Ten-year outcomes after percutaneous coronary intervention of in-stent restenosis in saphenous vein grafts
Abstract
Background
Only few data is available for long-term outcomes of patients being treated for in-stent restenosis (ISR) in saphenous vein grafts (SVG).
Aims
Thus, the aim of this observational, retrospective study was to close this lack of evidence.
Methods
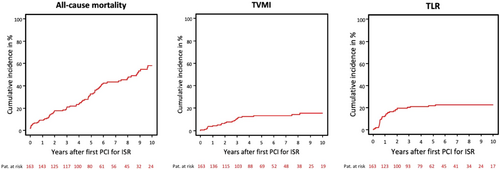
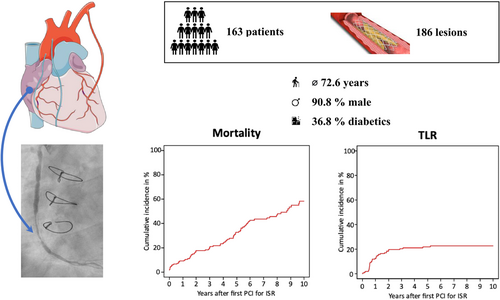
Between January 2007 and February 2021 a total of 163 patients with 186 ISR lesions located in SVG were treated at two large-volume centers in Munich, Germany. Endpoints of interest were all-cause mortality, target lesion revascularization (TLR) and target vessel myocardial infarction (TVMI). Furthermore, recurrent ISR were assessed. Outcomes are presented as Kaplan–Meier event rates.
Results
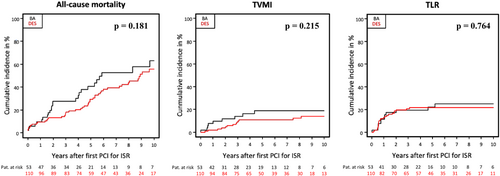
Mean age was 72.6 ± 8.6 years, 90.8% were male, 36.8% were diabetics and 42.3% presented an acute coronary syndrome. ISR were treated with DES in 64.0% and with balloon angioplasty (BA) in 36.0%. After 10 years, the rates for all-cause mortality, TVMI and TLR were 58.2%, 15.4%, and 22.6%, respectively. No statistically relevant differences were found between the types of treatment (DES or BA) regarding all-cause mortality (55.7% vs. 63.2%, p = 0.181), TVMI (13.8% vs. 18.6%, p = 0.215) and TLR (21.8% vs. 25.0%, p = 0.764). Median time between first and recurrent ISR was 270.8 days. Recurrent ISR were treated with DES in a comparable proportion as during first ISR (p = 0.075). Independent predictor of TLR is patient age (p = 0.034). The median follow-up duration was 5.1 years (75% CI 2.8; 8.5).
Conclusions
Clinical event rates after intervention of ISR located in SVG are high without statistically relevant differences regarding the type of treatment. However, further studies are needed.
Abbreviations
-
- BA
-
- balloon angioplasty
-
- CABG
-
- coronary artery bypass graft
-
- DCB
-
- drug-coated balloon
-
- DES
-
- drug-eluting stent
-
- ISR
-
- in-stent restenosis
-
- MI
-
- myocardial infarction
-
- NTVMI
-
- nontarget vessel myocardial infarction
-
- NTVR
-
- nontarget vessel revascularization
-
- PCI
-
- percutaneous coronary intervention
-
- POBA
-
- plain old balloon angioplasty
-
- ST
-
- stent thrombosis
-
- SVG
-
- saphenous vein graft
-
- TLR
-
- target lesion revascularization
-
- TVMI
-
- target vessel myocardial infarction
-
- TVR
-
- target vessel revascularization
1 INTRODUCTION
In-stent restenosis (ISR) represents the most common reason for treatment failure after interventional treatment of coronary artery stenosis.1, 2 The implementation of new generation drug-eluting stents (DES) diminished the risk of ISR in comparison to previous devices.3 However, still about every fifth patient develops ISR during long-term follow-up4 which is known to be associated with higher mortality rates.5
Approximately 6% of all percutaneous coronary interventions (PCI) affect saphenous vein grafts (SVG),6, 7 which are known to have a higher risk of restenosis8, 9 and cardiovascular events10-12 as compared to PCI of stenosis in native coronary arteries. Besides, SVG represents the most frequently used conduit in coronary artery bypass graft (CABG) surgery13 and approximately half of SVG occlude within 10 years after coronary artery bypass graft surgery,14, 15 which is explained by early acute thrombosis, intimal hyperplasia, vascular inflammation, and accelerated atherosclerosis.16 Taking these considerations into account, the treatment of ISR located in SVG represents a challenging interventional procedure.
