Bioequivalence of alternative pembrolizumab dosing regimens: current practice and future perspectives
Ruben Malmberg, Bram C. Agema, and Maaike M. Hofman contributed equally to this work.
Abbreviations
-
- ADS
-
- Alternative dosing strategy
-
- PD-1/PD-L1
-
- programmed cell death protein 1/ programmed death-ligand 1
-
- AUC
-
- Area under the curve
-
- Cmax
-
- Maximum concentration
-
- Ctrough,ss
-
- Steady-state trough concentration
-
- FDA
-
- Food and Drug Administration
-
- ICI
-
- Immune checkpoint inhibitor
-
- mAb
-
- monoclonal antibody
-
- NCT
-
- The National Clinical Trial number
-
- NSCLC
-
- Non-small cell lung cancer
-
- Q3W
-
- Three-weekly
-
- Q4W
-
- Four-weekly
-
- Q6W
-
- Six-weekly
-
- RCT
-
- Randomized controlled trial
Immune checkpoint inhibitors (ICIs), including humanized anti-programmed cell death protein 1/programmed death-ligand 1 (anti-PD-1/PD-L1) monoclonal antibodies (mAbs), such as pembrolizumab, have transformed cancer treatment. Pembrolizumab was initially approved as a three-weekly (Q3W) 2 mg/kg weight-based dose by the Food and Drug Administration (FDA), which was later replaced by a 200 mg Q3W fixed-dose, mainly based on in silico simulations. Later, a fixed 400 mg six-weekly (Q6W) regimen was approved based on pharmacokinetic simulations [1].
Due to increasing ICI use and high costs per treatment, increasingly large portions of healthcare budgets are shifted to ICI treatment. Therefore, it is important to handle ICIs as efficiently and cost-effectively as possible. Hence, the Q6W regimen was introduced, lowering the total amount of ICI administrations per patient and the strain on healthcare capacity, and improving patient convenience. The cost-effectiveness of ICI treatment could be optimized further by using alternative dosing strategies (ADS) [1]. Some of these ADS have already been tested for pembrolizumab in some countries [2, 3].
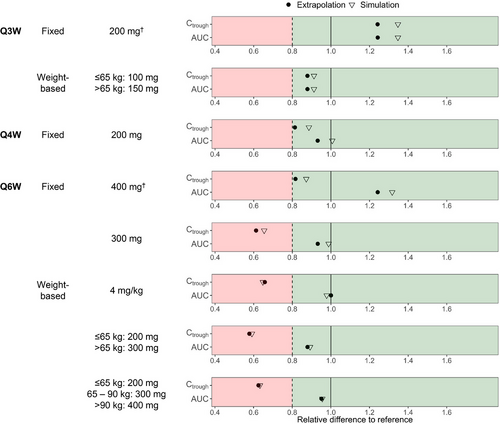
Recently, the FDA provided bioequivalence guidelines for ADS, specifically for anti-PD-1/PD-L1 mAbs [4]. These guidelines support the use of pharmacokinetic-modeling to simulate steady-state trough concentrations (Ctrough,ss) and area under the curve (AUC; exposure) to establish bioequivalence for anti-PD-1/PD-L1 mAbs. In these guidelines, ADS are considered bioequivalent when both Ctrough,ss and exposure are at most 20% lower compared to the dosing regimen used while establishing efficacy in clinical trials (i.e. the reference dosing regimen). A maximum of 25% increase in the maximum concentration (Cmax) is used as the upper boundary, unless adequate clinical evidence shows that increasing the Cmax does not increase toxicity. For pembrolizumab, incidences of toxicities were generally consistent across a 2-10 mg/kg dose range in multiple trials [5].
To verify whether various ADS (Figure 1, Supplementary Table S1) are bioequivalent following the current FDA guidelines, we assessed bioequivalence using pharmacokinetic modelling. Using pharmacokinetic data from a real-world cohort, the best performing model was selected with which bioequivalence was assessed in extrapolations from this cohort (“extrapolation”) and also from a virtual (“simulation”) cohort. Details on both cohorts, as well as modelling procedures, are depicted in the Supplementary Material and Methods. As a reference, the Q3W 2 mg/kg dosing regimen was used, as this regimen was used in the original approval. Results of these analyses are shown in Figure 1. The simulated ADS for pembrolizumab given every 3 or 4 weeks (Q3/4W) were bioequivalent according to the FDA guidelines. Interestingly, despite meeting the criteria for exposure, none of the (non-registered) simulated Q6W ADS were bioequivalent, as the criteria for Ctrough,ss were not met.
