Bioactive Compound-Fortified Nanocarriers in the Management of Neurodegenerative Disease: A Review
Aditya Singh
Department of Pharmacy, Faculty of Pharmacy, Integral University, Lucknow, Uttar Pradesh, India
Search for more papers by this authorShubhrat Maheshwari
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
Search for more papers by this authorJagat Pal Yadav
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
Search for more papers by this authorRavi Kumar
Institute of pharmaceutical sciences, J.S. University, Shikohabad, Uttar Pradesh, India
Search for more papers by this authorAmita Verma
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
School of Pharmacy, Graphic Era Hill University, Dehradun, Uttrakhand, India
Search for more papers by this authorCorresponding Author
Sudarshan Singh
Office of Research Administration, Chiang Mai University, Chiang Mai, Thailand
Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand
Correspondence: Sudarshan Singh ([email protected]) | Bhupendra G. Prajapati ([email protected])
Search for more papers by this authorCorresponding Author
Bhupendra G. Prajapati
Shree S. K. Patel College of Pharmaceutical Education and Research, Ganpat University, Gujarat, India
Faculty of Pharmacy, Silpakorn University, Nakhon Pathom, Thailand
Correspondence: Sudarshan Singh ([email protected]) | Bhupendra G. Prajapati ([email protected])
Search for more papers by this authorAditya Singh
Department of Pharmacy, Faculty of Pharmacy, Integral University, Lucknow, Uttar Pradesh, India
Search for more papers by this authorShubhrat Maheshwari
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
Search for more papers by this authorJagat Pal Yadav
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
Search for more papers by this authorRavi Kumar
Institute of pharmaceutical sciences, J.S. University, Shikohabad, Uttar Pradesh, India
Search for more papers by this authorAmita Verma
Faculty of Pharmaceutical Sciences, Sam Higginbottom University of Agriculture, Technology and Sciences, Prayagraj, India
School of Pharmacy, Graphic Era Hill University, Dehradun, Uttrakhand, India
Search for more papers by this authorCorresponding Author
Sudarshan Singh
Office of Research Administration, Chiang Mai University, Chiang Mai, Thailand
Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand
Correspondence: Sudarshan Singh ([email protected]) | Bhupendra G. Prajapati ([email protected])
Search for more papers by this authorCorresponding Author
Bhupendra G. Prajapati
Shree S. K. Patel College of Pharmaceutical Education and Research, Ganpat University, Gujarat, India
Faculty of Pharmacy, Silpakorn University, Nakhon Pathom, Thailand
Correspondence: Sudarshan Singh ([email protected]) | Bhupendra G. Prajapati ([email protected])
Search for more papers by this authorFunding: The authors received no specific funding for this work.
ABSTRACT
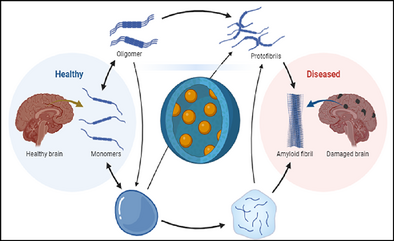
Individual around the globe faces enormous problems from illnesses of the neurological system and the cerebrum, including neurodegenerative conditions and brain tumors. There are still no demonstrated viable treatments for neurological conditions, despite advances in drug delivery technologies such as solid lipid nanoparticles, nanostructured lipid carriers, and nano-liposomes. To address this, there is growing interest in leveraging naturally occurring bioactive substances for their therapeutic potential. However, challenges such as limited bioavailability and metabolism hinder their efficacy, particularly in the brain. Although various pharmaceutical interventions exist for neurodegenerative diseases, they often come with significant side effects, and there is currently no specific treatment to cure or slow down disease progression. Challenges such as the blood–brain barrier and blood–cerebrospinal fluid barrier present significant obstacles to deliver drugs into the brain. Strategies to improve drug penetration across these barriers include targeting specific transport systems and developing innovative drug delivery approaches. Hence, the development of nanocarriers capable of targeting bioactive compounds to the brain represents a promising approach for neurodegenerative disease therapy. This review explores the potential of bioactive compound-fortified nano-delivery systems for treating neurodegenerative diseases, with various compounds offering unique avenues for investigating neurodegeneration pathways and strategies in overcoming associated challenges.
Graphical Abstract
Conflicts of Interest
The authors declare no conflicts of interest.
Open Research
Data Availability Statement
Data will be made available on request.
References
- 1A. Singh, V. A. Ansari, T. Mahmood, F. Ahsan, and R. Wasim, Drug Research 72 (2022): 496.
- 2H. Luo, Y. Xiang, X. Qu, et al., “Apelin-13 Suppresses Neuroinflammation Against Cognitive Deficit in a Streptozotocin-Induced Rat Model of Alzheimer's Disease Through Activation of BDNF-TrkB Signaling Pathway,” Frontiers in Pharmacology 10 (2019): 395.
- 3F. Kong, Z. Xu, G. Yang, et al., “Microelectrode Arrays for Detection of Neural Activity in Depressed Rats: Enhanced Theta Activity in the Basolateral Amygdala,” Cyborg and Bionic Systems 5 (2024): 0125.
- 4Z. Song, Z. Jiang, Z. Zhang, et al., “Evolving Brain Network Dynamics in Early Childhood: Insights from Modular Graph Metrics,” Neuroimage 297 (2024): 120740.
- 5H. Feng, Q. C. Qiao, Q. F. Luo, et al., Research (Wash D C) 7 (2024): 0355.
- 6B. Chauhan, S. Patel, B. G. Prajapati, and S. Singh, “ Drug Delivery for Alzheimer's Disease Using Nanotechnology: Challenges and Advancements,” ed. B. G. Prajapati, D. K. Chellappan, and P. N. Kendre. (Academic Press, 2024).
- 7A. Chowdhury, S. Kunjiappan, T. Panneerselvam, B. Somasundaram, and C. Bhattacharjee, “Nanotechnology and Nanocarrier-Based Approaches on Treatment of Degenerative Diseases,” International Nano Letters 7 (2017): 91–122.
- 8D. Zhang, J. Song, Z. Jing, et al., “Stimulus Responsive Nanocarrier for Enhanced Antitumor Responses Against Hepatocellular Carcinoma,” International Journal of Nanomedicine 19 (2024): 13339–13355.
- 9Q.-Y. Zhang, Q. Wang, J.-X. Fu, et al., “Multi Targeted Therapy for Alzheimer's Disease by Guanidinium-Modified Calixarene and Cyclodextrin Co-Assembly Loaded With Insulin,” ACS Nano 18 (2024): 33032–33041.
- 10M. M. Ibrahim and M. T. Gabr, Neural Regeneration Research 14 (2019): 437.
- 11A. Puri, P. Mohite, S. Khan, and S. Singh, “Breaking the Barriers in Management of Alzheimer's Disease Through Cationic Nanoformulation: A Review,” Results in Chemistry 7 (2024): 101463.
- 12A. Singh, V. A. Ansari, T. Mahmood, et al., Drug Research 73 (2023): 247.
- 13C. Saraiva, C. Praça, R. Ferreira, T. Santos, L. Ferreira, and L. Bernardino, “Nanoparticle-Mediated Brain Drug Delivery: Overcoming Blood–Brain Barrier to Treat Neurodegenerative Diseases,” Journal of Controlled Release 235 (2016): 34–47.
- 14J. Miao, H. Ma, Y. Yang, et al., “Microglia in Alzheimer's Disease: Pathogenesis, Mechanisms, and Therapeutic Potentials,” Frontiers in Aging Neuroscience 15 (2023).
