Management of locally advanced non-small cell lung cancer: State of the art and future directions
Da Miao and Jing Zhao contributed equally to this work.
Abstract
Lung cancer is the second most common and the deadliest type of cancer worldwide. Clinically, non-small cell lung cancer (NSCLC) is the most common pathological type of lung cancer; approximately one-third of affected patients have locally advanced NSCLC (LA-NSCLC, stage III NSCLC) at diagnosis. Because of its heterogeneity, LA-NSCLC often requires multidisciplinary assessment. Moreover, the prognosis of affected patients is much below satisfaction, and the efficacy of traditional therapeutic strategies has reached a plateau. With the emergence of targeted therapies and immunotherapies, as well as the continuous development of novel radiotherapies, we have entered an era of novel treatment paradigm for LA-NSCLC. Here, we reviewed the landscape of relevant therapeutic modalities, including adjuvant, neoadjuvant, and perioperative targeted and immune strategies in patients with resectable LA-NSCLC with/without oncogenic alterations; as well as novel combinations of chemoradiation and immunotherapy/targeted therapy in unresectable LA-NSCLC. We addressed the unresolved challenges that remain in the field, and examined future directions to optimize clinical management and increase the cure rate of LA-NSCLC.
List of abbreviations
-
- NSCLC
-
- non-small cell lung cancer
-
- LA-NSCLC
-
- locally advanced-non-small cell lung cancer
-
- OS
-
- overall survival
-
- PORT
-
- postoperative radiotherapy
-
- DFS
-
- disease-free survival
-
- HR
-
- hazard ratio
-
- PD-L1
-
- programmed death-ligand 1
-
- EGFR
-
- epidermal growth factor receptor
-
- ALK
-
- anaplastic lymphoma kinase
-
- mDFS
-
- median disease-free survival
-
- ICI
-
- immune checkpoint inhibitor
-
- mPFS
-
- median progression-free survival
-
- ctDNA
-
- circulating tumor DNA
-
- MRD
-
- minimal residual disease
-
- IMRT
-
- intensity-modulated radiation therapy
-
- CRT
-
- conformal radiation therapy
-
- MPR
-
- major pathological response
-
- pCR
-
- pathological complete response
-
- RFS
-
- recurrence-free survival
-
- IL7R
-
- interleukin-7 receptor
-
- TCF7
-
- transcription factor 7
-
- GZMK
-
- granayme K
-
- TOX2
-
- TOX high mobility group box family member 2
-
- CTLA4
-
- cytotoxic T lymphocyte associate protein 4
-
- HAVCR2
-
- hepatitis A virus cellular receptor 2
-
- ENTPD1
-
- ectonucleoside triphosphate diphosphohydrolase 1
-
- ORR
-
- objective response rate
-
- TRAE
-
- treatment-related adverse event
-
- EFS
-
- event-free survival
-
- mOS
-
- median overall survival
-
- sCRT
-
- sequential chemoradiotherapy
-
- mEFS
-
- median event-free survival
-
- IMPT
-
- intensity-modulated proton therapy
-
- TKI
-
- tyrosine kinase inhibitor
1 BACKGROUND
Lung cancer is the second most prevalent and the deadliest cancer worldwide [1]. In particular, non-small cell lung cancer (NSCLC) causes approximately 85% of all cases of lung cancer, and 30% of affected patients have locally advanced (stage III) disease at diagnosis [2]. Locally advanced-NSCLC (LA-NSCLC) is a highly heterogeneous disease that often displays a complex clinical profile and high tumor burden. Although LA-NSCLC does not metastasize to distant sites, there remains an unmet clinical need to improve the overall prognosis of LA-NSCLC considering its complexity and the limitations of current treatment strategies.
