SARS-CoV-2 and influenza viruses: Strategies to cope with coinfection and bioinformatics perspective
Abstract
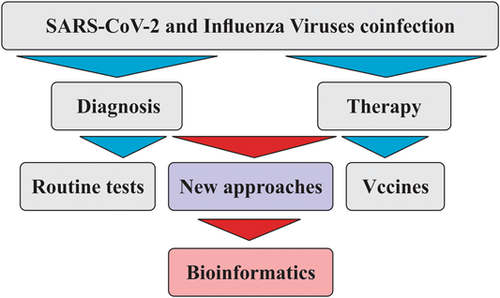
Almost a century after the devastating pandemic of the Spanish flu, humankind is facing the relatively comparable global outbreak of COVID-19. COVID-19 is an infectious disease caused by SARS-CoV-2 with an unprecedented transmission pattern. In the face of the recent repercussions of COVID-19, many have argued that the clinical experience with influenza through the last century may have tremendous implications in the containment of this newly emerged viral disease. During the last 2 years, from the emergence of COVID-19, tremendous advances have been made in diagnosing and treating coinfections. Several approved vaccines are available now for the primary prevention of COVID-19 and specific treatments exist to alleviate symptoms. The present review article aims to discuss the pathophysiology, diagnosis, and treatment of SARS-CoV-2 and influenza A virus coinfection while delivering a bioinformatics-based insight into this subject matter.
1 INTRODUCTION
A newly emerged menace to public health, coronavirus disease 2019, or COVID-19, was first reported in the Huanan South China Seafood Market located in Wuhan, China. Ever since the first report in the country of origin, COVID-19 has continued to pose a severe health issue in almost all parts of the world (Heidari Nia et al., 2022; Sheervalilou, Shirvaliloo, Sargazi, Bahari, et al., 2021; Sheervalilou, Shirvaliloo, Sargazi, Shirvalilou, et al., 2021; Sivasankarapillai et al., 2020). A seasonal disease of the respiratory tract, influenza was the eighth leading cause of mortality among Americans before the massive outbreak of COVID-19 (Jain et al., 2015). The recent 2019–2020 influenza outbreak had resulted in tens of millions of patients in the United States before the unwelcome reign of COVID-19 started (Singer, 2020). As of February 18, 2022, there have been 418,650,474 confirmed cases of COVID-19, including 5,856,224 deaths, in the world. As of February 14, 2022, a total of 10,279,668,555 doses of vaccines have been administered (https://covid19.who.int/).
The newly identified viral strain called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes significant morbidity and mortality as an impending consequence of acute respiratory distress syndrome (Sheervalilou et al., 2020; Sheervalilou, Shirvaliloo, Sargazi, Shirvalilou, et al., 2021). This is why we now live in a distinctly different world with a redefined lifestyle (Debby & David, 2020). In the absence of relevant information regarding the pathogenesis of SARS-CoV-2, the rational alternative was to turn to our previous experience with outbreaks such as SARS, MERS, and influenza. There were conclusive libraries of information particularly concerned with the pathogenesis of these causative agents (Debby & David, 2020; Y. Wang, Wang, et al., 2020). However, the overwhelmingly high fatality rate of COVID-19 urged the scientific society to learn about this new calamity as quickly as possible (Sheervalilou, Shirvaliloo, Sargazi, Bahari, et al., 2021; Y. Wang, Wang, et al., 2020).
To date, there has been officially approved specific medication for the treatment of COVID-19 as well as vaccines; hence, the need to comply with the tried-and-true methods such as self-isolation and prevention of infection. This is because developing novel therapeutic agents, or even repurposing the old ones, is a rather challenging task for clinicians. They first need to make an evident lab-based diagnosis of the disease due to the many similarities it shares with other viral infections (Zhu et al., 2020). It is well established that the primary intervention in the case of any contagious disease is immunization of individuals against the causative agents through vaccination (Azizi & Azizi, 2020). Several vaccines have been approved for emergency use against COVID-19 (Aruru et al., 2021), including vaccines developed by Pfizer and BioNTech. Nevertheless, researchers are still trying to design a more effective vaccine versus the SARS-CoV-2 36. Table 1 displays various vaccine platforms utilized versus CoVs (Anderson et al., 2020; Buchholz et al., 2004; H.-W. Chen et al., 2016; D. D., 2020; Graham et al., 2018; Hashemi et al., 2021; Jimenez-Guardeño et al., 2015; Kalita et al., 2020; T. W. Kim et al., 2004; D. Kim et al., 2020; J. Lu et al., 2020; Menachery et al., 2018; Spruth et al., 2006; Takashima et al., 2011; S.-F. Wang et al., 2014; Zakhartchouk et al., 2007; Zhang et al., 2020).