- 15N. S. Kiran, G. Vaishnavi, S. Singh, et al., Regenerative Engineering and Translational Medicine (2024).
- 16L. R. Conroy, T. R. Hawkinson, L. E. A. Young, M. S. Gentry, and R. C. Sun, Trends in Endocrinology & Metabolism 32 (2021): 980.
- 17B. Hu, F. Dai, Z. Fan, G. Ma, Q. Tang, and X. Zhang, “Nanotheranostics: Congo Red/Rutin-MNPs With Enhanced Magnetic Resonance Imaging and H2O2-Responsive Therapy of Alzheimer's Disease in APPswe/PS1dE9 Transgenic Mice,” Advanced Materials 27 (2015): 5499–5505.
- 18J. Tang, L. Xiong, G. Zhou, et al., “Silver Nanoparticles Crossing through and Distribution in the Blood-Brain Barrier In Vitro,” Journal of Nanoscience and Nanotechnology 10 (2010): 6313–6317.
- 19F. Talebpour and A. Ghahghaei, “Effect of Green Synthesis of Gold Nanoparticles (AuNPs) From Hibiscus sabdariffa on the Aggregation of α-Lactalbumin,” International Journal of Peptide Research and Therapeutics 26 (2020): 2297–2306.
- 20Y. C. Kuo and H. C. Tsai, “Rosmarinic Acid- and Curcumin-Loaded Polyacrylamide-Cardiolipin-Poly(Lactide-co-Glycolide) Nanoparticles with Conjugated 83–14 Monoclonal Antibody to Protect β-Amyloid-Insulted Neurons,” Materials Science & Engineering C-Materials for Biological Applications 91 (2018): 445–457.
- 21M. Mohajeri, B. Behnam, G. E. Barreto, and A. Sahebkar, “Carbon Nanomaterials and Amyloid-Beta Interactions: Potentials for the Detection and Treatment of Alzheimer's Disease?,” Pharmacological Research 143 (2019): 186–203.
- 22J. Liu, L. Cui, and D. Losic, “Graphene and Graphene Oxide as New Nanocarriers for Drug Delivery Applications,” Acta Biomaterialia 9 (2013): 9243–9257.
- 23H. Li, Y. Tan, X. Cheng, et al., “Untargeted Metabolomics Analysis of the Hippocampus and Cerebral Cortex Identified the Neuroprotective Mechanisms of Bushen Tiansui Formula in an aß25-35-induced Rat Model of Alzheimer's Disease,” Frontiers in Pharmacology (2022): 13.
- 24M. Cheng, T. Li, E. Hu, et al., “A Novel Strategy of Integrating Network Pharmacology and Transcriptome Reveals Antiapoptotic Mechanisms of Buyang Huanwu Decoction in Treating Intracerebral Hemorrhage,” Journal of Ethnopharmacology 319 (2024): 117123.
- 25E. Hu, Z. Li, T. Li, et al., “A Novel Microbial and Hepatic Biotransformation-Integrated Network Pharmacology Strategy Explores the Therapeutic Mechanisms of Bioactive Herbal Products in Neurological Diseases: The Effects of Astragaloside IV on Intracerebral Hemorrhage as an Example,” Chinese Medicine 18 (2023): 40.
- 26R. Agrawal, P. Jurel, R. Deshmukh, et al., “Emerging Trends in the Treatment of Skin Disorders by Herbal Drugs: Traditional and Nanotechnological Approach,” Pharmaceutics 16 (2024): 869.
- 27J. Angsusing, S. Singh, W. Samee, et al., “Anti-Inflammatory Activities of Yataprasen Thai Traditional Formulary and Its Active Compounds, Beta-Amyrin and Stigmasterol, in RAW264.7 and THP-1 Cells,” Pharmaceuticals 17 (2024): 1018.
- 28O. F. Nwabor, K. Vongkamjan, and S. P. Voravuthikunchai, “Antioxidant Properties and Antibacterial Effects of Eucalyptus Camaldulensis Ethanolic Leaf Extract on Biofilm Formation, Motility, Hemolysin Production, and Cell Membrane of the Foodborne Pathogen Listeria Monocytogenes,” Foodborne Pathogens and Disease 16 (2019): 581–589.
- 29O. F. Nwabor, S. Singh, D. Marlina, and S. P. Voravuthikunchai, “Chemical Characterization, Release, and Bioactivity of Eucalyptus Camaldulensis Polyphenols From Freeze-Dried Sodium Alginate and Sodium Carboxymethyl Cellulose Matrix,” Food Quality and Safety 4 (2020): 203–212.
- 30O. F. Nwabor, S. Singh, D. M. Syukri, and S. P. Voravuthikunchai, “Bioactive Fractions of Eucalyptus Camaldulensis Inhibit Important Foodborne Pathogens, Reduce Listeriolysin O-Induced Haemolysis, and Ameliorate Hydrogen Peroxide-Induced Oxidative Stress on Human Embryonic Colon Cells,” Food Chemistry 344 (2021): 128571.
- 31V. R. Chidrawar, S. Singh, T. J. Jayeoye, R. Dodiya, W. Samee, and C. Chittasupho, “Porous Swellable Hypromellose Composite Fortified With Eucalyptus Camaldulensis Leaf Hydrophobic/Hydrophilic Phenolic-Rich Extract to Mitigate Dermal Wound Infections,” Journal of Polymers and the Environment 31 (2023): 3841–3856.
- 32S. Singh, D. M. Syukri, Y. V. Ushir, et al., Journal of Polymers and the Environment (2024).
- 33D. M. Syukri and S. Singh, “ Medicinal and Nutritional Importance of Eucalyptus Camaldulensis in Human Health,” ed. M. A. Ansari, S. Shoaib, and N. Islam. (Springer Nature Singapore, 2024).
- 34J. C. Ontong, S. Singh, T. Siriyong, and S. P. Voravuthikunchai, “Transferosomes Stabilized Hydrogel Incorporated Rhodomyrtone-Rich Extract From Rhodomyrtus Tomentosa Leaf Fortified With Phosphatidylcholine for the Management of Skin and Soft-Tissue Infections,” Biotechnology Letters 46 (2024): 127–142.
- 35J. Chorachoo Ontong, S. Singh, O. F. Nwabor, et al., “Microwave-Assisted Extract of Rhodomyrtone From Rhodomyrtus Tomentosa Leaf: Anti-Inflammatory, Antibacterial, Antioxidant, and Safety Assessment of Topical Rhodomyrtone Formulation,” Separation Science and Technology 58 (2023): 929–943.
- 36O. F. Nwabor and S. Singh, “A Systematic Review on Rhodomyrtus Tomentosa (Aiton) Hassk: A Potential Source of Pharmacological Relevant Bioactive Compounds With Prospects as Alternative Remedies in Varied Medical Conditions,” International Journal of Pharmaceutical Sciences and Nanotechnology (IJPSN) 15 (2022): 5875–5891.
10.37285/ijpsn.2022.15.2.7 Google Scholar
- 37S. Wunnoo, S. Bilhman, T. Amnuaikit, et al., “Rhodomyrtone as a New Natural Antibiotic Isolated From Rhodomyrtus Tomentosa Leaf Extract: A Clinical Application in the Management of Acne Vulgaris,” Antibiotics 10 (2021): 108.