Pharmacokinetic bioequivalence is usually utilized to ensure equivalent efficacy. However, the applicability of the thresholds proposed in the FDA guidelines could be questioned, as it disregards clinical pharmacological data regarding exposure-response relationships (except for Cmax). Consequently, the implications of non-adherence to the bioequivalence criteria are unclear. To explore the possible implications of non-adherence, we shall examine arguments in favor of and against the FDA-guidelines for bioequivalence of anti-PD-1/PD-L1 mAbs in the next section.
Firstly, the thresholds in these guidelines are derived from bioequivalence guidelines for small molecules. However, anti-PD-1/PD-L1 mAbs do not show similar exposure-response relationships to most small molecules. Therefore, similar anti-PD-1/PD-L1 mAb pharmacokinetics are probably not necessary to ensure similar efficacy. For example, no significant differences in efficacy were observed in a 2-10 mg/kg dose range [5]. Besides, no adequately powered prospective study has validated the FDA criteria for exposure (nor Ctrough,ss) [5]. This is exemplified during the registration of the pembrolizumab 400 mg Q6W dosing regimen [5]. The FDA initially rejected this regimen, as a pharmacokinetic model predicted that 400 mg Q6W was not bioequivalent to the 200 mg Q3W regimen [5]. Nonetheless, conditional approval was granted, based on a limited descriptive interim analysis (n = 44) of objective response rates in a non-randomized cohort, in which the response rates were compared with literature values [5].
Furthermore, clinical pharmacological data suggests that approved pembrolizumab doses are higher than required for maximum efficacy. This may be caused by a focus on the maximum tolerated dose in phase I trials, instead of the lowest maximally effective dose. For instance, it was demonstrated that doses ≥ 0.1 mg/kg result in near-complete (> 95%) receptor occupancy in blood. Early research with nivolumab showed that maximum efficacy is achieved when near-complete receptor occupancy is reached [1, 6]. Nevertheless, only doses ≥ 2 mg/kg were selected for subsequent trials as simulations showed that this would result in near-complete intra-tumoral receptor occupancy after the first administration, which was considered a surrogate marker for maximum efficacy [1]. Two hundred mg Q3W results in a geometric mean of ≥ 10.7 µg/mL after the first dose. Consequently, the approved doses result in a much higher Ctrough,ss than required, which suggests that ADS resulting in Ctrough,ss levels ≥ 10.7 µg/mL (corresponding with a simulated dose of ≥ 0.85 mg/kg Q3W or ≥ 2.58 mg/kg Q6W, Supplementary Material and Methods) would also be maximally effective [7].
It has been reported that lower pembrolizumab exposure is associated with poorer outcomes, suggesting an exposure-response relationship. The post-hoc analyses of the Keynote-002 and Keynote-010 studies have shown however that worse clinical outcomes are associated with increased pembrolizumab clearance [8]. These findings could explain the absence of an exposure-response relationship, illustrated by similar overall survival, in the 2-10 mg/kg dose range despite substantial variation in Ctrough,ss (2 mg/kg Q3W (Ctrough,ss range: 1.13-127 µg/mL) [1, 5]. This underlines that bioequivalent exposure is not always indicative of outcome and could explain the reports of prolonged responses after treatment cessation during phase I-II trials [1].
Clinical evidence from various pembrolizumab trials in different tumor types also support non-bioequivalent doses which are lower than the EMA/FDA approved doses [1]. For instance, a retrospective study in patients with non-small cell lung cancer (NSCLC) found that administration of Q3W-Q6W ADS (n = 604) resulted in comparable overall survival as standard dosing (n = 1,362) [2]. Furthermore, three small Canadian studies retrospectively analyzed cohorts of NSCLC patients treated with 2 mg/kg Q3W and 4 mg/kg Q6W (combined n = 139) and concluded that 4 mg/kg Q6W was equally effective [3].
However, there is uncertainty in measuring receptor occupancy in vivo because this is a complex technical endeavor. Therefore, the intra-tumoral receptor occupancy studies were performed in silico using in vitro data and the developed model has never been validated in vivo. Consequently, its clinical predictive value remains unclear [6]. Moreover, even at near-complete receptor occupancy, attained by the 2 mg/kg dosing regimen under the most optimal conditions, only 15%-50% of patients with solid tumors respond [5, 9]. This indicates that the effectiveness of treatment is not solely dependent on receptor occupancy and pharmacokinetic parameters, suggesting a more complex array of non-pharmacokinetic factors influencing the response, such as tumor type, tumor mutational burden, the ability of T-cells to infiltrate and become activated within tumors, as well as PD-L1 expression and the expression of certain genomic alterations [10].