According to current ESC guidelines new generation DES and drug-coated balloons (DCB) are listed as golden standard for the treatment of ISR.17 However, as most outcome data with currently available treatment strategies is preserved for ISR in native coronary arteries, there is still a lack of data concerning the optimal treatment strategy for ISR in SVG. The aim of this analysis is to close this gap of knowledge by providing further information for PCI of ISR in SVG.
2 METHODS
2.1 Study design and patient selection
The ISAR-DESIRE registry is an observational study of patients who underwent PCI for the treatment of ISR between January 2007 and February 2021 at the Deutsches Herzzentrum München, Munich, Germany and the 1. Med. Klinik, Klinikum rechts der Isar, Technical University, Munich, Germany. The present analysis focuses on ISR located in SVG.
2.2 Interventional procedure and medications
PCI of ISR was performed according to standard clinical practice. All patients were treated with either balloon angioplasty (BA) including DCB or implantation of DES. Patients treated with both, DES and BA, for the same ISR lesion were assigned to the DES group. The decision regarding the individual therapy strategy was determined by the treating physician. According to local standards, predilatation was recommended for all patients undergoing PCI for ISR, the use of scoring or debulking devices was left to the operators' discretion, as well as the decision to perform postdilatation after stenting. During the procedure, patients usually received 500 mg aspirin intravenously and body weight adjusted intraarterial or intravenous heparin or bivalirudin immediately after the decision to perform the intervention. After the intervention all patients received aspirin indefinitely and a P2Y12 inhibitor (clopidogrel, prasugrel, or ticagrelor) according to clinical presentation and recommendations at the time of PCI.
2.3 Data collection and quantitative coronary angiography analysis
Personnel of the clinical data management center (ISAResearch-Center) collected relevant data on source-documented hospital chart reviews. This data included information regarding clinical and lesion-related parameters at the time of initial and repetitive PCI for first and recurrent ISR. The required data for this study was entered into an anonymized study database. Angiographic and procedural parameters of interest included the type of intervention (BA vs. DES), balloon diameter and maximum balloon pressure, total stented length, and stent diameter as well as TIMI grade flow pre and post PCI.
2.4 Endpoints
Endpoints of interest regarding this analysis were survival after first PCI due to ISR in SVG, time to ISR recurrence, target lesion revascularization (TLR), target vessel myocardial infarction (TVMI), nontarget vessel revascularization (NTVR), nontarget vessel myocardial infarction (NTVMI), and stent thrombosis (ST). Target vessel revascularization (TVR) was defined as revascularization in the target vessel outside the target lesion. Event rates are presented as Kaplan–Meier 10-year event rates for all-cause mortality and cumulative 10-year incidences after accounting for the competing risk of death for the other endpoints. The definition of myocardial infarction (MI) used in this analysis was based on the Third Universal Definition of Myocardial Infarction.18 The definitions of ISR, ST, TLR, and NTVR used in this trial were adapted from the Academic Research Consortium.19, 20
2.5 Statistics
Baseline descriptive parameters are presented as mean ± standard deviation for continuous data and numbers with percentages for categorical data. Survival analyses were performed according to Kaplan–Meier method and the treatment of the first ISR was defined as time zero. Univariate analysis considering clinical and lesion-related variables was performed. Unadjusted hazard ratios and 95% confidence intervals were calculated with the use of Cox proportional models. We applied a multivariable linear model to identify the independent predictors of the total number of repeat TLR per patient. A 2-tailed p < 0.05 was considered statistically significant. Statistical software R (Version 4.0, R Foundation for Statistical Computing) was used for all analyses.