| Vaccine type | Virus | Vaccine target | Reference |
|---|---|---|---|
| Live-attenuated virus | Coronaviruses | All virus proteins | Graham et al. (2018); Menachery et al. (2018) |
| Inactivated virus | Coronaviruses | Whole structural protein of the virus | Jimenez-Guardeño et al. (2015); Spruth et al. (2006) |
| RNA-based vaccines | SARS-CoV-2 | Spike protein | Anderson et al. (2020) |
| Virus-like vaccines | Coronaviruses | N/A | H.-W. Chen et al. (2016); J. Lu et al. (2020) |
| DNA-based vaccines | Coronaviruses containing SARS-CoV-2 | S glycoprotein | T. W. Kim et al. (2004); S.-F. Wang et al. (2014); Zhang et al. (2020) |
| Protein-based vaccines | NVX-(COV2373)/respiratory syncytial virus | S glycoprotein and peptides | Kalita et al. (2020); Zakhartchouk et al. (2007) |
| Recombinant protein-based vaccines | Coronaviruses containing SARS-CoV-2 | All virus proteins: Spike protein, membrane protein nucleocapsid protein | Buchholz et al. (2004); D. D. (2020); E. Kim et al. (2020); Takashima et al. (2011) |
It is a pressing concern to find that many investigations focus on isolated infection with SARS-CoV-2 while overlooking instances of simultaneous infection with another pathogen or even pathogens. This is an important issue as coinfection with several pathogens may interfere with an accurate diagnosis of COVID-19 and result in discrepancies in the therapeutic window related to either one of the infections (Zhu et al., 2020). Before the SARS-CoV-2 outbreak, respiratory viral coinfections were reported in about 40% of patients with flu-like symptoms (Pinky & Dobrovolny, 2020). More recently, a meta-analysis concluded that nearly 3% of patients hospitalized with the diagnosis of COVID-19 were simultaneously infected with other respiratory pathogens, with influenza A being the secondary infection in most of the cases (Lansbury et al., 2020). As the more recent studies suggest, there has been a descending trend in the detection of coinfection in adults diagnosed with COVID-19 (Blasco et al., 2020; D. Kim et al., 2020; Nowak et al., 2020; Siordia, 2020; Xing et al., 2020). Still, the same statement cannot be made for pediatric patients with COVID-19, as they showed a 40% coinfection rate with another pathogen along SARS-CoV-2 in several investigations (Xia et al., 2020). It is unclear whether coinfection with another pathogen may result in unfavorable therapeutic outcomes in patients infected with SARS-CoV-2. According to two separate investigations, SARS-CoV-2/influenza coinfection did not result in worse clinical outcomes (Ding et al., 2020). Moreover, this condition decreased the mortality rate among patients. Interestingly, coinfection with influenza virus in COVID-19 patients might render them less vulnerable to morbidities associated with COVID-19, and hence, a better prognosis overall (G. Wang, Xie, et al., 2020). On average, more than 90% of patients with COVID-19 are simultaneously infected with other bacteria, viruses, and/or fungi, according to an investigation. While the number of cases with SARS-CoV-2/influenza coinfection might not appear as staggering, the relatively high prevalence of seasonal influenza can increase the risk of coinfection in patients with COVID-19 (Zhu et al., 2020). Though, the present theory needs to be further evaluated by prospective investigations, as in some instances, coinfection might very well worsen patients' clinical condition (Khorramdelazad et al., 2021).
