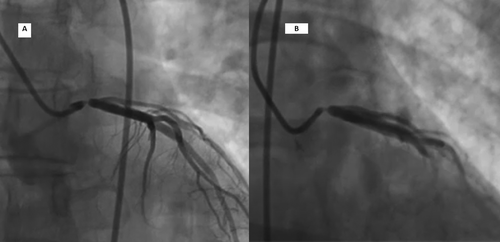
Upon presentation, she was hemodynamically stable, afebrile, normotensive, with a heart rate of 76 beats per minute. Initial laboratory tests revealed troponin I levels of 0.037 and 0.023 ng/mL, with a subsequent measurement below 0.020 ng/mL. Electrocardiography (EKG) demonstrated sinus tachycardia without ischemic changes. A nuclear cardiac stress test revealed high risk stress test with large anterior, septal, and lateral ischemia (Figure 1). A transthoracic echocardiogram showed left ventricular ejection fraction of 65%, and no wall motion abnormalities. The patient subsequently underwent an elective coronary angiogram, which revealed 95% stenosis vs Catheter tip associated vasospasm of the left main coronary artery (LMCA) that did not respond to intracoronary nitroglycerin (Figure 2). Of note, no other coronary vasodilators were given, no intracoronary imaging was performed, and no Coronary Computed Tomography Angiography (CCTA) was ordered to confirm atherosclerotic versus vasospastic nature of the stenosis. No significant disease was noted in the right coronary artery (RCA), left anterior descending artery (LAD), left circumflex artery (LCx), or LIMA. The right iliac and common femoral arteries were normal. Given the findings, she was transferred to our facility for CABG.
The patient underwent CABG under general anesthesia, receiving a LIMA graft to the mid LAD and a venous graft to the obtuse marginal artery. She was successfully weaned from cardiopulmonary bypass (CPB) on dobutamine. Intraoperative transesophageal echocardiography (TEE) demonstrated no wall motion abnormalities. However, during wound closure, she developed premature ventricular contractions (PVCs), followed by ST-segment elevation and hypotension requiring epinephrine administration and cardiac massage. The ST-segment changes improved with blood pressure stabilization; however, TEE revealed anterior wall hypokinesia, raising concerns for LIMA graft vasospasm. The patient was re-heparinized, re-cannulated, placed back on CPB, and started on IV nitroglycerin infusion. The LIMA graft to the LAD was ligated and replaced with a venous graft. An IABP was inserted via the right common femoral artery access, and the patient was weaned from CPB with both medical and mechanical circulatory support, along with nitroglycerin infusion. Following intervention, echocardiography and EKG findings normalized.
During transport from the operating room (OR) bed, the patient developed ventricular tachycardia cardiac arrest requiring chest compressions and epinephrine administration. At that moment, there was concern about a diffuse coronary artery spasm. After blood pressure stabilization, the IABP was removed and replaced with a Percutaneous Ventricular Assist Device (PVAD/Impella). Additionally, norepinephrine and epinephrine infusions were started for circulatory support to maintain perfusing systemic pressures, while nitroglycerin and diltiazem infusions were used to treat coronary vasospasm.
TEE showed global hypokinesia with reduced contractility compared to baseline. Emergent coronary angiography demonstrated severe diffuse coronary vasospasm in all coronary arteries with resultant occlusion of the saphenous venous graft to the obtuse marginal artery at the distal anastomosis, and a patent saphenous graft to the LAD (Figures 3 and 4). Significant peripheral vasoconstriction was also noted on femoral access angiography with severe spasm of the superficial femoral and profunda femoris arteries.