- 38S. Singh, V. R. Chidrawar, D. Hermawan, et al., “Solvent-Assisted Dechlorophyllization of Psidium Guajava Leaf Extract: Effects on the Polyphenol Content, Cytocompatibility, Antibacterial, Anti-Inflammatory, and Anticancer Activities,” South African Journal of Botany 158 (2023): 166–179.
- 39S. Singh, V. R. Chidrawar, D. Hermawan, et al., “Hypromellose Highly Swellable Composite Fortified With Psidium Guajava Leaf Phenolic-Rich Extract for Antioxidative, Antibacterial, Anti-Inflammatory, Anti-Melanogenesis, and Hemostasis Applications,” Journal of Polymers and the Environment 31 (2023): 3197–3214.
- 40O. J. Olatunji, O. O. Olatunde, T. J. Jayeoye, et al., “New Insights on Acanthus ebracteatus Vahl: UPLC-ESI-QTOF-MS Profile, Antioxidant, Antimicrobial and Anticancer Activities,” Molecules (Basel, Switzerland) 27 (2022): 1981.
- 41I. V. Pylypchuk, P. A. Lindén, M. E. Lindström, and O. Sevastyanova, ACS Sustainable Chemistry & Engineering 8 (2020): 13805.
- 42H. Wang, Z. Yan, W. Yang, et al., “A Strategy of Monitoring Acetylcholinesterase and Screening of Natural Inhibitors From Uncaria for Alzheimer's Disease Therapy Based on Near-Infrared Fluorescence Probe,” Sensors and Actuators B: Chemical 424 (2025): 136895.
- 43D. M. S. Pooja V Nagime, T. Sjahriani, D. Hermawan, et al., Nano-Structures & Nano-Objects (2024).
- 44P. V. Nagime, N. M. Shaikh, S. B. Shaikh, et al., “Facile Synthesis of Silver Nanoparticles Using Calotropis procera Leaves: Unraveling Biological and Electrochemical Potentials,” Discover Nano 19 (2024): 139.
- 45T. J. Jayeoye, S. Singh, F. N. Eze, et al., “Exploration of Biocompatible Ascorbic Acid Reduced and Stabilized Gold Nanoparticles, as Sensitive and Selective Detection Nanoplatform for Silver Ion in Solution,” Plasmonics (2024), https://doi.org/10.1007/s11468-024-02413-2.
- 46T. J. Jayeoye, S. Singh, F. N. Eze, et al., “Green Synthesis of Silver Nanoparticles Using Cyto-Compatible Polymer Derivative of Tara Gum for Gold (III) Ion Detection in Water Samples,” Journal of Polymers and the Environment 32 (2024): 6667–6686, https://doi.org/10.1007/s10924-024-03393-4.
- 47A. Puri, P. Mohite, S. Patil, et al., “Facile Green Synthesis and Characterization of Terminalia Arjuna Bark Phenolic–Selenium Nanogel: A Biocompatible and Green Nano-Biomaterial for Multifaceted Biological Applications,” Frontiers in Chemistry (2023): 11.
- 48P. V. Nagime, S. Singh, N. M. Shaikh, et al., “Biogenic Fabrication of Silver Nanoparticles Using Calotropis procera Flower Extract With Enhanced Biomimetics Attributes,” Materials 16 (2023): 4058.
- 49J. C. Ontong, S. Singh, O. F. Nwabor, S. Chusri, and S. P. Voravuthikunchai, “Potential of Antimicrobial Topical Gel With Synthesized Biogenic Silver Nanoparticle Using Rhodomyrtus Tomentosa Leaf Extract and Silk Sericin,” Biotechnology Letters 42 (2020): 2653–2664.
- 50O. F. Nwabor, S. Singh, S. Paosen, K. Vongkamjan, and S. P. Voravuthikunchai, “Enhancement of Food Shelf Life with Polyvinyl Alcohol-Chitosan Nanocomposite Films From Bioactive Eucalyptus Leaf Extracts,” Food Bioscience 36 (2020): 100609.
- 51D. M. Syukri, S. Singh, O. F. Nwabor, et al., “Prevention of Post-Operative Bacterial Colonization on Mice Buccal Mucosa Using Biogenic Silver Nanoparticles-Coated Nylon Sutures,” Regen Eng Transl Med 10 (2024): 294–308, https://doi.org/10.1007/s40883-024-00335-3.
- 52F. N. Eze, R. C. Eze, S. Singh, and K. E. Okpara, “Fabrication of a Versatile and Efficient Ultraviolet Blocking Biodegradable Composite Film Consisting of Tara Gum/PVA/Riceberry Phenolics Reinforced With Biogenic Riceberry Phenolic-Rich Extract-Nano‑Silver,” International Journal of Biological Macromolecules 278 (2024): 134914.
- 53A. K. Sachdeva and K. Chopra, “Lycopene Abrogates Aβ(1–42)-Mediated Neuroinflammatory Cascade in an Experimental Model of Alzheimer's Disease,” Journal of Nutritional Biochemistry 26 (2015): 736–744.
- 54L. Yu, W. Wang, W. Pang, Z. Xiao, Y. Jiang, and Y. Hong, “Dietary Lycopene Supplementation Improves Cognitive Performances in Tau Transgenic Mice Expressing P301L Mutation via Inhibiting Oxidative Stress and Tau Hyperphosphorylation,” Journal of Alzheimer's Disease 57 (2017): 475–482.
- 55A. Babazadeh, F. M. Vahed, Q. Liu, S. A. Siddiqui, M. S. Kharazmi, and S. M. Jafari, “Natural Bioactive Molecules as Neuromedicines for the Treatment/Prevention of Neurodegenerative Diseases,” ACS Omega 8 (2023): 3667–3683.
- 56K. Wang, Y. Wang, K. Li, et al., “Uptake, Translocation and Biotransformation of Selenium Nanoparticles in Rice Seedlings (Oryza sativa L.),” Journal of Nanbiotechnology 18 (2020): 103, https://doi.org/10.1186/s12951-020-00659-6.
- 57A. Pruss-Ustun, L. Fewrell, P. Landrigan, and J. Ayuso-Mateos, “Lead Exposure. Comparative Quantification of Health Risks,” World Health Organization (2004): 1495–1542.
- 58O. V. Taso, A. Philippou, A. Moustogiannis, E. Zevolis, and M. Koutsilieris, “Lipid Peroxidation Products and Their Role in Neurodegenerative Diseases,” Annals of Research Hospitals 3 (2019): 2.
10.21037/arh.2018.12.02 Google Scholar
- 59N. Majlessi, S. Choopani, M. Kamalinejad, and Z. Azizi, “Amelioration of Amyloid Ss-Induced Cognitive Deficits by Zataria multiflora Boiss. Essential Oil in a Rat Model of Alzheimer's Disease.” CNS Neuroscience & Therapeutics 18 (2012): 295–301, https://doi.org/10.1111/j.1755-5949.2011.00237.x.
- 60A. Singh, R. Kukreti, L. Saso, and S. Kukreti, “Oxidative Stress: A Key Modulator in Neurodegenerative Diseases,” Molecules (Basel, Switzerland) 24 (2019): 1583.
- 61A. Singh, V. A. Ansari, T. Mahmood, et al., “Targeting Abnormal Tau Phosphorylation for Alzheimer's Therapeutics,” Hormone and Metabolic Research 56, no. 07 (2024): 482–488.
- 62P. A. Postu, F. Z. Sadiki, M. El Idrissi, et al., “Pinus Halepensis Essential Oil Attenuates the Toxic Alzheimer's Amyloid Beta (1-42)-induced Memory Impairment and Oxidative Stress in the Rat Hippocampus,” Biomedicine & Pharmacotherapy 112 (2019): 108673.