3 RESULTS
3.1 Baseline and procedural characteristics
A total of 163 patients underwent PCI due to ISR located in SVG. The mean age of this patient cohort was 72.6 ± 8.6 years and 90.8% were male. 36.8% suffered from diabetes, 98.2% from arterial hypertension and 84.7% from hypercholesterolemia. Nearly all patients (99.4%) presented with coronary multivessel disease and 58.9% had history of myocardial infarction. Most patients were admitted due to stable coronary artery disease (57.7%). Further clinical baseline characteristics are presented in Table 1.
| All patients (n = 163) | Patients treated with DES (n = 110) | Patients treated with DCB (n = 21) | Patients treated with POBA (n = 32) | p Value | |
|---|---|---|---|---|---|
| Age (in years) | 72.6 ± 8.6 | 71.7 ± 8.6 | 72.2 ± 7.8 | 75.8 ± 8.8 | 0.060 |
| Female sex | 15 (9.2) | 12 (10.9) | 1 (4.8) | 2 (6.3) | 0.770 |
| BMI (in kg/m2) | 27.7 ± 4.2 | 27.8 ± 4.0 | 29.5 ± 5.4 | 26.4 ± 3.5 | 0.026 |
| (n = 160) | (n = 108) | (n = 21) | (n = 31) | ||
| Diabetes mellitus | 60 (36.8) | 35 (31.8) | 13 (61.9) | 12 (37.5) | 0.032 |
|
34 (20.9) | 22 (20.0) | 6 (28.6) | 6 (18.8) | 0.612 |
| Arterial hypertension | 160 (98.2) | 108 (98.2) | 21 (100.0) | 31 (96.9) | 0.695 |
| Hypercholesterolemia | 138 (84.7) | 91 (82.7) | 18 (85.7) | 29 (90.6) | 0.601 |
| Current smoker | 13 (8.0) | 12 (10.9) | 1 (4.8) | 0 (0.0) | 0.093 |
| CAD | 0.247 | ||||
|
1 (0.6) | 0 (0.0) | 0 (0.0) | 1 (3.1) | |
|
2. (1.2) | 1 (0.9) | 0 (0.0) | 1 (3.1) | |
|
160 (98.2) | 99.1 (109) | 21 (100.0) | 30 (93.8) | |
| Multivessel disease | 162 (99.4) | 110 (100.0) | 21 (100.0) | 31 (96.9) | 0.325 |
| Ejection fraction (in %) | 50.3 ± 9.5 | 50.2 ± 9.7 | 47.9 ± 15.0 | 51.5 ± 7.2 | 0.666 |
| (n = 98) | (n = 67) | (n = 7) | (n = 24) | ||
| Clinical presentation | 0.020 | ||||
|
94 (57.7) | 60 (54.5) | 9 (42.9) | 25 (78.1) | |
|
31 (19.0) | 22 (20.0) | 8 (38.1) | 1 (3.1) | |
|
32 (19.6) | 24 (21.8) | 4 (19.0) | 4 (12.5) | |
|
6 (3.7) | 4 (3.6) | 0 (0.0) | 2 (6.3) | |
| History of MI | 96 (58.9) | 64 (58.2) | 12 (57.1) | 20 (62.5) | 0.895 |
- Note: Clinical baseline characteristics of 163 patients being treated for first ISR in SVG, either with DES, with DCB or with POBA. Data shown as means ± standard deviation or numbers (percentage).
- Abbreviations: BMI, body mass index; CAD, coronary artery disease; DCB, drug-coated balloon; DES, drug-eluting stent; MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; POBA, plain old balloon angioplasty; STEMI, ST-elevation myocardial infarction.