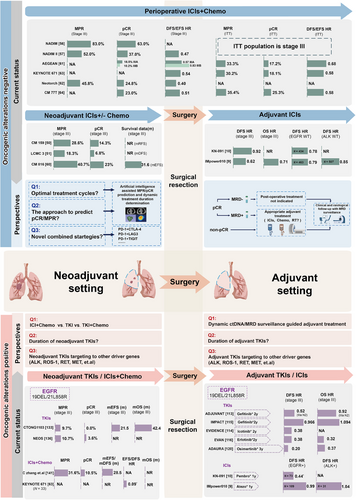
Recent research advances have supported that concurrent or sequential chemoradiotherapy confers a limited survival benefit to patients with stage IIIA, IIIB, and IIIC NSCLC; the 5-year overall survival (OS) rates are 36%, 26%, and 13%, respectively [3]. However, the emergence of enhanced therapeutic strategies for LA-NSCLC (e.g., neoadjuvant therapies, postoperative adjuvant therapies, postoperative adjuvant radiotherapy, immunotherapy maintenance after concurrent chemoradiotherapy [cCRT], and cCRT combined with immunotherapy) provide hope for patients with LA-NSCLC. The availability of multiple new treatment options introduces numerous questions into the clinical decision-making process. For example, it is clear that resectable LA-NSCLC without surgical contraindication should be surgically resected. However, questions arise regarding the subsequent course of treatment: should patients undergo maintenance immunotherapy or is neoadjuvant chemoimmunotherapy a more favorable approach? Furthermore, which postoperative adjuvant strategy should be selected for patients receiving neoadjuvant chemoimmunotherapy? What is the role of postoperative radiotherapy (PORT)? Considering the encouraging efficacy of neoadjuvant chemoimmunotherapy, can downstaging transformation be achieved through an aggressive inductive strategy for patients with traditionally unresectable tumors? Lastly, which therapeutic strategy should be selected for patients who have locally advanced cancer with driver genes?
This review comprehensively explored the landscape of relevant therapeutic modalities in patients with LA-NSCLC, examining unresolved challenges and future directions in the field, with a particular focus on driver gene-positive NSCLC. The overall goal is to facilitate stratified management of the highly heterogeneous LA-NSCLC population, thereby improving patient outcomes.
2 RESECTABLE LA-NSCLC
2.1 Adjuvant therapy
Postoperative adjuvant chemotherapy improves patient prognosis; however, studies have shown that its OS benefit (approximately 5%) remains unsatisfactory [4-7]. Therefore, adjuvant immunotherapeutic strategies have gradually emerged. The representative IMpower010 trial (NCT02486718) revealed that compared with best supportive care, treatment comprising atezolizumab upon complete tumor resection and after adjuvant chemotherapy with platinum-containing regimens improved the 3-year disease-free survival (DFS) rate (hazard ratio [HR] = 0.66) and 5-year OS rate (HR = 0.71) by 12.0% and 9.3%, respectively, in patients who had stage II-IIIA NSCLC with a programmed death-ligand 1 (PD-L1) expression rate of ≥ 1%. Moreover, the clinical benefit of atezolizumab was PD-L1 expression dependent; 17.3% improvement in the 5-year OS rate (HR = 0.42) was achieved in patients with high PD-L1 expression (≥ 50%) and no epidermal growth factor receptor (EGFR) mutations or anaplastic lymphoma kinase (ALK) rearrangement [8, 9]. Consistent with these findings, the KEYNOTE-091 trial (NCT02504372) showed that treatment with pembrolizumab improved the median DFS (mDFS) of the overall population by 11.6 months (HR = 0.76, P = 0.0014) compared with placebo; however, no significant DFS benefit was observed in patients with high PD-L1 expression (HR = 0.82, P = 0.14) [10]. Nevertheless, there are still many questions to be considered and explored in the field of adjuvant therapy these include: adjuvant chemotherapy, duration of postoperative adjuvant immunotherapy maintenance and biomarkers for adjuvant therapy protocol.