- 63J. Gao, L. Wang, J. Liu, F. Xie, B. Su, and X. Wang, “Abnormalities of Mitochondrial Dynamics in Neurodegenerative Diseases,” Antioxidants 6 (2017): 25.
- 64A. F. Esfanjani, E. Assadpour, and S. M. Jafari, “Mproving the Bioavailability of Phenolic Compounds by Loading Them Within Lipid-Based Nanocarriers,” Trends in Food Science & Technology 76 (2018): 56–66.
- 65S. D. Stan, S. Kar, G. D. Stoner, and S. V. Singh, “Bioactive Food Components and Cancer Risk Reduction,” Journal of Cellular Biochemistry 104 (2008): 339–356.
- 66M. B. Bahadori, B. Kirkan, and C. Sarikurkcu, “Phenolic Ingredients and Therapeutic Potential of Stachys Cretica Subsp. Smyrnaea for the Management of Oxidative Stress, Alzheimer's Disease, Hyperglycemia, and Melasma,” Industrial Crops and Products 127 (2019): 82–87.
- 67B. O. Ajiboye, O. A. Ojo, M. A. Okesola, et al., “In Vitro Antioxidant Activities and Inhibitory Effects of Phenolic Extract of Senecio Biafrae (Oliv and Hiern) Against Key Enzymes Linked With Type II Diabetes Mellitus and Alzheimer's Disease,” Food Sci Nutr 6 (2018): 1803–1810, https://doi.org/10.1002/fsn3.749.
- 68A. Abdulqadir, Y. S. Cakmak, and G. Zengin, “Phenolic Compounds, Antioxidant Properties and Enzyme Inhibition Ability of Adiantum Capillus Veneris L. Linked to Alzheimer's Disease, Diabetes Mellitus and Skin Disorders,” Current Organic Chemistry 22 (2018): 1697–1703.
- 69D. Wang, L. Ho, J. Faith, et al., “Role of Intestinal Microbiota in the Generation of Polyphenol-Derived Phenolic Acid Mediated Attenuation of Alzheimer's Disease Ss-amyloid Oligomerization,” Molecular Nutrition & Food Research 59 (2015): 1025–1040.
- 70K. Sugimoto, K. Tamura, N. Ohta, et al., “Synthesis of Dihydrofuran-fused Perhydrophenanthrenes Having a Phenolic Hydroxyl Group as a Novel Anti-Alzheimer's Disease Agent,” Bioorganic & Medicinal Chemistry Letters 22 (2012): 449–452.
- 71S.-W. Wang, S.-G. Yang, W. Liu, et al., “Alpha-Tocopherol Quinine Ameliorates Spatial Memory Deficits by Reducing Beta-Amyloid Oligomers, Neuroinflammation and Oxidative Stress in Transgenic Mice with Alzheimer's Disease,” Behavioural Brain Research 296 (2016): 109–117.
- 72M. Qu, Z. Jiang, Y. Liao, Z. Song, and X. Nan, “Lycopene Prevents Amyloid [Beta]-Induced Mitochondrial Oxidative Stress and Dysfunctions in Cultured Rat Cortical Neurons,” Neurochemical Research 41 (2016): 1354–1364.
- 73H. Man and W. Bi, “Protective Effect of Lycopene in a Mouse Model of Parkinson's Disease via Reducing Oxidative Stress and Apoptosis,” Anal Quant Cytopathol Histopathol 40 (2018): 253–258.
- 74A. Babazadeh, B. Ghanbarzadeh, and H. Hamishehkar, “Formulation of Food Grade Nanostructured Lipid Carrier (NLC) for Potential Applications in Medicinal-Functional Foods,” Journal of Drug Delivery Science and Technology 39 (2017): 50–58.
- 75A. Singh and S. Maheshwari, “Dendrimers for Neuro Targeting,” International Journal of Pharma Professional's Research (IJPPR) 14 (2023): 124.
10.48165/ijppronline.2023.14111 Google Scholar
- 76S. Maheshwari and A. Singh, “Navigating the Dementia Landscape: Biomarkers and Emerging Therapies,” Ageing Research Reviews 94 (2024): 102193.
- 77J. A. Loureiro, S. Andrade, A. Duarte, et al., “Resveratrol and Grape Extract-Loaded Solid Lipid Nanoparticles for the Treatment of Alzheimer's Disease,” Molecules (Basel, Switzerland) 22 (2017): 277.
- 78A. Cano, M. Ettcheto, J.-H. Chang, et al., “Dual-Drug Loaded Nanoparticles of Epigallocatechin-3-Gallate (EGCG)/Ascorbic Acid Enhance Therapeutic Efficacy of EGCG in a APPswe/PS1dE9 Alzheimer's Disease Mice Model,” Journal of Controlled Release 301 (2019): 62–75.
- 79Y.-C. Kuo, I.-Y. Chen, and R. Rajesh, “Use of Functionalized Liposomes Loaded With Antioxidants to Permeate the Blood–Brain Barrier and Inhibit β-amyloid-induced Neurodegeneration in the Brain,” Journal of the Taiwan Institute of Chemical Engineers 87 (2018): 1–14.
- 80P. A. Patel, S. C. Patil, D. R. Kalaria, Y. N. Kalia, and V. B. Patravale, “Comparative In Vitro and In Vivo Evaluation of Lipid Based Nanocarriers of Huperzine A,” International Journal of Pharmaceutics 446 (2013): 16–23.
- 81S. Misra, V. Tiwari, A. Kuhad, and K. Chopra, “Modulation of Nitrergic Pathway by Sesamol Prevents Cognitive Deficits and Associated Biochemical Alterations in Intracerebroventricular Streptozotocin Administered Rats,” European Journal of Pharmacology 659 (2011): 177–186.
- 82S. Md, S. Y. Gan, Y. H. Haw, C. L. Ho, S. Wong, and H. Choudhury, “In Vitro Neuroprotective Effects of Naringenin Nanoemulsion against β-Amyloid Toxicity Through the Regulation of Amyloidogenesis and Tau Phosphorylation,” International Journal of Biological Macromolecules 118 (2018): 1211–1219.
- 83T. Ali, M. J. Kim, S. U. Rehman, A. Ahmad, and M. O. Kim, “Anthocyanin-Loaded PEG-Gold Nanoparticles Enhanced the Neuroprotection of Anthocyanins in an Aβ1–42 Mouse Model of Alzheimer's Disease,” Molecular Neurobiology 54 (2017): 6490–6506.
- 84S. Q. Zhang, D. Obregon, J. Ehrhart, et al., “Baicalein Reduces β-Amyloid and Promotes Nonamyloidogenic Amyloid Precursor Protein Processing in an Alzheimer's Disease Transgenic Mouse Model,” Journal of Neuroscience Research 91 (2013): 1239–1246.
- 85R. Kumar and R. Garg, “Bacoside Rich Extract Loaded Solid Lipid Nanoparticles for Alzheimer's Disease,” Plant Archives 20 (2020): 247–252.
- 86S. Saini, T. Sharma, A. Jain, H. Kaur, O. Katare, and B. Singh, “Systematically Designed Chitosan-Coated Solid Lipid Nanoparticles of Ferulic Acid for Effective Management of Alzheimer's Disease: A Preclinical Evidence,” Colloids and Surfaces B: Biointerfaces 205 (2021): 111838.
