Novel Techniques for Alcohol Septal Ablation in Hypertrophic Obstructive Cardiomyopathy With Complex Anatomy: A Case Series
ABSTRACT
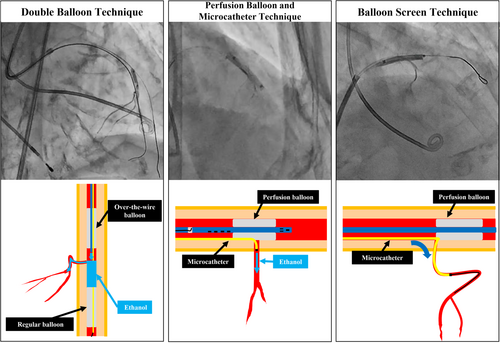
Alcohol septal ablation (ASA) is an established treatment for hypertrophic obstructive cardiomyopathy (HOCM). However, conventional techniques may be challenging in cases with complex septal branch anatomy, including hairpin curves, extremely small branches, and acute angle bifurcations. We present three innovative catheter techniques that expand the applicability of ASA in these challenging anatomical scenarios. The double balloon technique overcomes hairpin curves in the proximal septal branches, while the perfusion balloon and microcatheter technique enables ablation of extremely small branches. The balloon screen technique facilitates access to small branches at acute angles. These methods were successfully applied to three patients with medically refractory HOCM, resulting in a significant reduction in left ventricular outflow tract pressure gradients and an improvement in symptoms. These novel techniques provide potential solutions for anatomically challenging cases, expanding the indications for ASA and improving clinical outcomes for patients with HOCM.
1 Introduction
Alcohol septal ablation (ASA) is an established treatment option for drug-refractory hypertrophic obstructive cardiomyopathy (HOCM) [1-3]. The clinical application of this technique has been challenged by the more predictable and durable results of surgical myectomy or of the transcatheter septal scoring along midline endocardium (SESAME) technique [4] as well as by the introduction of anti-myosin inhibitors that offer a pharmacological alternative to all mechanical interventions. However, ASA has also found new applications in the prevention or treatment of left ventricular outflow obstruction after transcatheter mitral valve implantation. Preprocedural coronary angiography (CAG) is crucial for identifying target septal branches and assessing their anatomy, including origin, diameter, and course. Intraprocedural echocardiography is essential to confirm that the targeted septal branches adequately perfuse the intended myocardium. This imaging technique helps to evaluate the extent of myocardial ablation, detects any inadvertent effects on non-target areas, and determines if additional septal branches require ablation to achieve optimal results. Key elements of this procedure include: (1) effective ablation of the myocardium contributing to left ventricular outflow tract (LVOT) obstruction; (2) prevention of ethanol leakage into non-target vessels, especially the left anterior descending (LAD) artery, to avoid unintended acute myocardial infarction; and (3) sparing of non-target myocardial regions. Mastery of these technical aspects is crucial for procedural success and avoidance of complications. However, conventional ASA techniques may be challenging or unfeasible in cases with extremely small septal branches or acute bifurcation angles, making it difficult or impossible to deliver over-the-wire (OTW) balloons or microcatheters. To address these anatomical challenges, we developed novel techniques to expand the indications for ASA to previously unsuitable cases. This report describes innovative approaches aimed at improving the safety and efficacy of ASA in complex anatomical scenarios.
1.1 Case Reports
Detailed case descriptions are provided as Online Supporting Information S1: Material.
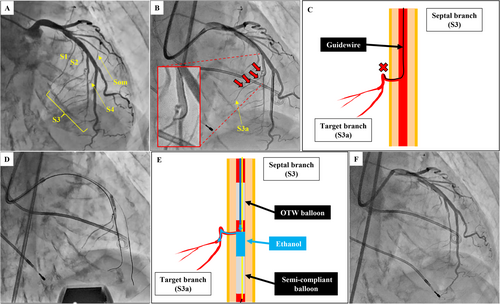
Case 1: Double Balloon Technique
A 76-year-old woman with drug-refractory HOCM (New York Heart Association [NYHA] functional class III) underwent ASA with an LVOT pressure gradient (PG) of 74 mmHg. Preprocedural CAG identified four target vessels: the second (S2), third (S3), and fourth (S4) septal branches and a septal branch originating from the second diagonal branch (Som) (Figure 1A). After the initial ethanol injection into S2, the proximal portion of S3 (S3a) was targeted (Figure 1B). The guidewire passage was challenging due to a hairpin curve in the proximal S3a (Figure 1C). To overcome this, we performed the double balloon technique: a 2.0 × 10 mm semi-compliant balloon catheter occluded the distal S3, while a 2.5 × 8 mm OTW balloon catheter occluded the proximal S3, effectively sandwiching the target vessel segment (Figure 1D,E, Supporting Information S1: Video 1). Ethanol was injected between the two balloons, achieving selective ablation. After additional ablations of S4 and Som, the final CAG showed successful ablations of all targeted vessels (Figure 1F). Post-procedural LVOT-PG decreased to 18 mmHg with sustained improvement at 1-year follow-up.