2.2 Adjuvant chemotherapy
The survival benefit of adjuvant chemotherapy is related to the disease stage. Patients with stage IA disease do not benefit from adjuvant chemotherapy, whereas patients with stage II-III disease experience significant benefit. The benefit of adjuvant chemotherapy in patients with stage IB disease remains unclear, but adjuvant chemotherapy is recommended for patients with stage IB disease who have characteristics associated with high risk [7]. The > 40% incidence of grade ≥ 3 hematologic toxicities and 0.9% rate of chemotherapy-related mortality reported in the LACE-BIO study (NCT01294280) also merit attention [7]. Long-term follow-up analysis in the International Adjuvant Lung Cancer Trial (NCT00002823) showed that although adjuvant chemotherapy had a preventive effect on local recurrence (HR = 0.73, P = 0.003), it did not significantly inhibit brain metastases (HR = 1.1, P = 0.61); moreover, the risk of non-cancer death increased according to follow-up duration on adjuvant chemotherapy (HR = 3.6, P < 0.001) [11]. Thus, the limited survival benefit and remarkable toxicity highlight the limitations of postoperative adjuvant chemotherapy. In the KEYNOTE-091 trial, 14% of patients did not receive adjuvant chemotherapy, whereas 80% received 3 to 4 cycles of adjuvant chemotherapy; a more pronounced DFS benefit was observed among patients who received sequential adjuvant chemotherapy and immunotherapy (HR = 0.73, 95% confidence interval [CI] = 0.60-0.89), and there were no substantial safety concerns [10]. Indeed, synergistic effects between chemotherapy and immunotherapy in patients with advanced NSCLC have been extensively documented in multiple clinical studies; therefore, immunotherapy maintenance after adjuvant chemotherapy is a reasonably better option (Table 1, Figure 1). Treatment outcome was improved in the sequential treatment arm because postoperative treatment with immune checkpoint inhibitors (ICIs) is mainly directed against micrometastatic disease, which has a low neoplastic burden and subclonal divergence; therefore, it responds favorably to cytotoxic drugs. This concept will receive further validation in relevant studies that are currently underway (Figure 2).
| Trial | No. of patients (stage) | Regimen | Median DFS (months) (HR; 95% CI) | Median OS (months) (HR; 95% CI) |
|---|---|---|---|---|
|
IMpower010 [8] (NCT02486718) |
413 (IIIA) | CT → atezolizumab vs. BSC × 1 year |
Stage IIIA with PD-L1 ≥ 1%: 42.3 vs. 26.7 (HR = 0.62; 95% CI = 0.42-0.90); Stage IIIA: 32.3 vs. 29.7 (HR = 0.81; 95% CI = 0.61-1.06) |
Stage IIIA with PD-L1 ≥ 1%: NA (HR = 0.71; 95% CI = 0.44-1.15); Stage IIIA with PD-L1 ≥ 50%: NA (HR = 0.30; 95% CI = 0.12-0.74) |
|
PEARLS/KEYNOTE- 091 [10] (NCT02504372) |
177 (IIIA) | CT (optional) → Pembrolizumab vs. placebo × 1 year | NR (HR = 0.92; 95% CI = 0.69-1.24) | NR |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; CT, chemotherapy; BSC, best supportive care; HR, hazard ratio; CI, confidence interval; DFS, disease-free survival; OS, overall survival; PD-L1, programmed death-ligand 1; NA, not available; NR, not reached.
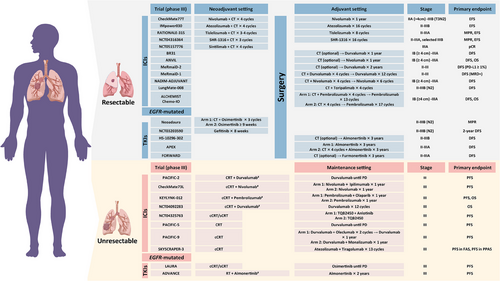
2.3 Duration of adjuvant immunotherapy maintenance
The optimal duration of postoperative adjuvant immunotherapy maintenance in NSCLC remains unclear; therefore, trials such as IMpower010 [8, 9], ANVIL (NCT02595944) [12], KEYNOTE-091 [10], and BR31 (NCT02273375) [13] are currently exploring the impact of 1-year adjuvant immunotherapy cycles. It is unknown whether a longer duration will lead to a more pronounced survival benefit. Thus, we refer to data from analyses of unresectable LA-NSCLC because surgery and radiotherapy are both radical treatment modalities in this locally advanced setting. It is unsurprising that the PACIFIC study (NCT02125461) suggested a significant survival benefit associated with 1 year of durvalumab consolidation treatment after cCRT for unresectable LA-NSCLC [14]. A tailing effect was clearly detected after cessation of 1-year ICI consolidation, suggesting that immunotherapy alters the tumor microenvironment and thus exerts a sustained effect, providing an important safeguard for drug discontinuation [15]. Relative to the PACIFIC study, the GEMSTONE-301 trial (NCT03728556) extended the duration of sugemalimab consolidation to 2 years, achieving a median progression-free survival (mPFS) of 10.5 months (HR = 0.55) for the overall population in the immunotherapy group [16, 17], where the HR was similar to the result in the PACIFIC trial. Hence, a longer immune maintenance therapy duration may not be more efficient, but these data should be interpreted cautiously because of differences in drug use, the PD-L1 expression profile of the enrolled population, efficacy assessment, and the baseline characteristics of the population enrolled in each trial. The pharmacoeconomic burden caused by a prolonged duration of immunotherapy should also be considered. We believe that 1-year postoperative adjuvant immunotherapy maintenance is sufficient, and we recommend measurement of biomarkers such as memory T cells [15], circulating tumor DNA (ctDNA), and minimal residual disease (MRD) [18, 19], which can help to define the optimal duration of immunotherapy maintenance.