A total of 186 ISR lesions located in SVG were treated. ISR were treated with DES-implantation in 64.0% and with BA in 36.0%. In the BA group 35.8% (24/67 patients) were treated with a DCB. In the total cohort, median maximum balloon diameter was 3.5 mm (3.0 mm; 4.0 mm), median maximum balloon pressure was 16.0 atm (13.0; 18.0), median stented length was 25.0 mm (18.0; 38.0 mm) and median stent diameter was 3.5 mm (3.0 mm; 4.0 mm). Postinterventional 93.0% had TIMI grade flow 3. A summary of procedure-related characteristics is shown in Table 2.
| All lesions (n = 186) | Lesions treated with DES (n = 119) | Lesions treated with DCB (n = 24) | Lesions treated with POBA (n = 43) | p Value | |
|---|---|---|---|---|---|
| Total stented length (in mm) | 25.0 (18.0; 38.0) | 25.0 (18.0; 38.0) | - | - | - |
| Max. stent diameter (in mm) | 3.5 (3.0; 4.0) | 3.5 (3.0; 4.0) | - | - | - |
| Max. balloon diameter (in mm) | 3.5 (3.0; 4.0) | 3.5 (3.0; 4.0) | 3.5 (3.0; 4.0) | 3.5 (3.0; 4.0) | 0.001 |
| Max. balloon pressure (in atm) | 16.0 (13.0; 18.0) | 16.0 (14.0; 18.0) | 15.0 (13.0; 16.2) | 15.0 (12.2; 19.8) | 0.373 |
| Cutting balloon | 5 (2.7) | 2 (1.7) | 3 (12.5) | 0 (0.0) | 0.020 |
| Ostial lesion | 30 (16.6) | 21 (17.9) | 2 (8.3) | 7 (17.5) | 0.605 |
| TIMI grade flow pre PCI | 0.246 | ||||
|
18 (9.7) | 9 (7.6) | 1 (4.2) | 8 (19.0) | |
|
4 (2.2) | 4 (3.4) | 0 (0.0) | 0 (0.0) | |
|
20 (10.8) | 15 (12.6) | 1 (4.2) | 4 (9.5) | |
|
143 (77.3) | 91 (76.5) | 22 (91.7) | 30 (71.4) | |
| TIMI grade flow post PCI | 0.005 | ||||
|
4 (2.1) | 1 (0.8) | 0 (0.0) | 3 (7.1) | |
|
3 (1.6) | 0 (0.0) | 0 (0.0) | 3 (7.1) | |
|
6 (3.2) | 3 (2.5) | 0 (0.0) | 3 (7.1) | |
|
172 (93.0) | 115 (96.6) | 24 (100.0) | 33 (78.6) |
- Note: Procedural characteristics of 186 first ISR lesions in SVG, either being treated with DES, with DCB or with POBA. Data shown as numbers (percentage) or absolute numbers (95% confidence interval).
- Abbreviations: DCB, drug-coated balloon; DES, drug-eluting stent; PCI, percutaneous coronary intervention; POBA, plain old balloon angioplasty; TIMI, thrombolysis in myocardial infarction.
3.2 Clinical outcomes
The median follow-up duration was 5.1 years (75% CI 2.8; 8.5). Ten-year all-cause mortality rate after PCI of ISR in SVG was 58.2%, TVMI rate was 15.4% and TLR rate was 22.6% after 10 years (Figure 1). A total of 15.3% underwent TVR, 51.3% underwent NTVR and in 11.1% NTVMI occurred after 10 years. One ST was detected. An overview of the clinical outcomes is presented in Table 3. Outcomes according to the type of treatment (DES vs. BA) did not differ statistically significant: the 10-year rate for all-cause mortality was 55.7% versus 63.2% (p = 0.181), for TVMI 13.8% versus 18.6% (p = 0.215) and for TLR 21.8% versus 25.0% (p = 0.764) (Figure 2). The rates for NTVR (56.2% vs. 40.7%, p = 0.205), NTVMI (12.3% vs. 8.5%, p = 0.709), TVR (12.4% vs. 21.1%, p = 0.088) and ST (1.4% vs. 0.0%, p = 0.468) were comparable as well. Moreover, BA treated patients have been divided in DCB treated and plain old balloon angioplasty (POBA) treated patients based on an exploratory analysis to further illustrate clinical outcomes.