It would be sensible to elucidate how SARS-CoV-2 might interact with other pathogens, especially respiratory agents, in severe cases of coinfection (Pinky & Dobrovolny, 2020). A pathogen of interest, the influenza virus, commonly results in signs and symptoms that may not be readily distinguished from that of COVID-19 in all instances. Hence, our current lack of knowledge could beget a wave of coinfection, rendering us incapable of containing the situation (Azekawa et al., 2020). In terms of clinical reasoning, SARS-CoV-2 is a beguiling pathogen that most deceptively mimics the influenza virus in numerous regards, including clinical manifestations and transmission mode as well. Ergo, coinfection by both viruses might not be as far-fetched as expected (Cuadrado-Payán et al., 2020) (Table 2).
| Difference | Flu | COVID-19 | References |
|---|---|---|---|
| Virus characteristics | Segmented genome with negative-sense ss-RNA chain | Unsegmented genome with positive-sense ss-RNA chain | B. Singh et al. (2020); Konala et al. (2020); Balla et al. (2020) |
| Transmission | Contact/Respiratory droplets | Contact/Respiratory droplets | |
| Asymptomatic or symptomatic | Asymptomatic Patients due to herd immunity | Patients with symptom developments within 2 days of infection | |
| Signs and symptoms | Fever, headache, myalgia, malaise, cough, sore throat, nasal discharge, gastrointestinal illness (vomiting and diarrhea in 10%–20% infected children) | Fever, cough, dyspnea, nasal discharge, myalgias, common diarrhea, and smell or taste disorders, conjunctivitis/dermatologic manifestations, maculopapular, urticarial, vesicular eruptions, transient livedo reticularis | |
| Incubation period | 1–4 days (average 2 days) | Within 14 days after exposure (most cases 4–5 days after exposure) | |
| Viral shedding | 5–10 days | Up to 14 days or longer | |
| Severity of illness | Mild to moderate | Mild to severe | |
| Mortality | <1% | Approximately 3%–4% | |
| Diagnostics | Antigen detection assays, RT-PCR, multiplex PCR, rapid molecular assays | NAAT most commonly RT-PCR assay | |
| Laboratory findings | Leukocyte counts: normal/low early in the illness elevated later in the illness | Lymphopenia, elevated AT levels, elevated LDH, elevated inflammatory markers (ferritin, CRP, ESR), abnormal coagulation tests | |
| Chest X-ray findings | Bilateral reticular or reticulonodular opacities with or without superimposed consolidation | Consolidation and GGO | |
| Vaccines | FDA-licensed influenza vaccines available; with variable efficacy from season to season | No available vaccine, clinical trials in progress Convalescent blood therapy proposed | |
| Treatments | FDA-approved antiviral drugs: oseltamivir, zanamivir, peramivir, baloxavir | No treatment available, clinical trials in progress. Proposed antiviral agent remdesivir and dexamethasone | |
| Complications | ARDS (less common), rhabdomyolysis, acute myocardial infarction, myocarditis and pericarditis, toxic shock syndrome, Guillain–Barre syndrome, transverse myelitis, encephalopathy | ARDS (more common), myocarditis, heart failure, acute coronary syndrome, arrhythmias, cardiogenic shock, thromboembolic complications (pulmonary embolism, acute limb ischemia, mesenteric thrombosis, acute stroke), multisystem inflammatory syndrome, and Guillain–Barre syndrome. |
- Abbreviations: ARDS, acute respiratory distress syndrome; AT, aminotransaminase; COVID-19, coronavirus diseases 2019; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Flu, influenza; GGO, ground-glass opacities; LDH, lactate dehydrogenase levels; NAAT, nucleic acid amplification testing; RT-PCR, reverse-transcription polymerase chain reaction; ss, single strand.