2.3.1 Biomarkers for adjuvant therapy protocol
There were discrepancies between the IMpower010 [8, 9] and KEYNOTE-091 [10] trials. An exploratory analysis of the IMpower010 suggested that the DFS benefit was associated with PD-L1 expression (PD-L1 < 1% [HR = 0.97], PD-L1 = 1%-49% [HR = 0.87], PD-L1 ≥ 50% [HR = 0.43]) within the stage II–IIIA population [8]. In contrast, the DFS benefit in the KEYNOTE-091 trial was independent of PD-L1 expression, and adjuvant immunotherapy also conferred a DFS benefit to the PD-L1 < 1% population (HR = 0.78, 95% CI = 0.58-1.03). There was even a negative DFS in the population with tumors expressing PD-L1 on ≥ 50% of cancer cells as a study endpoint [10]. Factors that may have contributed to these differences include the following: (1) Patients registered in the IMpower010 trial received adjuvant chemotherapy, whereas adjuvant chemotherapy was not a requirement in the KEYNOTE-091 trial (14.2% of patients did not receive adjuvant chemotherapy). (2) The proportion of patients with stage IIIA disease was higher in the IMpower010 trial than in the KEYNOTE-091 trial (40.4% vs. 30.0%), whereas stage IB disease was more common in the KEYNOTE-091 trial (14.2% vs. 12.8%). (3) IMpower010 was an open-label trial, whereas KEYNOTE-091 was a randomized, triple-blind trial. (4) The two trials used different assays to determine the PD-L1 expression status (PD-L1 IHC22C3 reagent in KEYNOTE-091 vs. SP142 assay in IMpower010). (5) Finally, in the KEYNOTE-091 trial, the PD-L1 ≥ 50% subpopulation in the placebo group had relatively superior mDFS compared with the other PD-L1 subgroups; this difference may be explained by randomization considerations and is the potential cause of negative results in the PD-L1 ≥ 50% population. Overall, we believe that PD-L1 expression plays a role in predicting the efficacy of adjuvant immunotherapy.
On-treatment ctDNA dynamics also helped to predict the efficacy. The IMpower010 trial showed that postoperative ctDNA non-clearance was associated with worse DFS. However, both the ctDNA-uncleared and ctDNA-cleared stage II-IIIA populations benefitted from adjuvant ICI therapy; only the ctDNA-uncleared, PD-L1 < 1% population did not achieve a significant DFS benefit (HR = 0.88; 95% CI = 0.40-1.91) [20]. A recent trial including patients with stage I-III NSCLC who underwent definitive surgery showed that only 3.2% of patients with longitudinal undetectable MRD developed recurrence, resulting in a negative predictive value of 96.8%; the positive predictive value of longitudinal detectable MRD was 89.1%. Although adjuvant therapy did not improve DFS among patients with undetectable MRD (HR = 2.29, 95% CI = 0.85-6.11), it conferred a survival benefit for patients with detectable MRD (HR = 0.34, 95% CI = 0.12-0.88) [21]. Similarly, the LUNGCA-1 trial (NCT03317080) showed that the postoperative presence of ctDNA-based MRD was associated with disease relapse (HR = 11.1) [22]. Furthermore, recurrence-free survival was higher in MRD-uncleared patients who received adjuvant therapy than in MRD-uncleared patients who did not receive adjuvant therapy (HR = 0.3, P = 0.008). In MRD-negative patients, adjuvant therapy did not prolong recurrence-free survival. Therefore, dynamic monitoring of ctDNA/MRD in the perioperative period demonstrates the potential to predict the risk of recurrence and may indicate a need for adjuvant therapy.