- 87M. Singh, V. Thakur, R. Deshmukh, et al., “Development and Characterization of Morin Hydrate-Loaded Micellar Nanocarriers for the Effective Management of Alzheimer's Disease,” Journal of Microencapsulation 35 (2018): 137–148.
- 88S. Lohan, K. Raza, S. Mehta, G. K. Bhatti, S. Saini, and B. Singh, “Anti-Alzheimer's Potential of Berberine Using Surface Decorated Multi-Walled Carbon Nanotubes: A Preclinical Evidence,” International Journal of Pharmaceutics 530 (2017): 263–278.
- 89Y. S. Elnaggar, S. M. Etman, D. A. Abdelmonsif, and O. Y. Abdallah, “Intranasal Piperine-Loaded Chitosan Nanoparticles as Brain-Targeted Therapy in Alzheimer's Disease: Optimization, Biological Efficacy, and Potential Toxicity,” Journal of Pharmaceutical Sciences 104 (2015): 3544–3556.
- 90M. Esteves, A. C. Cristóvão, T. Saraiva, et al., “Retinoic Acid-Loaded Polymeric Nanoparticles Induce Neuroprotection in a Mouse Model for Parkinson's Disease,” Frontiers in Aging Neuroscience 7 (2015): 20.
- 91A. H. Moghaddam and M. Zare, “Neuroprotective Effect of Hesperetin and Nano-Hesperetin on Recognition Memory Impairment and the Elevated Oxygen Stress in Rat Model of Alzheimer's Disease,” Biomedicine & Pharmacotherapy 97 (2018): 1096–1101.
- 92K. Ono, K. Hasegawa, H. Naiki, and M. Yamada, “Anti-Amyloidogenic Activity of Tannic Acid and Its Activity to Destabilize Alzheimer's β-Amyloid Fibrils In Vitro,” Biochimica Et Biophysica Acta (BBA)-Molecular Basis of Disease 1690 (2004): 193–202.
- 93Y. Jin, J. Wen, S. Garg, et al., “Development of a Novel Niosomal System for Oral Delivery of Ginkgo Biloba Extract,” International Journal of Nanomedicine (2013): 421–430.
- 94A. Vedagiri and S. Thangarajan, “Mitigating Effect of Chrysin Loaded Solid Lipid Nanoparticles Against Amyloid β25–35 Induced Oxidative Stress in Rat Hippocampal Region: An Efficient Formulation Approach for Alzheimer's Disease,” Neuropeptides 58 (2016): 111–125.
- 95A. A. Moghaddam, M. Aqil, F. J. Ahmad, M. M. Ali, Y. Sultana, and A. Ali, “Nanoethosomes Mediated Transdermal Delivery of Vinpocetine for Management of Alzheimer's Disease,” Drug Delivery 22 (2015): 1018–1026.
- 96J. Zhang, R. Liu, D. Zhang, et al., “Neuroprotective Effects of Maize Tetrapeptide-Anchored Gold Nanoparticles in Alzheimer's Disease,” Colloids and Surfaces B: Biointerfaces 200 (2021): 111584.
- 97S. Madhu, M. Komala, and P. Pandian, “Formulation Development and Characterization of Withaferin-A Loaded Polymeric Nanoparticles for Alzheimer's Disease,” BioNanoScience 11 (2021): 559–566.
- 98M. Agrawal, S. Saraf, S. Saraf, et al., “Recent Advancements in the Field of Nanotechnology for the Delivery of Anti-Alzheimer Drug in the Brain Region,” Expert Opinion on Drug Delivery 15 (2018): 589–617.
- 99C. J. L. Murray, A. D. Lopez, and World Health Organization. Global Comparative Assessments in the Health Sector: Disease Burden, Expenditures and Intervention Packages, ed. C. J. L. Murray and A. D. Lopez (World Health Organization, 1994), https://iris.who.int/handle/10665/41177.
- 100T. Finkel and N. J. Holbrook, “Oxidants, Oxidative Stress and the Biology of Ageing,” Nature 408 (2000): 239–247.
- 101J. Lee, H. Y. Kim, H. Zhou, et al., “Green Synthesis of Phytochemical-Stabilized Au Nanoparticles Under Ambient Conditions and Their Biocompatibility and Antioxidative Activity,” Journal of Materials Chemistry 21 (2011): 13316.
- 102A. R. Rezai, P.-F. D'Haese, V. Finomore, et al., “Ultrasound Blood–Brain Barrier Opening and Aducanumab in Alzheimer's Disease,” New England Journal of Medicine 390 (2024): 55–62.
- 103M. S. Haney, R. Pálovics, C. N. Munson, et al., “Author Correction: An Atlas of Epithelial Cell States and Plasticity in Lung Adenocarcinoma,” Nature 628 (2024): E1.
- 104G. M. Cole, G. P. Lim, F. Yang, et al., “Prevention of Alzheimer's Disease: Omega-3 Fatty Acid and Phenolic Anti-Oxidant Interventions,” Neurobiology of Aging 26 (2005): 133–136.
- 105B. M. Tijms, E. M. Vromen, O. Mjaavatten, et al., “Cerebrospinal Fluid Proteomics in Patients With Alzheimer's Disease Reveals Five Molecular Subtypes With Distinct Genetic Risk Profiles,” Nat Aging 4 (2024): 33–47, https://doi.org/10.1038/s43587-023-00550-7.
- 106S. Abuhamdah, R. Abuhamdah, M.-J. R. Howes, S. Al-Olimat, A. Ennaceur, and P. L. Chazot, “Pharmacological and Neuroprotective Profile of an Essential Oil Derived From Leaves of Aloysia Citrodora Palau,” Journal of Pharmacy and Pharmacology 67 (2015): 1306–1315.
- 107S. Maheshwari, “AGEs RAGE Pathways: Alzheimer's Disease,” Drug Research 73, no. 5 (2023): 251–254.
- 108M. Agrawal, D. K. T. Ajazuddin , S. Saraf, et al., “Recent Advancements in Liposomes Targeting Strategies to Cross Blood-Brain Barrier (BBB) for the Treatment of Alzheimer's Disease,” Journal of Controlled Release 260 (2017): 61–77.
- 109N. Curtis, “To ChatGPT or Not to ChatGPT? The Impact of Artificial Intelligence on Academic Publishing,” Pediatric Infectious Disease Journal 42 (2023): 275.
- 110S. A. Syed Mortadza, J. A. Sim, V. E. Neubrand, and L. H. Jiang, “A Critical Role of TRPM2 Channel in Aβ 42 -Induced Microglial Activation and Generation of Tumor Necrosis Factor-α,” Glia 66 (2018): 562–575.
- 111S. Fan, Y. Zheng, X. Liu, et al., “Curcumin-Loaded PLGA-PEG Nanoparticles Conjugated With B6 Peptide for Potential Use in Alzheimer's Disease,” Drug Delivery 25 (2018): 1091–1102.
- 112X. Huo, Y. Zhang, X. Jin, Y. Li, and L. Zhang, “A Novel Synthesis of Selenium Nanoparticles Encapsulated PLGA Nanospheres With Curcumin Molecules for the Inhibition of Amyloid β Aggregation in Alzheimer's Disease,” Journal of Photochemistry and Photobiology B: Biology 190 (2019): 98–102.
- 113A. Sanz-Alcázar, E. Britti, F. Delaspre, et al., “Mitochondrial Impairment, Decreased Sirtuin Activity and Protein Acetylation in Dorsal Root Ganglia in Friedreich Ataxia Models,” Cellular and Molecular Life Sciences 81 (2024): 12.