Randomized controlled trials (RCTs) are the golden standard for determining efficacy and safety of ADS. Currently, multiple studies are being conducted, illustrating the unmet need for ADS (NCT04913025, NCT04295863, NCT05692999, and NCT04909684) (detailed descriptions are depicted in Supplementary Table S2). However, presently, no adequately powered RCT to assess efficacy of doses < 2 mg/kg has been completed yet, as this is time-consuming and expensive.
In conclusion, there are indications that the stipulated FDA criteria are not reflective of the true exposure-response relationship of pembrolizumab, thereby underlining the potential of ADS to improve cost-effectiveness of treatment. However, we still do not fully understand the driving mechanisms of ICI efficacy and the exact threshold for maximum efficacy remains elusive. Consequently, the implications of implementing ADS that are not bioequivalent to the reference dosing regimen in daily practice are not yet fully understood. Nevertheless, lower doses that deviate from bioequivalence criteria may result in exposures below the threshold for maximum efficacy, potentially leading to reduced efficacy. More sophisticated methods are needed to determine the minimum effectivity threshold in a faster way, and provide adequate guidance to support ADS for pembrolizumab. For future dose-optimization studies Tannock et al. [11] suggest moving away from the requirement for non-inferiority trials. Additionally, we recommend initiating ADS studies earlier, preferably prior to market reimbursement, to facilitate faster validation and regulatory acceptance of ADS. Until then, all available pembrolizumab dosing data should be carefully discussed, balanced, and reviewed.
AUTHOR CONTRIBUTIONS
Ruben Malmberg: Methodology; investigation; validation; formal analysis; writing—original draft; writing—review & editing, visualization. Bram C. Agema: Methodology; investigation; validation; formal analysis; writing—original draft; writing—review & editing; visualization. Maaike M. Hofman: Methodology; investigation; validation; formal analysis; writing—original draft; writing—review & editing; visualization. Stefani Oosterveld: Investigation; writing—review & editing. Sander Bins: Methodology; writing—review & editing. Daphne W. Dumoulin: Methodology; writing—review & editing. Arjen Joosse: Methodology; writing—review & editing. Joachim G.J.V Aerts: Methodology; writing—review & editing. Reno Debets: Methodology; writing—review & editing. Birgit C.P. Koch: Methodology; writing—review & editing. Astrid A.M. van der Veldt: Methodology; writing—review & editing. Roelof W.F. van Leeuwen: Conceptualization; methodology; investigation; writing—review & editing. Ron H.J. Mathijssen: Conceptualization; methodology; resources; investigation; writing—review & editing.
ACKNOWLEDGEMENTS
We thank all the health care professionals from the Erasmus MC Cancer Institute in Rotterdam, the Netherlands contributing to the MULTOMAB-study.
CONFLICT OF INTEREST STATEMENT
None of the co-authors have a conflict of interest in relation to the current manuscript. Ruben Malmberg reports speaker fees from Bristol Myers Squibb. Daphne W. Dumoulin reports speaker fees and consultancy fees from Roche, Bristol Myers Squibb, Merck Sharp & Dohme, Astra Zeneca, Pfizer, and Amgen. Joachim G.J.V. Aerts reports grants from Boehringer-Ingelheim, Merck Sharp & Dohme, Bristol Myers Squibb, Astra-Zeneca, Eli-Lilly, Verastem, Nutricia, Amphera, and CureVac (payments to institution and personnel). Fees for lectures: Merck Sharp &Dohme, Astra-Zeneca, and Eli-Lilly. Travel fees: Merck Sharp & Dohme and Astra Zeneca. Patent issued: allogeneic tumor cell lysate, combination immunotherapy. Board of directors’ member for International Association for the Study of Lung Cancer and International Mesothelioma Interest Group. Stock: Amphera. Astrid A.M. van der Veldt reports consultancy fees from Bristol Myers Squibb, Eisai, Ipsen, Merck Sharp & Dohme, Sanofi, Pierre Fabre, Novartis, Pfizer, and Roche (payments to institution). Roelof W.F. van Leeuwen reports research grants from Bristol Myers Squibb and Pfizer. Consulting fees from Bristol Myers Squibb, Pfizer, Pierre-Fabre and Merck Sharp & Dohme. Ron H.J. Mathijssen reports research grants (payments to institution) from Astellas, Bayer, Boehringer-Ingelheim, Cristal Therapeutics, Deuter Oncology, Echo Pharmaceuticals, Nordic Pharma, Novartis, Pamgene, Pfizer, Roche, Sanofi and Servier.
FUNDING INFORMATION
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
This study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the Erasmus Medical Center (METC 16-011). All participants provided written informed consent prior to their inclusion in the study.
Open Research
DATA AVAILABILITY STATEMENT
All data supporting the findings of this study are available within the article and its information files and from the corresponding author upon reasonable request.