| Ten-year event rate of all patients (n = 163) | Ten-year event rate of DES treated patients (n = 110) | Ten-year event rate of BA treated patients (n = 53) | p Value (DES vs. BA) | Ten-year event rate of DCB treated patients (n = 21) | Ten-year event rate of POBA treated patients (n = 32) | |
|---|---|---|---|---|---|---|
| All-cause mortality | 71 (58.2) | 46 (55.7) | 25 (63.2) | 0.181 | 7 (53.7) | 18 (62.2) |
| TLR | 35 (22.6) | 23 (21.8) | 12 (25.0) | 0.764 | 5 (24.8) | 7 (22.4) |
| TVMI | 22 (15.4) | 13 (13.8) | 9 (18.6) | 0.215 | 6 (41.0) | 3 (9.6) |
| NTVMI | 16 (11.1) | 12 (12.3) | 4 (8.5) | 0.709 | 1 (5.3) | 3 (9.5) |
| TVR | 22 (15.3) | 12 (12.4) | 10 (21.1) | 0.088 | 5 (33.8) | 5 (16.0) |
| NTVR | 76 (51.3) | 56 (56.2) | 20 (40.7) | 0.205 | 11 (69.7) | 9 (28.6) |
| ST | 1 (1.0) | 1 (1.4) | 0 (0.0) | 0.469 | 0 (0.0) | 0 (0.0) |
- Note: Clinical outcomes in terms of 10-year event rates after treatment of first DES-ISR in SVG. Data shown as Kaplan–Meier event rates for all-cause mortality and cumulative incidences after accounting for the competing risk of death for the other outcomes. Data shown in numbers (percentage).
- Abbreviations: BA, balloon angioplasty; DCB, drug-coated balloon; DES, drug-eluting stent; NTVMI, nontarget vessel myocarial infarction; NTVR, nontarget vessel revascularization; POBA, plain old balloon angioplasty; ST, stent thrombosis; TLR, target lesion revascularization; TVMI, target vessel myocardial infarction; TVR, target vessel revascularization.
3.3 Predictors of TLR
In total, there were 332 repeat TLR, or 2.04 ± 1.78 repeat TLR per patients. In the multivariable model, the number of repeat TLR inversely correlated with patient's age (p = 0.034) (Table 4).
| p Value | Coefficient | |
|---|---|---|
| Age | 0.034 | −0.062 |
| Sex | 0.877 | −0.532 |
| BMI | 0.262 | −0.068 |
| Diabetes mellitus | 0.594 | −0.265 |
| Hypercholesterinemia | 0.593 | −0.318 |
| Current smoker | 0.753 | −0.425 |
| CAD | 0.917 | +0.782 |
| Clinical presentation | ||
|
0.516 | −0.405 |
|
0.231 | −1.058 |
|
0.979 | −0.193 |
| History of myocardial infarction | 0.842 | −0.085 |
| Max. balloon diameter | 0.783 | −0.084 |
| Restenosis morphology | ||
|
0.659 | −0.177 |
|
0.823 | +1.113 |
|
0.905 | −0.276 |
- Note: Parameters predicting TLR after treatment of first DES-ISR in SVG.
- Abbreviations: BMI, body mass index; CAD, coronary artery disease; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
3.4 Recurrent ISR
A total of 70 lesions (37.6%) were treated due to recurrent ISR at least twice, 30 lesions were treated with a third PCI, 21 lesions underwent a fourth PCI and 24 lesions underwent more than four PCIs. Median elapsed time between PCI of first SVG ISR and PCI of second SVG ISR was 348.4 days (Q1 198.3; Q3 729.8), between second and third PCI 203.1 days (Q1 195.3; Q3 642.9), between third and fourth PCI 315.3 days (Q1 159.0; Q3 528.4) and between later following PCIs it was 186.0 days (Q1 85.1; Q3 337.7). Median time between first and recurrent ISR was 270.8 days. The rates of DES-implantation for the second, third, fourth and later recurrent ISR were 57.7%, 43.3%, 52.4%, and 41.7%, respectively. Recurrent ISR were treated with DES in a comparable proportion as during first ISR (p = 0.075). Overall, a total of 129 patients had an angiographic follow-up (median time after last PCI of SVG-ISR: 682 days) and the rate of occluded SVGs was 15.5%.