- 114S. Shandilya and J. Ruokolainen, “Modulating Effects of Vitamin K2 on Oxidative Stress Induced Organelle Damage in Alzheimer's Disease,” Alzheimer's Dement 19 (2023): e078731, https://doi.org/10.1002/alz.078731.
10.1002/alz.078731 Google Scholar
- 115R. Patel, S. Singh, S. Singh, N. Sheth, and R. Gendle, “Development and Characterization of Curcumin Loaded Transfersome for Transdermal Delivery,” Journal of Pharmaceutical Sciences and Research 4 (2009): 71–80.
- 116A. Singh, V. A. Ansari, T. Mahmood, et al., “Emerging Nanotechnology for the Treatment of Alzheimer's Disease,” CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders) 23 (2024): 687–696.
- 117A. Singh, V. A. Ansari, T. M. Ansari, et al., “Consequence of Dementia and Cognitive Impairment by Primary Nucleation Pathway,” Hormone and Metabolic Research 55 (2023): 304–314.
- 118I. Allaman, M. Bélanger, and P. J. Magistretti, “Astrocyte–Neuron Metabolic Relationships: For Better and for Worse,” Trends in Neuroscience (Tins) 34 (2011): 76–87.
- 119S. Singh, W. Chunglok, O. F. Nwabor, Y. V. Ushir, S. Singh, and W. Panpipat, “Hydrophilic Biopolymer Matrix Antibacterial Peel-Off Facial Mask Functionalized With Biogenic Nanostructured Material for Cosmeceutical Applications,” Journal of Polymers and the Environment 30 (2022): 938–953.
- 120S.-Y. Lim and C. Klein, “Parkinson's Disease Is Predominantly a Genetic Disease,” Journal of Parkinson's Disease 14, no. 3 (2024): 467–482, https://doi.org/10.3233/JPD-230376.
- 121R. Mohseni, Z. ArabSadeghabadi, N. Ziamajidi, R. Abbasalipourkabir, and A. RezaeiFarimani, “Oral Administration of Resveratrol-Loaded Solid Lipid Nanoparticle Improves Insulin Resistance Through Targeting Expression of SNARE Proteins in Adipose and Muscle Tissue in Rats With Type 2 Diabetes,” Nanoscale Research Letters 14 (2019): 227.
- 122B. R. Bloem, M. S. Okun, and C. Klein, “Parkinson's Disease,” Lancet 397 (2021): 2284–2303.
- 123U. Rüb, K. Seidel, H. Heinsen, J. Vonsattel, W. Den Dunnen, and H. Korf, “Huntington's Disease (HD): The Neuropathology of a Multisystem Neurodegenerative Disorder of the Human Brain,” Brain Pathology 26 (2016): 726–740.
- 124P. Aramwit, K. Fongsodsri, K. Tuentam, et al., “Sericin Coated Thin Polymeric Films Reduce Keratinocyte Proliferation via the mTOR Pathway and Epidermal Inflammation Through IL17 Signaling in Psoriasis Rat Model,” Scientific Reports 13 (2023): 12133.
- 125W. Wang, T. Chen, H. Xu, et al., “Curcumin-Loaded Solid Lipid Nanoparticles Enhanced Anticancer Efficiency in Breast Cancer,” Molecules (Basel, Switzerland) 23 (2018): 1578.
- 126K. Kieburtz, R. Reilmann, and C. W. Olanow, “Huntington's Disease: Current and Future Therapeutic Prospects,” Movement Disorders 33 (2018): 1033–1041.
- 127V. Kakkar, S. K. Muppu, K. Chopra, and I. P. Kaur, “Curcumin Loaded Solid Lipid Nanoparticles: An Efficient Formulation Approach for Cerebral Ischemic Reperfusion Injury in Rats,” European Journal of Pharmaceutics and Biopharmaceutics 85 (2013): 339–345.
- 128E. L. Feldman, S. A. Goutman, S. Petri, et al., “Amyotrophic Lateral Sclerosis,” Lancet 400 (2022): 1363–1380.
- 129O. Hardiman, A. Al-Chalabi, A. Chio, et al., “Amyotrophic Lateral Sclerosis,” Simmons and L H Van Den Berg, Nature Reviews Disease Primers 3, no. 1 (2017): 1–19.
- 130C. R. Vintilescu, S. Afreen, A. E. Rubino, and A. Ferreira, “The Neurotoxic Tau45-230 Fragment Accumulates in Upper and Lower Motor Neurons in Amyotrophic Lateral Sclerosis Subjects,” Molecular Medicine 22 (2016): 477–486.
- 131M. A. Van Es, O. Hardiman, A. Chio, et al., “Amyotrophic Lateral Sclerosis,” Lancet 390 (2017): 2084–2098.
- 132F. Sarubbo, S. Esteban, A. Miralles, and D. Moranta, “Effects of Resveratrol and Other Polyphenols on Sirt1: Relevance to Brain Function During Aging,” Current Neuropharmacology 16 (2018): 126–136.
- 133D. Bian, M. Liu, Y. Li, Y. Xia, Z. Gong, and Y. Dai, “Madecassoside, a Triterpenoid Saponin Isolated From Centella Asiatica Herbs, Protects Endothelial Cells Against Oxidative Stress,” Journal of Biochemical and Molecular Toxicology 26 (2012): 399–406.
- 134Q. Chen, Q. Qian, H. Xu, et al., “Mitochondrial-Targeted Metal-Phenolic Nanoparticles to Attenuate Intervertebral Disc Degeneration: Alleviating Oxidative Stress and Mitochondrial Dysfunction,” ACS Nano 18 (2024): 8885–8905.
- 135L. J. Valotto Neto, M. Reverete de Araujo, R. C. Moretti Junior, et al., “Investigating the Neuroprotective and Cognitive-Enhancing Effects of Bacopa monnieri: A Systematic Review Focused on Inflammation, Oxidative Stress, Mitochondrial Dysfunction, and Apoptosis,” Antioxidants 13 (2024): 393.
- 136J. L. F. de la Paz, P. de Jesús Martínez-Morales, E. Calderón-Cortés, et al., “Avocado Oil Increases Cell Viability and Respiratory Rate of Yeast During Oxidative Stress Induced by Ferrous Iron,” Faseb Journal 26 (2012): 611.8–611.8.
10.1096/fasebj.26.1_supplement.611.8 Google Scholar
- 137Z.-J. Yang, C.-L. Zhao, W.-Q. Liang, Z.-R. Chen, Z.-D. Du, and S.-S. Gong, “ROS-Induced Oxidative Stress and Mitochondrial Dysfunction: A Possible Mechanism Responsible for Noise-Induced Ribbon Synaptic Damage,” American Journal of Translational Research 16 (2024): 272–284.
- 138S. Heales, J. Land, and S. Pope, “S7/3 Oxidative Stress and Mitochondrial Dysfunction,” BBA-Bioenergetics 1777 (2008): S45.
10.1016/j.bbabio.2008.05.180 Google Scholar
- 139S. G. Younkin, “The Role of Aβ42 in Alzheimer's Disease,” Journal of Physiology-Paris 92 (1998): 289–292.
- 140J. Sørensen, “Reduction of Ferric Iron in Anaerobic, Marine Sediment and Interaction With Reduction of Nitrate and Sulfate,” Applied and Environmental Microbiology 43 (1982): 319–324.