Coinfections contribute to the morbidity and mortality accompanied by influenza infection (Dunning et al., 2020). Early data from China showed that nearly 50% of the patients who deceased due to COVID-19 disease were also infected with the influenza virus at the time (Huang et al., 2020). Viral infections of the respiratory tract predispose individuals to more severe forms of COVID-19. Cases of coinfection with SARS-CoV-2 and influenza A virus have been frequently reported, bringing about certain challenges in the diagnosis and treatment of concordant infections disease (Khorramdelazad et al., 2021). There are also other reports with more lenient results, suggesting a 10% rate of coinfection at the highest (N. Chen et al., 2020; Table 3). Additionally, as of December 30, 2021, Israel has coined the term “Florona” to describe coinfection with SARS-CoV-2 and influenza A virus. In Israel, a pregnant woman was reported to have “Florona” without a vaccination history (https://www.ndtv.com/world-news/israel-detects-first-case-of-florona-disease-report-2681965). Deductively, Florona is not caused by a new variant of SARS-CoV-2. It is a term referring to simultaneous infection with COVID-19 and influenza (Meena, 2019).
| Patient/case | Coinfection | Characteristics | Medical history | Diagnostics | Therapeutics | Outcome | Reference |
|---|---|---|---|---|---|---|---|
| A 66-year-old woman, ex-smoker | Flu A and COVID-19 | Syncopal episode: fever (38.9°C), nonproductive cough, shortness of breath, decreased appetite, ABG: pH 7.3, PO2: 59 mmHg, PCO2: 45 mmHg, Hb: 13.8 g/dl, Creatinine phosphokinase: 89U/I | Ischemic cardiomyopathy, T2DM, hypertension, CAD, and CKD (baseline Cr: 1.3) | Flu A test: positive, COVID-19 nasopharyngeal swab testing: positive CXR: right lower lobe infiltrate |
Tamiflu 30 mg by mouth, twice a day for 5 days, azithromycin, ceftriaxone, hydroxychloroquine, Losartan, IV normal saline, transferred to ICU, high-flow oxygen, intubated/ventilated | Renal failure, dehydrated, Urine output increased, improved Cr, ventilator-dependent with minimal settings with an FiO2 of 30%, tracheostomy, and percutaneous gastrostomy tube placement | Konala et al. (2020) |
| 78-year-old woman, nonsmoker | Flu A virus and SARS-CoV-2 | General malaise, anorexia, SpO2: 98%–95%, cough, max temp: 37.7°C, RR: 20 breaths/min, heart rate: 106 beats/min, BP: 139/63 mmHg; elevated CRP, AST: 106 U/L, ALT: 80 U/L, GGT: 153 U/L, ALP: 372 U/L, LDH: 383 U/L | Dyslipidemia and hypothyroidism | CXR: bilateral reticular shadow CT: GGO adjacent to the pleura PCR: positive |
Oseltamivir with ceftriaxone 2 g/day, azithromycin 500 mg/day | Afebrile, worsened general malaise. Improvements in GGO more like a consolidation, improvement in clinical symptoms and CT findings, positive PCR, negative PCR, patient discharged, not require oxygen therapy | Azekawa et al. (2020) |
| P1–3: men aged 53, 78, and 56 years, P4: a woman aged 81 years | SARS-CoV-2 and Flu A/B | Nonproductive cough, fever, dyspnea | All: hypertension: P1 and P4: CKD on hemodialysis P2 and P4: T2D |
Physical examination: all patients (except P3): tachypnea and bronchospasm, low oxygen saturation CXR: P2: bilateral infiltrates, P4: right bilobar pneumonia Rapid NA amplification test: P1 and P2: positive for Flu A, P3: positive for both Flu A and B, P4: positive for Flu B RT-PCR: All positive for SARS-COV-2 |
P1, P2, P4: acute respiratory deterioration, orotracheal intubation, mechanical ventilation Lopinavir–Ritonavir 400/100 mg twice a day hydroxychloroquine 200 mg twice a day oseltamivir 150 mg twice a day, subcutaneous interferonβ−1b 8MU every 48 h |
P3: discharged after 48 h without treatment or any complication P1: clinical improvement with minimal oxygen requirements P1 and P4 remained under mechanical ventilation |
Cuadrado-Payán et al. (2020) |