4 DISCUSSION
- 1.
The 10-year all-cause mortality of patients undergoing PCI of DES-ISR in SVG is high (58.2%) and statistically comparable between patients treated with DES or BA.
- 2.
Patient age was found out to be an independent predictor of TLR.
- 3.
More than one-third of the lesions required a repeat PCI due to recurrent ISR (37.6%) and 15.5% of the previously treated SVG lesions were occluded during angiographic follow-up.
According to data from the PREVENT IV trial SVG failure rate is 25.4% at 1 year assessed by follow-up angiogram.21 As redo-CABG is associated with higher rates of peri- and postoperative complications than initial CABG surgery, PCI represents a reasonable therapeutic approach after CABG.22 Although PCI after CABG is frequently performed in native vessels, PCI of SVG becomes more common with longer time intervals from CABG.23 It is far well known that the treatment of SVG failure constitutes a challenging therapeutic procedure due to higher rates of periprocedural complications, mortality, MI and repeat revascularizations than PCI in native vessels.24 Furthermore, PCI of SVG is accompanied by high rates of restenosis,8, 9 an independent predictor of long-time survival.5 Because of low shear stress and a high thrombogenic state, SVG ISR develop faster than de novo lesions in SVG.25 However, elapsed time from stent implantation to ISR does not seem to differ between SVG and native vessel lesions,26 which implicates similar pathophysiological processes causing ISR in SVG and native vessels.25 Taking these considerations into account, ISR located in SVG constitute a clinically significant challenge in interventional cardiology.
In our study the 10-year all-cause mortality after PCI of ISR in SVG was 58.2% which is considerably higher than observed after PCI of native coronary arteries. For example, the 10-year mortality rate was 36.1% in the ISAR-TEST-5 trial, which evaluated patients being treated with DES for de novo lesions in native coronary vessels.27 However, median age of ISAR-TEST-5 patients was 67.8 years in comparison to 72.6 years in the underlying patient cohort. Moreover, 29.0% of ISAR-TEST-5 patients were diabetics, the rate of coronary artery multivessel disease was 83.7% and mean ejection fraction was between 52.4% and 52.6%.27 Baseline characteristics of the underlying cohort showed 36.8% to be diabetics, 99.4% to suffer from multivessel disease and a mean ejection fraction of 50.3%.27 Patients being treated for SVG lesions are commonly older and show an increased cardiovascular risk profile in comparison to patients being treated for native vessel lesions. Thus, the higher rates of mortality and major adverse cardiovascular events observed in this high-risk cohort are not unexpected.
During the 10-year observation period, the Kaplan-Maier TLR rate was 22.6%, which is comparable to PCI of native coronary arteries: in the ISAR-TEST-5 trial, the 10-year TLR rates were 21.4%.27 However, long-term data regarding TLR of ISR and especially those located in SVG are currently lacking. First long-term results for treatment of DES-ISR in native vessels were published by Kufner and colleagues who reported comparable TLR rates of 33.3% for ISR treatment with DCB and 24.2% for treatment with another DES implantation after 3 years, mainly driven by TLRs within the first year after treatment of restenosis. However, 3-year TLR rates after ISR treatment with BA were significantly higher (>50%) compared to DCB and DES.28 Furthermore, after a median follow-up of 825 days the event rates for major adverse cardiac and cerebrovascular events (55.6% vs. 45.0%, p < 0.001) and TVR (22.4% vs. 8.0%, p < 0.001) are significantly higher after PCI in ISR than in de novo lesions.29 In the multivariable model, the number of repeat TLR inversely correlated with patient's age; so, an older age predicted a reduced need for TLR. The impact of older age might be explained in two ways: first, by a more conservative approach in the treatment of ISR in elderly; second, the higher mortality in the elderly may limit the time window for reintervention in this age category.