- 141S. Oshiro, M. S. Morioka, and M. Kikuchi, “Dysregulation of Iron Metabolism in Alzheimer' s Disease, Parkinson' s Disease, and Amyotrophic Lateral Sclerosis,” Advances in Pharmacological and Pharmaceutical Sciences 1 (2011): 378278.
- 142S. Altamura and M. U. Muckenthaler, “Iron Toxicity in Diseases of Aging: Alzheimer's Disease, Parkinson's Disease and Atherosclerosis,” Journal of Alzheimer's Disease 16 (2009): 879–895.
- 143S. Maheshwari, “Ferroptosis Signaling Pathways: Alzheimer's Disease,” Hormone and Metabolic Research 55, no. 12 (2023): 819–826.
- 144S. Jin, P.-S. Liu, D. Zheng, and X. Xie, “The Interplay of miRNAs and Ferroptosis in Diseases Related to Iron Overload,” Apoptosis 29 (2024): 45–65.
- 145J. Y. Cao and S. J. Dixon, “Mechanisms of Ferroptosis,” Cellular and Molecular Life Sciences 73 (2016): 2195–2209.
- 146A. Kumar, T. J. Jayeoye, P. Mohite, et al., “Sustainable and Consumer-centric Nanotechnology-Based Materials: An Update on the Multifaceted Applications, Risks and Tremendous Opportunities,” Nano-Structures & Nano-Objects 38 (2024): 101148.
10.1016/j.nanoso.2024.101148 Google Scholar
- 147P. Corcia, C. Tauber, J. Vercoullie, et al., “Molecular Imaging of Microglial Activation in Amyotrophic Lateral Sclerosis,” PLoS ONE 7 (2012): e52941.
- 148F. A. Cupaioli, F. A. Zucca, D. Boraschi, and L. Zecca, “Engineered Nanoparticles. How Brain Friendly Is this New Guest?,” Progress in Neurobiology 119–120 (2014): 20–38.
- 149J. Dernedde, A. Rausch, M. Weinhart, et al., “Dendritic Polyglycerol Sulfates as Multivalent Inhibitors of Inflammation,” Proceedings of the National Academy of Sciences of the United States of America 107 (2010): 19679–19684.
- 150A. P. Dias, S. da Silva Santos, J. V. da Silva, et al., “Dendrimers in the Context of Nanomedicine,” International Journal of Pharmaceutics 573 (2020): 118814.
- 151D. J. DiSabato, N. Quan, and J. P. Godbout, “Neuroinflammation: The Devil Is in the Details,” Journal of Neurochemistry 139, no. S2 (2016): 136–153.
- 152N. D. Santos Tramontin, S. da Silva, R. Arruda, et al., “Gold Nanoparticles Treatment Reverses Brain Damage in Alzheimer's Disease Model,” Molecular Neurobiology 57 (2020): 926–936.
- 153S. Sudarshan, R. D. Tanvi, D. Rajesh, V. U. Yogesh, and W. Slamet, Lipid Nanoparticulate Drug Delivery Systems: Approaches Toward Improvement in Therapeutic Efficacy of Bioactive Molecules, ed. V.-G. Luis Jesús (IntechOpen, 2022).
- 154D. U. Kapoor, M. Gaur, A. Parihar, B. G. Prajapati, S. Singh, and R. J. Patel, “Phosphatidylcholine (PCL) Fortified Nano-phytopharmaceuticals for Improvement of Therapeutic Efficacy,” EXCLI journal 22 (2023): 880.
- 155B. N. Dugger and D. W. Dickson, “Pathology of Neurodegenerative Diseases,” Cold Spring Harbor Perspectives in Biology 9, no. 7 (2017): a028035.
- 156S. Maheshwari, R. K. Tiwari, and L. Singh, “Green Expertise: Synthesis of Silver Nanoparticles for Wound Healing Application an Overview,” Research Journal of Pharmacy and Technology 14 (2021): 1149–1154.
10.5958/0974-360X.2021.00206.7 Google Scholar
- 157S. Maheshwari, “Synergistic Effects of Woodfordia Fruticosa Silver Nanoparticles Accelerating Wound Healing in Swiss Mice In Vivo,” Intelligent Pharmacy 2 (2024): 17–27.
10.1016/j.ipha.2023.09.005 Google Scholar
- 158S. U. Islam, A. Shehzad, M. B. Ahmed, and Y. S. Lee, “Intranasal Delivery of Nanoformulations: A Potential Way of Treatment for Neurological Disorders,” Molecules (Basel, Switzerland) 8 (2020): 1929.
10.3390/molecules25081929 Google Scholar
- 159J. Wang, H. Wang, R. Zhu, Q. Liu, J. Fei, and S. Wang, “Anti-Inflammatory Activity of Curcumin-Loaded Solid Lipid Nanoparticles in IL-1β Transgenic Mice Subjected to the Lipopolysaccharide-Induced Sepsis,” Biomaterials 53 (2015): 475–483.
- 160B. F. Far, M. Safaei, A. Pourmolaei, et al., “Exploring Curcumin-Loaded Lipid-Based Nanomedicine as Efficient Targeted Therapy for Alzheimer's Diseases,” ACS Applied Bio Materials 7 (2024): 3535–3555.
- 161N. Clemente, B. Ferrara, C. L. Gigliotti, et al., “Solid Lipid Nanoparticles Carrying Temozolomide for Melanoma Treatment. Preliminary In Vitro and In Vivo Studies,” International Journal of Molecular Sciences 19 (2018): 255.
- 162V. P. Chavda, P. C. Balar, R. Bezbaruah, et al., “Nanoemulsions: Summary of a Decade of Research and Recent Advances,” Nanomedicine 19 (2024): 519–536.
- 163N. Huang, S. Lu, X.-G. Liu, J. Zhu, Y.-J. Wang, and R.-T. Liu, “PLGA Nanoparticles Modified With a BBB-penetrating Peptide Co-Delivering Aβ Generation Inhibitor and Curcumin Attenuate Memory Deficits and Neuropathology in Alzheimer's Disease Mice,” Oncotarget 46 (2017): 81001.
10.18632/oncotarget.20944 Google Scholar
- 164A. Cano, M. Ettcheto, M. Espina, et al., “Epigallocatechin-3-Gallate Loaded PEGylated-PLGA Nanoparticles: A New Anti-Seizure Strategy for Temporal Lobe Epilepsy,” Nanomedicine: Nanotechnology, Biology and Medicine 14 (2018): 1073–1085.
- 165G. C. Lavorato, J. C. Azcárate, M. B. R. Aiello, et al., “Hydrophilization of Magnetic Nanoparticles With an Amphiphilic Polymer Revisited: Roles of Nanoparticle Capping Density and Polymer Structure,” Applied Surface Science 570 (2021): 151171.
- 166C. Modi, B. G. Prajapati, S. Singh, A. Singh, and S. Maheshwari, “ Chapter 14—Dendrimers in the Management of Alzheimer's Disease,” in Alzheimer's Disease and Advanced Drug Delivery Strategies, ed. B. G. Prajapati, D. K. Chellappan, and P. N. Kendre (Academic Press, 2024), 235–251.
10.1016/B978-0-443-13205-6.00028-5 Google Scholar
- 167D. Maysinger, J. Ji, A. Moquin, et al., “Dendritic Polyglycerol Sulfates in the Prevention of Synaptic Loss and Mechanism of Action on Glia,” ACS Chemical Neuroscience 9 (2018): 260–271.