2.4 Adjuvant radiotherapy for resectable LA-NSCLC
A historical study by the PORT Meta-analysis Trialists Group suggested that PORT adversely affects survival prognosis among patients with stage I/II (N0-N1) disease [23]; additional studies confirmed that PORT may improve survival prognosis among patients with stage III–N2 NSCLC [24-28]. In 2021, the continuous innovation of radiotherapy techniques caused the PORT-C trial (NCT00880971) [29] and Lung ART trial (NCT00410683) [30] to become landmarks in the context of modern radiotherapy techniques (Table 2). The PORT-C trial explored the use of intensity-modulated radiation therapy (IMRT) as postoperative adjuvant treatment in patients with pIIIA-N2 disease. In particular, analysis of the modified intention-to-treat population revealed that PORT could reduce the local recurrence rate (HR = 0.71, P = 0.03), but it did not deliver DFS and OS benefits (DFS: HR = 0.84, P = 0.20; OS: HR = 1.02, P = 0.93). Exploratory stratified analysis based on the number of detected lymph nodes and positive lymph nodes suggested that PORT could improve DFS (HR = 0.75, P = 0.04). In contrast, the per-protocol analysis showed that PORT could significantly improve DFS (HR = 0.75, P = 0.05), but the OS remained unchanged (HR = 0.83, P = 0.41). In terms of safety, no grade 4 or 5 adverse reactions associated with radiotherapy were observed. However, the Lung ART trial, which mainly used three-dimensional conformal radiation therapy (CRT) as adjuvant technology (in 89% of patients), also yielded negative results (DFS: HR = 0.86, P = 0.18).
| Trial | No. of patients with stage III | Regimen | DFS rate | OS rate | Median DFS (months) (HR; 95% CI) |
|---|---|---|---|---|---|
|
PORT-C [29] (NCT00880971) |
394 | 3D-CRT/IMRT vs. non-PORT | 40.5% vs. 32.7% | 78.3% vs. 82.8% | 22.1 vs. 18.6 (HR = 0.84; 95% CI = 0.65-1.09) |
|
Lung ART [30] (NCT00410683) |
501 | 3D-CRT/IMRT vs. non-PORT | 47.0% vs. 44.0% | 67.0% vs. 69.0% | 30.5 vs. 22.8 (HR = 0.86; 95% CI = 0.68-1.08) |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; 3D, 3-dimensional; CRT, conformal radiotherapy; IMRT, intensity modulated radiotherapy; DFS, disease-free survival; OS, overall survival; HR, hazard ratio; CI, confidence interval.
Analysis of the Lung ART study design showed that it was more difficult to ensure optimal protection of normal tissue from irradiation, compared with the IMRT approach used in the PORT-C trial [29, 30]. Additionally, when metastasis was detected at one lymph node station, the next lymph node station was included in the clinical target volume, according to the Lung ART outlining protocol. This guideline resulted in a relatively large irradiation field and, therefore, increased the incidence of cardiotoxicity (11 [52%] of 21 deaths were associated with cardiotoxicity). In contrast, data from the RTOG 0617 trial (NCT00533949) suggested that the dose of irradiation to the heart is an independent predictor of survival in patients with LA-NSCLC; compared with three-dimensional CRT, IMRT can be better focused on the target area and thus cause less damage to other organs [31]. Moreover, 23.9% of patients in the PORT-C trial refused PORT, implying that the primary endpoint of the study was not met in the intention-to-treat analysis. Nonetheless, PORT significantly improved the 3-year DFS rate in the per-protocol analysis, suggesting that nearly 76% of patients receiving radiotherapy in the PORT group experienced a clinical benefit. In summary, there is insufficient evidence to definitively exclude the use of PORT. In the future, the following areas should be explored in greater detail: improving the target pattern and reducing toxicity, exploring new radiotherapy techniques, and conducting radiotherapy with the aid of biomarkers, such as ctDNA/MRD and the postoperative pathological response. Additional studies related to postoperative adjuvant radiotherapy are currently exploring the timing and status of postoperative adjuvant radiotherapy (Table 3).
| Trial | Exploration question | Stage | No. of patients | Regimen | Primary endpoint | Estimated completion date |
|---|---|---|---|---|---|---|
| NCT02974426 | Optimal timing of PORT | III (N2) | 1094 | 50.4Gy/28F; PORT-first vs. PORT-last | DFS | December 2021 (incomplete) |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; DFS, disease-free survival.