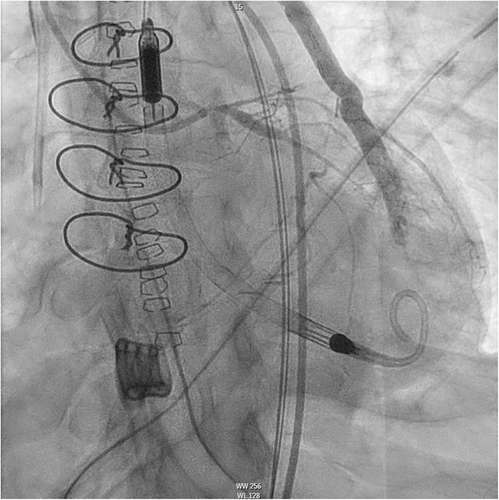
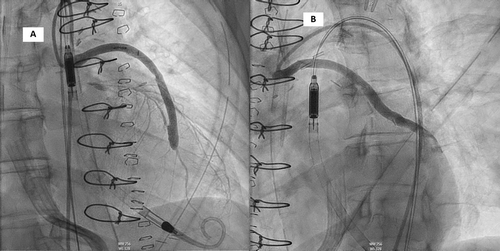
The patient was transferred to the cardiac intensive care unit (ICU) intubated, sedated, on mechanical circulatory support with Abiomed Impella CP device for left ventricular offloading and to improve coronary perfusion pressures, along with medical circulatory support through norepinephrine, epinephrine, vasopressin, and milrinone infusions. Additionally, diltiazem and nitroglycerin infusions were maintained to treat the diffuse, resistant coronary artery vasospasm.
The postoperative period was complicated by cardiogenic shock, and acute kidney injury She also developed ventilator-associated pneumonia, and new-onset atrial fibrillation. She was managed with above support measures, continuous renal replacement therapy (CRRT), broad-spectrum antibiotics, and amiodarone infusion, respectively. Nitroglycerin was successfully weaned off by POD 3. Impella support was gradually weaned off and ultimately removed on POD 6. The remaining vasoactive medications were gradually tapered, and the patient was successfully extubated on POD 9. Renal function showed progressive improvement, allowing discontinuation of CRRT by POD 10, with restoration of normal urine output and kidney function.
The patient eventually converted to sinus rhythm, leading to discontinuation of amiodarone therapy. She was subsequently discharged to a cardiac rehabilitation program. Her discharge medications included dual antiplatelet therapy with aspirin and clopidogrel, as well as diltiazem and isosorbide mononitrate for continued cardiovascular management.
3 Discussion
Revascularization with CABG is the gold-standard management (Class 1 recommendation) in patients with LMCA stenosis, associated with treatment-resistant anginal symptoms [4]. Using autologous arteries as bypass grafts has been proven to provide superior outcomes when compared to venous grafts. In the arterial graft group, the use of LIMA to graft the diseased LAD has become the standard of practice in CABG because LIMA is generally free of atherosclerosis and has high patency rates as grafts [3]. In addition, there are also differences in responses between the LIMA and the native coronary artery to vasoconstrictors [5].
Coronary artery spasm before CPB during cardiac surgery was reported by MacAlpin et al. in 1973 [6], and the first case of coronary artery spasm developed in the postoperative period of CPB was reported in 1980 by Pichard et al. [7]. This entity can often be unrecognized in the setting of cardiovascular collapse with disastrous results such an infarction, ventricular arrhythmias, and death. Coronary spasm can involve just a segment of the vessel or a diffuse process. Clinically evident perioperative coronary artery spasm usually occurs within 24 h following the discontinuation of CPB, but lethal spams have been reported even 2 days after the surgery [8]. The estimated Perioperative spasm in bypass grafts and coronary arteries has been reported in 0.43% of all CABG surgeries, However, this may be an underestimate since they can be present without triggering severe hemodynamic implications, also nowadays in the setting of more advanced and standardized strict postop monitoring where mild spasms might be asymptomatic [9].
The exact pathophysiologic mechanisms behind the arterial graft spasms are not known. However, multiple factors might Interplay. For instance, vascular trauma secondary to coronary artery manipulation or cardioplegia infusion, platelet activation at the site of endothelial damage, high local concentrations of potassium, acid-based disorders, hypomagnesemia, and induced ischemia. In addition, increased intracellular calcium has been reported to be a contributor since it mediates fine and powerful regulation of the interaction between the myosin and the actin filaments that regulate cellular contraction. This mechanism probably accounts for the successful results obtained when calcium channel-blocking agents treat angina. Similarly, nitroglycerin may also provide epicardial coronary vasodilatation through a calcium-mediated mechanism [10]. Furthermore, a study published by Engelman reported four patients who experienced life-threatening coronary vasospasm following the withdrawal of calcium channel blocker at the time of coronary revascularization [11]. Withdrawal from preoperative intravenous nitroglycerin was reported as a potential cause of severe early post-CABG spasm [10]. Medication-induced coronary artery spasm—such as potentially in our patient—may be influenced by the treatment of ADHD with dextroamphetamine-amphetamine, perhaps contributing to the clinical presentation.