- 168A. Singh, V. A. Ansari, T. Mahmood, F. Ahsan, and R. Wasim, “Dendrimers: A Neuroprotective Lead in Alzheimer Disease: A Review on Its Synthetic Approach and Applications,” Drug Research 72 (2022): 417–423.
- 169P. Kesharwani, K. Jain, and N. K. Jain, “Dendrimer as Nanocarrier for Drug Delivery,” Progress in Polymer Science 39 (2014): 268–307.
- 170J. Li, M. Darabi, J. Gu, et al., “A Drug Delivery Hydrogel System Based on Activin B for Parkinson's Disease,” Biomaterials 102 (2016): 72–86.
- 171S. Bhattacharya, B. G. Prajapati, and S. Singh, “A Critical Review on the Dissemination of PH and Stimuli-Responsive Polymeric Nanoparticular Systems to Improve Drug Delivery in Cancer Therapy,” Critical Reviews in Oncology/Hematology 185 (2023): 103961.
- 172Y. Fan, M. Lüchow, Y. Zhang, et al., “Nanogel Encapsulated Hydrogels as Advanced Wound Dressings for the Controlled Delivery of Antibiotics,” Advanced Functional Materials 31 (2021): 2006453.
- 173H. Zhu, L. Kong, X. Zhu, T. Ran, and X. Ji, “pH-Responsive Nanoparticles for Delivery of Paclitaxel to the Injury Site for Inhibiting Vascular Restenosis,” Pharmaceutics 14 (2022): 535.
- 174T. J. Jayeoye, E. F. Nwude, S. Singh, B. G. Prajapati, D. U. Kapoor, and N. Muangsi, “Sustainable Synthesis of Gold Nanoparticles for Drug Delivery and Cosmeceutical Applications: A Review,” BioNanoScience 14 (2024): 3355–3384.
- 175D. A. Giljohann, D. S. Seferos, W. L. Daniel, M. D. Massich, P. C. Patel, and C. A. Mirkin, “ Gold Nanoparticles for Biology and Medicine,” in Spherical Nucleic Acid, ed. C. A. Mirkin (Jenny Stanford Publishing, 2020), 36.
- 176P. C. Chen, S. C. Mwakwari, and A. K. Oyelere, “Gold Nanoparticles: From Nanomedicine to Nanosensing,” Nanotechnology, Science and Applications 1 (2008): 45–65.
- 177A. Ali, H. Zafar, M. Zia, et al., “Synthesis, Characterization, Applications, and Challenges of Iron Oxide Nanoparticles,” Nanotechnology, Science and Applications (2016): 49–67.
- 178A. H. Karim, A. Ali, and S. Mezan, “Synthesis and Characterization of Silica Nanoparticle (Sio2 Nps) via Chemical Process,” Annals of the Romanian Society for Cell Biology 25 (2021): 6211.
- 179W. Pan, H.-J. Zhang, Y.-F. Zhang, et al., “Silica Nanoparticle Accumulation in Plants: Current state and Future Perspectives,” Nanoscale 15 (2023): 15079–15091.
- 180A. Malhan, M. Guleria, U. Das, et al., “Navigating the Future of Cancer Management Through Carbon Nanodots: A Review,” Nano-Structures & Nano-Objects 39 (2024): 101217.
- 181H. Choi, B. Min, J. Shin, and D. Bae, “Strengthening in Nanostructured 2024 Aluminum Alloy and Its Composites Containing Carbon Nanotubes,” Composites Part A: Applied Science and Manufacturing 42 (2011): 1438–1444.
- 182G. Perini, V. Palmieri, G. Ciasca, M. De Spirito, and M. Papi, “Unravelling the Potential of Graphene Quantum Dots in Biomedicine and Neuroscience,” International Journal of Molecular Sciences 21 (2020): 3712.
- 183G. Perini, V. Palmieri, G. Ciasca, et al., “Enhanced Chemotherapy for Glioblastoma Multiforme Mediated by Functionalized Graphene Quantum Dots,” Materials 13 (2020): 4139.
- 184D. Huh, G. A. Hamilton, and D. E. Ingber, “From 3D Cell Culture to Organs-on-Chips,” Trends in Cell Biology 21 (2011): 745–754.
- 185F. Cheng, W. Li, Y. Zhou, et al., “admetSAR: A Comprehensive Source and Free Tool for Assessment of Chemical ADMET Properties,” Journal of Chemical Information and Modeling 52 (2012): 3099–3105.
- 186S. K. Verma, A. Nandi, F. Z. Simnani, et al., “In Silico Nanotoxicology: The Computational Biology state of Art for Nanomaterial Safety Assessments,” Materials & Design 235 (2023): 112452.
- 187A. Cano, P. Turowski, M. Ettcheto, et al., “Nanomedicine-Based Technologies and Novel Biomarkers for the Diagnosis and Treatment of Alzheimer's Disease: From Current to Future Challenges,” Journal of Nanobiotechnology 19 (2021): 122.
- 188M. Agrawal, S. Saraf, M. Pradhan, et al., “Design and Optimization of Curcumin Loaded Nano Lipid Carrier System Using Box-Behnken Design,” Biomedicine & Pharmacotherapy 141 (2021): 111919.
- 189C. Moulton, A. Baroni, E. Quagliarini, et al., “Navigating the Nano-bio Immune Interface: Advancements and Challenges in CNS Nanotherapeutics,” Frontiers in Immunology 15 (2024).
- 190S. Ashique, O. Afzal, S. Yasmin, et al., “Strategic Nanocarriers to Control Neurodegenerative Disorders: Concept, Challenges, and Future Perspective,” International Journal of Pharmaceutics 633 (2023): 122614.
- 191M. Martínez-Ballesta, Á. Gil-Izquierdo, C. García-Viguera, and R. Domínguez-Perles, “Nanoparticles and Controlled Delivery for Bioactive Compounds: Outlining Challenges for New “Smart-Foods” for Health,” Foods 7 (2018): 72.
- 192S. M. Petrovic and M.-E. Barbinta-Patrascu, “Organic and Biogenic Nanocarriers as Bio-Friendly Systems for Bioactive Compounds' Delivery: State-of-the Art and Challenges,” Materials 16 (2023): 7550.
- 193M. Atabakhshi-Kashi, M. Geranpayehvaghei, Y. Wang, et al., “Recent Advances of Nanocarriers for Effective Delivery of Therapeutic Peptides,” Precision Nanomedicine 3 (2020): 549–576.
10.33218/001c.13444 Google Scholar
- 194H. Le, C. Karakasyan, T. Jouenne, D. Le Cerf, and E. Dé, “Application of Polymeric Nanocarriers for Enhancing the Bioavailability of Antibiotics at the Target Site and Overcoming Antimicrobial Resistance,” Applied Sciences 11 (2021): 10695.
- 195R. Sandhir, A. Yadav, A. Sunkaria, and N. Singhal, “Nano-Antioxidants: An Emerging Strategy for Intervention Against Neurodegenerative Conditions,” Neurochemistry International 89 (2015): 209–226.
- 196T. B. Soares, L. Loureiro, A. Carvalho, et al., “Lipid Nanocarriers Loaded With Natural Compounds: Potential New Therapies for Age Related Neurodegenerative Diseases?,” Progress in Neurobiology 168 (2018): 21–41.
- 197D. M. Sima, T. V. Phan, S. Van Eyndhoven, et al., “Artificial Intelligence Assistive Software Tool for Automated Detection and Quantification of Amyloid-Related Imaging Abnormalities,” JAMA Network Open 7 (2024): e2355800.