| 1 male and 2 females with mean age of 59.6 years | Flu and COVID-19 | Cough, fever, shortness of breath, myalgia, positive blood culture for Enterococcus faecium, elevated Inflammatory markers (ESR, CRP, IL-6) | Hypertension and DM | Positive nasopharyngeal swab RT-PCR for COVID-19. Rapid antigen assay: P1, P2: Flu B; P3: Flu A. CXR: P1: bilateral patchy infiltrates P2: multilobar infiltrates, P3: bilateral patchy infiltrates CT: P1: diffuse scattered areas of GGO and mixed attenuating opacities P2: diffuse bilateral GGO infiltrates |
All patients: hydroxychloroquine, azithromycin, ceftriaxone for COVID-19 and oseltamivir for influenza | All discharged in stable condition | B. Singh et al. (2020) |
| A 4-month-old infant | Flu A and SARS-COV-2 | Fever (38.2°C), cough, nasal congestion, clear rhinorrhea | - | Flu rapid immunochromatographic assay testing, RT-PCR | Satisfying oral fluid intake and excretions. Oseltamivir for 5 days |
- | Wehl et al. (2020) |
| 4 patients: a 74-year-old woman; 40-year-old healthy man; a 64-year-old man; 50-year-old healthy man | SARS-CoV-2 and Flu A | Pneumonia symptoms P1: dry cough, malaise, body pain, subjective fever, headache, anorexia, dyspnea, orthopnea, BP: 70/50 mmHg, body temp: 38.7°C, PR: 89 beat/min, RR: 26 breath/min, O2 saturation: 90% P2: headache, fever, developed sweating, chills, cough, severe compressive chest pain, dyspnea, orthopnea, body pain, diarrhea, chest pain worsened, respiratory distress, sweating, a low-grade fever, severe compressive chest pain, orthopnea, body pain, BP: 110/70 mmHg, body temp: 35.4°C, PR: 77 beat/min, RR: 20 breath/min, O2 saturation: 97% P3: dry cough, malaise, headache, subjective fever, dyspnea, BP:130/80 mmHg, body temp: 37.7°C, PR: 110 beat/min, RR: 19 breath/min, O2 saturation: 87% P4: fever, dry cough, and dyspnea, BP: 120/65 mm, body temp: 38.0°C, PR: 85 beat/min, RR: 18 breath/min, O2 saturation: 93% |
P1: ischemic cerebrovascular accident and hypertension | RT-PCR test: P1, P2, P3, P4 Flu viruses test: Flu A: P1, P2, P3, P4 CXR: P1: diffuse infiltrates in both lungs, P2: diffuse and bilateral infiltration in the lungs, P3: diffuse and bilateral infiltration in the lungs, P4: diffuse infiltrates in both lungs |
- | - | Khodamoradi et al. (2020) |
| 69-year-old man, China | Covid-19 and influenza | Cough and fever, a ground-glass consolidation lesion in the right inferior lobe of lungs, No Leukopenia 1 week later: persistent fever and worsening dyspnea , leukopenia |
No underlying diseases | RT-PCR: negative SARS-CoV-2, Xpert Flu/RSV Xpress assay of the nasopharyngeal swab: positive influenza A and negative for SARS-CoV-2 1 week later: RT-PCR: positive SARS |
- | - | Wu et al. (2020) |
| 4 patients, Spain | Covid-19 and influenza | Persistent nonproductive cough, fever, dyspnea | Diabetes and severe kidney disorder | Rapid NA amplification assay: positive influenza type A and B RT-PCR: positive for SARS-CoV-2 |
- | - | Cuadrado-Payán et al. (2020) |
| A 66-year-old woman, African American | Covid-19 and influenza | Fever (38.9°C), nonproductive cough, anorexia, shortness of breath | Chronic kidney disease, diabetes, coronary artery disease, and hypertension | Laboratory tests: positive COVID-19, positive influenza | - | - | Konala et al. (2020) |
| 115 patients, China | Covid-19 and influenza | Pneumonia, during the admission; Lymphopenia: during the remission Total lymphocyte count was gradually raised 5 coinfected patients with fever, cough, fatigue, and headache; unusual symptoms such as a nasal tampon, pharyngalgia, diarrhea, and mild hemoptysis |
No underlying diseases | 115 patients with positive SARS-CoV-2 infection, 5 patients with positive influenza virus | - | - | Ding et al. (2020); N. Chen et al. (2020); D. Wang, Hu et al. (2020) |
- Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BP, blood pressure; CAD, coronary artery disease; CKD, chronic kidney disease; Cr, creatinine; CRP, C-reactive protein; CT, computed tomography; DM, diabetes mellitus; Flu, influenza; GGO, ground-glass opacities; GGT, g-glutamyltransferase; Hb, Hemoglobin; ICU, intensive care unit; IV, intravenous; LDH, lactate dehydrogenase; max temp, maximum temperature; NA, nucleic acid; P, patient; PCR, polymerase chain reaction; PR, pulse rate; RR, respiratory rate; T2D, type 2 diabetes; T2DM, type 2 diabetes mellitus.