The clinical presentation of this entity is variable, and a low index of suspicion is mandatory to initiate prompt appropriate treatment. For instance, patients recently extubated might complain of back pain, diaphoresis, or respiratory distress with hypotension or ST changes in the ECG, on the other hand, in an intubated patient in the early post-operatory period the suspicious relies mostly on hemodynamic variables, and sometimes using TEE might provide additional early signs of ongoing graft spams such a new hypo or akinesia [12]. Therefore, in the context of suspicion of coronary vasospasm, urgent coronary angiography is crucial to confirm the diagnosis, identify the involved vessels, and guide treatment [13]. However, a clinical diagnosis might remain challenging, as in our case, the preoperative angiography does not clearly differentiate whether the LMCA occlusion is due to atherosclerotic coronary artery disease (CAD) or catheter-induced coronary vasospasm. The lesion's resistance to intracoronary nitroglycerin further complicates the assessment. Performing an intravascular imaging with intravascular ultrasound (IVUS) or optical coherence tomography (OCT) was likely unsafe given angiographically significant 90% left main stenosis, risking completely obliterating the blood flow in the left coronary tree with the intracoronary imaging catheters, that will eventually provoke acute coronary syndrome (ACS) and circulatory collapse. One potential approach for diagnosis could be the use of more potent vasodilator agents. Or perhaps, obtaining CCTA to establish atherosclerotic as opposed to vasospastic nature of the left main disease may have been appropriate before further evaluation of Aorto-Coronary Bypass surgical evaluation. In fact there was a report of two patients with confirmed LMCA catheter-induced vasospasm who were inappropriately referred to CABG, while coronary angiography later confirmed no LMCA stenosis [14]. The true incidence of catheter-induced coronary artery vasospasm remains uncertain. However, in a large retrospective analysis of 7295 coronary angiograms, Chang et al. reported 30 cases of catheter-induced LMCA vasospasm, yielding an incidence of approximately 0.41% [15, 16].
Since the cause of coronary spasm is not fully understood and may be multifactorial, treatment of this condition has been largely empirical and usually involves peripheral or intracoronary nitroglycerin, a-adrenergic receptor blockers, and calcium channel blockers along with hemodynamic support with IABP or percutaneous ventricular assisted device, and ECMO in severe cases complicated by cardiogenic shock. Conventional treatments to reverse acute hypotension due to ventricular dysfunction, such as vasopressors or inotropic catecholamine agents, can further worsen the magnitude of coronary vasospasm and lead to further decline in the patient's cardiovascular status. The use of calcium channel-blocking agents in the setting of hypotension with ventricular dysfunction might seem contra intuitive, however, if there is evidence of coronary artery spasm and other causes of hemodynamic decline are not evident, the use of diltiazem particularly with radial artery graft has been described and was shown to decrease the systemic vascular resistance, increase coronary flow, decrease myocardial oxygen consumption ultimately reducing myocardial ischemia [17]. The effectiveness of peripheral IV nitroglycerin has been shown not to be as effective as direct administration into the coronary arteries or graft [8, 18, 19]. If inotropic support is deemed necessary, the choice of an agent that does not cause coronary vasoconstriction (such as epinephrine) is recommended.
4 Conclusion
Nitroglycerin-resistant coronary artery vasospasm presents significant diagnostic and management challenges, particularly when involving the LMCA. Differentiating between true stenosis and transient spasm can be difficult, potentially leading to inappropriate referrals for CABG. Moreover, unrecognized vasospasm during CABG may result in catastrophic intraoperative outcomes. Advances in imaging-guided coronary angiography and the availability of post-operative mechanical circulatory support have improved the ability to diagnose and manage such cases. Nonetheless, optimal care requires a multidisciplinary approach to ensure accurate diagnosis and appropriate therapeutic decision-making.
Acknowledgments
Publication fees for this manuscript were supported by the Texas Tech Health Science Center.
Ethics Statement
The authors have nothing to report.
Consent
The patient has provided written informed consent for the publication of this case report.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data supporting this case report are available within the manuscript. Due to patient confidentiality and ethical considerations, additional data, including medical records and imaging, are not publicly available. Any further details may be provided upon reasonable request, subject to institutional and ethical approvals.