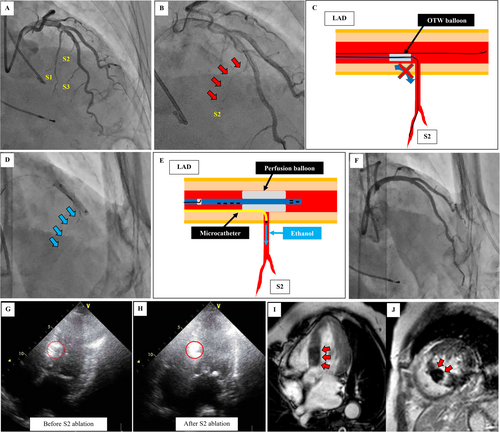
Case 2: Perfusion Balloon and Microcatheter Technique
A 76-year-old woman with NYHA functional class III HOCM (LVOT-PG 105 mmHg) underwent ASA. Preprocedural CAG identified the first septal branch (S1) and S3 as target vessels for ASA (Figure 2A). After the ablation of the two septal branches, transthoracic echocardiography (TTE) revealed a gap between the ablated areas. A small, string-like S2 branch was targeted (Figure 2B). Due to the small size of the branch, a microcatheter was used instead of an OTW balloon catheter (Figure 2C). To prevent ethanol leakage into the LAD, a perfusion balloon catheter (Ryusei; 3.0 × 20 mm; Kaneka Medix) was inflated in the LAD, covering the ostium of the S2 (Figure 2D,E, Supporting Information S1: Video 2). Ethanol was successfully injected without any leakage (Figure 2F). Post-procedural TTE confirmed the elimination of the previously unablated staining gap (Figure 2G,H). Cardiac magnetic resonance imaging confirmed thorough ablation of the target septum (Figure 2I,J). Post-procedural LVOT-PG decreased to 0 mmHg with sustained improvement at 1-year follow-up.
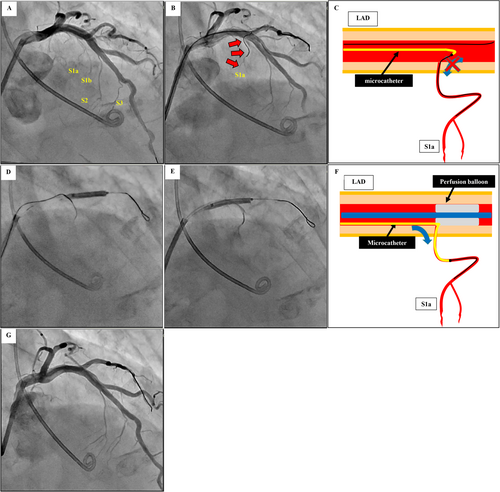
Case 3: Balloon Screen Technique
A 55-year-old man with drug-refractory HOCM (NYHA functional class III, LVOT-PG 62 mmHg) underwent ASA. Preprocedural CAG identified S1 bifurcating into S1a and S1b as target vessels (Figure 3A). The target S1a branch had an acute bifurcation angle that prevented insertion of OTW balloon catheter or microcatheter (Figure 3B,C). We performed the balloon screen technique, placing a perfusion balloon catheter (Ryusei; 3.0 × 20 mm; Kaneka Medix) in the LAD, with its proximal edge positioned at the ostium of S1 and inflating it at low pressure. The balloon acted as a supporting wall while anchoring the guidewire in S1a enabling microcatheter advancement (Figure 3D, Supporting Information S1: Video 3). Selective ethanol injection was successfully performed with an inflated perfusion balloon preventing ethanol leakage (Figure 3E,F). After S1b ablation, the target septal branch ablation was completed (Figure 3G). Post-procedural LVOT-PG improved to 6 mmHg with sustained improvement at 1-year follow-up.
2 Discussion
This case series demonstrates the potential efficacy of three novel ASA techniques in overcoming anatomical challenges that limit conventional approaches. These innovations build upon previous efforts to address the complex septal branch anatomy in ASA, offering solutions for patients who might otherwise be unsuitable candidates for this procedure.