An important issue with the molecular tests used currently to diagnose COVID-19 is the uncertainty regarding the adequacy of the samples obtained from patients. Another challenge is the false-negative test results for COVID-19 in cases of simultaneous infection with another respiratory virus (Khorramdelazad et al., 2021). It seems that distinguishing COVID-19 from seasonal influenza based on clinical manifestation is another challenge, as both diseases present with fever, nonproductive cough, and dyspnea. To avoid this, it is recommended that RT-PCR and other tests based on nucleic acids be taken in all cases with an indeterminate respiratory infection. This could also help prevent further disease propagation by misdiagnosed patients (Wu et al., 2020).
More recently, bioinformatics analyses have been considered in various fields. Molecular docking studies are conducted for unraveling the binding of protein–ligand complexes (R. Singh et al., 2022). These investigations have been of great value in the case of repurposing old drugs and identifying new therapeutic targets for COVID-19, such as the SARS-CoV-2 main protease (Rangsinth et al., 2021; Zaki et al., 2022), papain-like protease (R. Singh et al., 2022), spike protein, and RNA-dependent RNA polymerase (Rangsinth et al., 2021; Zaki et al., 2022). In 2021, Singh and colleagues suggested Tea (Camellia sinensis), theaflavin, BCH derivates (BCH10, BCH15, BCH16, and BCH17), dicaffeoylquinic acid, diacetylcurcumin, curcumin, and diacetylcurcumin candidate therapeutic agents for inhibiting nonstructural protein 16 (NSP16), nonstructural protein 1 (Nsp1), the Spike receptor-binding domain, and RNA-dependent RNA polymerase (RdRp) of SARS-CoV-2, respectively (R. Singh et al., 2022; R. Singh, Bhardwaj, & Purohit, 2021; R. Singh, Bhardwaj, Das, et al., 2021; R. Singh, Bhardwaj, Sharma, et al., 2021). The same year, Sharma et al. (2021) confirmed the inhibitory potential of three tea derivates (barrigenol, kaempferol, and myricetin) against nonstructural protein 15 (Nsp15) of SARS-CoV2. Later, Bhardwaj and colleagues indicated that the DSPD derivate (DSPD-2, DSPD-6, DSPD-5) bound effectively to the S1 subunit of SARS-CoV-2 S protein, as well as Oolonghomobisflavan-A that could bind and neutralize the SARS-CoV-2 main protease (Bhardwaj, Singh, Das, et al., 2021; Bhardwaj, Singh, Sharma, et al., 2021a). Further investigations identified three bioactive molecules from tea (epicatechin-3,5-di-O-gallate, epigallocatechin-3,5-di-O-gallate, and epigallocatechin-3,4-di-O-gallate) that displayed more effective binding with the enzyme RdRp than antiviral drugs remdesivir and favipiravir (Bhardwaj, Singh, Sharma, et al., 2021b). Figure 1 represents the schematic procedure of the present study.