In daily clinical practice, the question arises how to treat ISR located in SVG. In our study, no statistically relevant differences were found between patients treated with DES or BA. When comparing DCB versus POBA, a numerically higher rate of TVMI in the DCB-group was observed, but this finding should be taken with caution due to the limited number of patients in both groups. According to the DAEDALUS study treatment of ISR (mostly located in native coronary vessels) with DCB is less effective than treatment with DES in terms of TLR rate at 3-year follow-up.30 However, in this meta-analysis just about 1.5% of target lesions were localized in SVG, and the applicability of these data to the current collective is therefore very limited. This is consistent with previous data, where the use of DCB for treatment of ISR went along with higher numbers of TLR compared to the use of DES although it does not lead on to higher rates of MI during follow-up.31, 32
4.1 Limitations
The results of our analysis should be interpreted with caution as there are several limitations. First, it is an observational retrospective study and so subject to all limitations of this design. Thus, some information is not available for every patient, for example, exact cause of death or selected procedural characteristics of patients who were initially treated elsewhere. Furthermore, the median follow-up duration was 5.1 years (75% CI 2.8; 8.5). Because the study period in the underlying trial extended to 2021, only 67 of the patients who survived up to the last contact date were eligible for a 5-year follow-up. Nine of these 67 patients (13.6%) had incomplete 5-year follow-up. Second, the choice of PCI in case of SVG ISR was left to the operator's discretion and thus, a selection bias cannot be ruled out. Moreover, information regarding the decision making whether to treat the native vessel or the SVG are not available, especially in the case of recurrent ISR. Third, substantial advances in interventional treatment and antithrombotic therapy were made during the inclusion period. This may be a reason why DCB was used only in the minority of the patients. In addition, intravascular imaging has not been systematically applied. Fourth, the number of included patients with SVG ISR is small and the occurrence of rare events such as ST might be underreported. Fifth, the present analysis just considered DES-ISR in SVG and did not deal with DES-ISR in arterial bypass grafts. However, a minority of just approximately 2.5% of PCI in patients with prior CABG refers to arterial bypass grafts.23 Finally, there were numerically differences in DES- and BA-treated patients for several clinical outcomes such that even larger series need to be analyzed before firm conclusions can be made on the success rates of the two different treatment modalities.
5 CONCLUSIONS
Patients undergoing PCI of DES-ISR in SVG show high rates of clinical events during long-term follow-up, including a notable proportion of recurrent restenotic events. However, the type of treatment did not affect outcomes since event rates were statistically comparable with DES and BA. However, further randomized studies are required to assess the optimal treatment for DES-ISR in SVG (Central Illustration 1).
CONFLICTS OF INTEREST STATEMENT
C. K. has received a speaker fee from AstraZeneca (Speech for AstraZenecas “Summer Special” in 09/2022). S. K. reports lecture and consulting fees from AstraZeneca, Bristol-Myers Squibb, Translumina and Bently, not related to the current work. H. S. has received lecture fees from AstraZeneca, Bayer Vital, MSD Sharp & Dohme, Novartis, Servier, Sanofi-Aventis, Synlab, and Bristol-Myers Squibb, consulting fees from MSD Sharp & Dohme, Amgen, AstraZeneca, Boehringer Ingelheim, Daiichi-Sankyo and Servier and external funds from AstraZeneca, St. Jude and Boston Scientific. J. W. reports lecture fees from AstraZeneca, Translumina and Abbott Vascular and received Institutional Research Grant support from Abbott Vascular. The remaining authors declare no conflict of interest.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the ISAResearch-Center, Munich, Germany. Authors state no funding involved. The study was approved by the local ethics board of the Technical University Munich, Germany, and adheres to the Declaration of Helsinki.