The double balloon technique effectively addresses septal branches with extreme angulation, allowing precise ethanol delivery by occluding both the proximal and distal portions of the target vessel. This approach is especially valuable in cases where the proximal portion of the septal branch exhibits a hairpin curve, making conventional guidewire passage impossible. Kitamura et al. reported this technique as a method to block the distal portion of the target septal branch [5], thereby preventing unintended ethanol ablation of the right ventricle through collateral vessels originating from the target septal branch and draining into the right ventricle. Our modification focuses on navigating proximal hairpin curves, highlighting the versatility of this approach.
The perfusion balloon and microcatheter technique addresses a critical challenge in ASA: the treatment of extremely small septal branches. This approach utilizes a microcatheter for precise ethanol delivery and a perfusion balloon to prevent unintended leakage into the LAD. This approach facilitates targeted ablation of previously inaccessible septal myocardium, expanding the range of treatable septal branch anatomy.
The balloon screen technique has been widely used in various interventional scenarios, particularly for difficult bifurcation angles. However, our application in ASA for HOCM involves two significant adaptations. First, unlike traditional applications which primarily prevent device prolapse, we intentionally anchor the guidewire by positioning the proximal portion of the perfusion balloon at the S1 bifurcation. This creates a stable track specifically for microcatheter advancement through the challenging septal branch anatomy. Second, after successful microcatheter insertion, the perfusion balloon can be repositioned to cover the septal branch ostium, seamlessly transitioning to the perfusion balloon and microcatheter technique. This integration creates an efficient approach that progresses from vessel access to ethanol delivery, making the technique particularly valuable in ASA, as it not only solves the access challenge but directly facilitates the critical therapeutic step.
These novel techniques carry potential risks that warrant careful consideration. The double balloon technique necessitates careful manipulation of the two balloons, potentially increasing vascular injury risk. The perfusion balloon and microcatheter technique requires meticulous attention to prevent ethanol leakage. Low-pressure balloon inflation is essential to minimize the risk of coronary injury while excessively low pressure may increase the risk of ethanol leakage. Therefore, contrast test injections before ethanol administration are essential to ensure adequate vessel sealing. In our cases, we used a Ryusei perfusion balloon catheter, which has multiple small fenestrations in both the proximal and distal portions, allowing for distal coronary flow during inflation [6]. However, prolonged inflation of the Ryusei catheter may still induce myocardial ischemia. This technique can be further facilitated by the introduction of the Ringer perfusion balloon catheter (Teleflex) with its very large opening for distal perfusion and features that limit the risk of alcohol spilling into the proximal and distal portions of the balloon permeable to the bloodstream [7]. These factors must be carefully weighed against the potential benefits of the technique, with careful patient selection, and in centers with significant ASA experience. Intraprocedural imaging, particularly TTE, plays a critical role in ensuring adequate ablation and monitoring for complications. By implementing these safety measures, operators can strive to achieve effective septal branch isolation while minimizing the risk of myocardial injury.
3 Conclusion
The double balloon, perfusion balloon with microcatheter, and balloon screen techniques represent significant advancements in ASA for HOCM. These methods expand the applicability of this minimally invasive procedure to patients with challenging septal branch anatomy, who were previously considered unsuitable candidates. While these results are encouraging, it is imperative that these techniques be applied cautiously. This includes careful patient selection, detailed preprocedural planning with comprehensive angiographic and echocardiographic assessments, and performance in centers with significant ASA experience. Intraprocedural imaging, particularly TTE, plays a critical role in ensuring adequate ablation and monitoring for complications. As we continue to refine and evaluate these methods, they have the potential to significantly impact HOCM management (Central Illustration 1).
4 Learning Objectives
- 1.
This case series introduces three novel ASA techniques—the double balloon, perfusion balloon and microcatheter, and balloon screen techniques—to overcome anatomical challenges in HOCM.
- 2.
These novel techniques expand the applicability of ASA to cases with complex septal branch anatomy, including hairpin curves, extremely small branches, and acute angle bifurcations, which pose difficulties for conventional ASA.
- 3.
In three patients with drug-refractory HOCM, the application of these novel techniques resulted in a significant reduction in LVOT PGs and an improvement in symptoms.
- 4.
Cautious patient selection, detailed preprocedural planning with comprehensive angiographic and echocardiographic assessments, and performance in centers with significant ASA experience are crucial for the safe and effective implementation of these techniques.
Acknowledgments
The authors sincerely thank the staff of the Department of Cardiovascular Medicine, Nippon Medical School.
Ethics Statement
Ethical approval was not sought for this case report as the study involved the retrospective analysis of anonymized patient data according to the institutional guidelines for case reports. The patients provided written informed consent to publish their clinical details and images.
Consent
Written informed consent was obtained from all the patients.
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
The data that supports the findings of this study are available upon request from the corresponding author.