2 THERE ARE MANY CONCERNS
2.1 What can we expect as the COVID-19 outbreak continues?
The H1N1pdm09 virus caused the last influenza outbreak in 2009, which led to approximately 60 million cases of infection, over 274,000 hospitalizations, and 12,500 deaths in the United States throughout the following year (Shrestha et al., 2011). Almost a decade later, the virus can still be contracted even though it has been included in the influenza vaccine ever since the original outbreak. In fact, H1N1pdm09 was the dominant viral strain during the 2019–2020 annual outbreak of influenza. The same, however, cannot be applied to coronaviruses, as the causative strain behind the last human coronavirus epidemic, known as SARS, was successfully contained as a result of rigorous containment procedures before the complete development of a vaccine. Concerning the rebellious course of the COVID-19 outbreak and the timeline of vaccine development programs, it is safe to say that SARS-CoV-2 will not follow the abrupt termination of its predecessor. Instead, likely, SARS-CoV-2 will still be contracted in communities as we face the subsequent influenza epidemic (Singer, 2020).
2.2 What are the odds of coinfection with COVID-19 and seasonal influenza?
According to D. Kim et al. (2020), nearly 20% of patients infected with SARS-CoV-2 were concurrently infected with at least one other respiratory pathogen, most notably the influenza virus. There are critical diagnostic implications to this issue. In patients with respiratory symptoms, detecting any respiratory pathogen other than SARS-CoV-2 might not be a valid alternative to rule out COVID-19 infection, especially in areas with limited laboratory resources for SARS-CoV-2 detection in the first place. These findings imply the urgent need for on-demand access to diagnostic tools to detect SARS-CoV-2 and other respiratory pathogens (Singer, 2020).
2.3 How can the COVID-19 epidemic and seasonal influenza aid us in developing strategies for proper preparation?
Both the influenza virus and SARS-CoV-2 spread primarily via droplets expelled from the respiratory tract. Thus, self-isolation and social distancing methods suggested for the containment of COVID-19 transmission can also be useful against influenza (Fong et al., 2020). Accordingly, should the transmission rate of COVID-19 spike in the fall of this year, the corresponding preventive measures are most likely to taper the spread of the influenza virus (Singer, 2020). In terms of higher-level prevention, influenza is thought to be adequately amenable to antiviral therapy in the majority of patients (Dunning et al., 2020). SARS-CoV-2, on the contrary, is still being investigated for target pathways in its pathogenesis that might render the virus vulnerable to antiviral agents (S. Lu, 2020). In the case of influenza, vaccine efficacy is a determining factor that depends on the inclusion of the most recently extracted antigens in the vaccine. The effectiveness of the 2019–2020 influenza vaccine was reported to be 45% in the United States, which is not ideal considering that the vaccine contained the circulating influenza antigen in that year (Dawood et al., 2020). Despite recommendations for global vaccination, the Influenza vaccine merely covered 45% of adults during the last season in the United States (Centers for Disease Control and Prevention, 2017). Then again, it is encouraged to pursue research and development programs on COVID-19 vaccines. Efforts must be focused on devising strategies to contain potentially infectious agents that might superimpose on SARS-CoV-2, such as the influenza A virus (Singer, 2020).
2.4 Bioinformatics provide us with such mathematical models
Mathematical models have long been of particular value for understanding the mechanisms and dynamics of infections. One of the first iterations of such models was developed by Perelson et al. in 1996 to explore the dynamics of human immunodeficiency virus (HIV) infection (Perelson et al., 1996), which was later adapted by Nowak et al. and Neumann et al. to investigate hepatitis B (HBV) (Nowak et al., 1996) and hepatitis C viruses (HCV) (Neumann et al., 1998). Later, HCV was further investigated by Wodarz et al. (in 2003) in terms of adaptive immunity (Wodarz, 2003). In 2015, Hattaf and colleagues adapted these models to study HIV, Ebola, and Zika viruses (Hattaf & Yousfi, 2016; Hattaf et al., 2015). It is recommended that several conditions, known as delays, be considered in the study of infectious diseases. Infection of the host cell and virus replication are two such delays that occur instantaneously. Equations developed to address these delays are termed delay differential equations (Hattaf & Yousfi, 2020). Such equations were used by Zhuo (2012) for studying HBV infection with noncytolytic loss of infected cells and by Hattaf and Yousfi (2016), Raid (2016), and Mahrouf et al. (2017) as well. The equation introduced by Hattaf and Yousfi (2016) was a partial differential equation that allowed them to explain the evolution in time and space of infectious diseases. This model assumed that normal and infected cells, along with viral particles and antibodies are mixed together, and ignored their mobility. However, it is thought that the motion of these entities follows the Fickian diffusion. In this connection, the fluxes of these entities are correlated with their concentration gradient, flowing from the regions of high concentration to the regions of low concentration (Hattaf & Yousfi, 2020).
2.5 Can mathematical models be of help in estimating viral coinfection amid the COVID-19 pandemic?
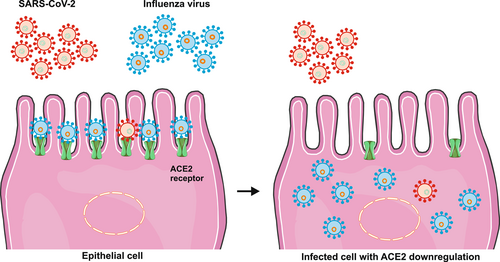
Mathematical models have had an essential role in extending our understanding of the dynamics of viral respiratory infections (Baccam et al., 2006). They have also been of particular interest to scientists studying coinfections (Pinky & Dobrovolny, 2020). According to one such mathematic model developed recently, viral strains with a faster growth rate can dominate strains with a slower growth rate. This theory might yield innovative insights into the issue of viral coinfection amid the COVID-19 pandemic (Pinky & Dobrovolny, 2016). The model mentioned earlier was designed in a recent study to investigate SARS-CoV-2 coinfection with several other viruses, such as influenza A virus, parainfluenza virus, respiratory syncytial virus, human rhinovirus, and human metapneumovirus. The study found that other strains readily suppress the replication of SARS-CoV-2. This would happen because SARS-CoV-2 had a significantly lower growth rate (1.8/day) than other studied strains. These findings may have implications for the severity and timing of a potential prospective second wave of infection, should there be any. It is hypothesized that once the primary infection with SARS-CoV-2 is established, secondary infection with another strain may not result in the suppression of SARS-CoV-2 to undetectable levels (Pinky & Dobrovolny, 2020). Importantly, it has been suggested that the angiotensin-converting enzyme 2 (ACE2) plays a fundamental role in SARS-CoV-2 replication (Huang et al., 2020). It is possible that several other strains may target this molecule, and thus, result in suppression of SARS-CoV-2. The influenza virus, for instance, has been reported to downregulate ACE2 (Liu et al., 2014) (Figure 1). Nonetheless, more investigations are warranted for the exact determination of SARS-CoV-2 growth rate and its interaction with other respiratory viruses to see if coinfection with influenza might actually result in the mitigation of a potential second wave of COVID-19 outbreak (Pinky & Dobrovolny, 2020) (Figure 2).
3 CONCLUSION
Humankind has struggled with influenza for a long time, and the new reality of COVID-19 will only complicate matters in the ongoing pandemic situation. Of paramount importance are the preventive measures at every level that will help dwindle the burden of viral respiratory infection in the coming days. With lessons learned from the several influenza outbreaks through the last century, we now have sufficient clinical experience to attain similar success in the containment of the recent outburst of COVID-19. Cases of coinfection with the two strains in question can be easily diagnosed and treated thanks to the development of different vaccines as a means of primary prevention of COVID-19. In addition, repurposing several drugs as well as employing bioinformatics-based models for the influenza A virus have significantly improved clinical management of SARS-CoV-2 infection. Thus, we strongly recommend that all individuals at a greater level of risk get vaccinated against influenza in due time to reduce the likelihood of respiratory coinfections in the coming fall.
AUTHOR CONTRIBUTIONS
All authors participated in the investigation, design, interpretation of the studies and analysis of the data, and review of the manuscript.
ACKNOWLEDGMENT
This study was supported by the Zahedan University of Medical Sciences (Ethical code: IR.ZAUMS.REC.1399.197) (Webpage of ethical approval code is: https://ethics.research.ac.ir/EthicsProposalViewEn.php?id=149801).
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
Open Research
DATA AVAILABILITY STATEMENT
All data are available.