2.5 Neoadjuvant therapy for resectable LA-NSCLC
In the 1980s, Frei et al. [32] proposed the concept of neoadjuvant therapy. Notably, conventional neoadjuvant chemotherapy increased the 5-year OS rate by 5%, but it had no advantage over adjuvant chemotherapy (HR = 0.99, P = 0.91) [33-37]. Early studies involving older radiation strategies showed that although neoadjuvant chemoradiotherapy did not improve the ultimate survival benefit, it improved the rates of downstaging and R0 resection [38-42]. However, complications of radiotherapy itself and the increased risk of postoperative complications are persistent problems [43, 44]. The tumor microenvironment undergoes immunosuppressive changes during disease progression; the immunosuppressive state is exacerbated by trauma and postoperative loss of tumor antigens, resulting in a “window period” of immunodeficiency [45]. Preoperative immunotherapy can promote greater release of tumor antigens, enhance T-cell activation, kill in situ tumors, and shrink preoperative lesions; it can also eliminate micrometastases, establish systemic immune surveillance, and enable patients to be sustained throughout the duration of the immunodeficiency state, leading to long-term survival benefits [46-48]. Thus, there are multiple explorations of neoadjuvant immunotherapy feasibility (Table 4, Figure 1).
| Trial | No. of patients (stage) | Regimen | MPR rate | pCR rate | Median EFS (months) (HR; 95% CI) |
|---|---|---|---|---|---|
|
(NCT02998528) |
228 (IIIA) | Nivolumab + CT vs. CT × 3cycles → S → CT ± RT | 40.7% vs. 9.6% | 23% vs. 0.9% | 31.6 vs.15.7 (HR = 0.54; 95% CI = 0.37-0.80) |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; CT, chemotherapy; S, surgery; RT, radiotherapy; MPR, major pathological response; pCR, pathological complete response; EFS, event-free survival; HR, hazard ratio; CI, confidence interval.
2.5.1 Neoadjuvant mono-immunotherapy
The CheckMate 159 trial (NCT02259621) demonstrated a major pathological response (MPR) rate of 45% and a pathological complete response (pCR) rate of 10% in patients with stage I-IIIA resectable disease after 2 preoperative cycles of nivolumab; recurrence-free survival (RFS) rates at 3, 4, and 5 years were 65%, 60%, and 60%, respectively, and the corresponding OS rates were 85%, 80%, and 80% [49, 50]. The survival benefit reached a plateau after 3 years, reflecting the sustained benefit of neoadjuvant nivolumab immunotherapy. The results of the LCMC3 trial (NCT02927301) also suggested that the application of neoadjuvant atezolizumab monotherapy to stage IB-selective IIIB NSCLC led to a substantially high survival plateau (3-year DFS and OS rates of 72% and 80%, respectively); however, it was associated with relatively low rates of MPR (20.4%) and pCR (6.8%) [51, 52]. Similarly, a trial involving a Chinese population (ChiCTR-OIC-17013726) showed that 2-cycle neoadjuvant sintilimab immunotherapy was associated with an MPR rate of 40.5%, a primary tumor pCR rate of 16.2%, and a lymph node pCR rate of 8.1% in patients with stage IA-IIIB NSCLC; the most pronounced responsiveness was derived from squamous cell carcinoma [53]. The rationale of administering immunotherapy to patients with resectable NSCLC in the neoadjuvant setting was also evaluated. Caushi et al. [54] showed that patients with MPR after neoadjuvant mono-immunotherapy had higher expression levels of genes associated with memory (interleukin-7 receptor [IL7R] and transcription factor 7 [TCF7]) and effector function (granayme K [GZMK]) in mutation-associated neoantigen-specific T cells. Moreover, mutation-associated neoantigen-specific T-cell-related disorder genes (TOX high mobility group box family member 2 [TOX2], cytotoxic T lymphocyte associate protein 4 [CTLA4], hepatitis A virus cellular receptor 2 [HAVCR2], and ectonucleoside triphosphate diphosphohydrolase 1 [ENTPD1]) were significantly higher in the non-MPR population; immune checkpoint and depletion scores tended to be higher. The study provided new insights concerning immune efficacy assessment and efforts to overcome immune resistance.
2.5.2 Neoadjuvant and perioperative chemoimmunotherapy
In the field of neoadjuvant/perioperative chemoimmunotherapy, the first questions are as follows: does the combined therapy produce an improved pathological response, and how does it influence surgical treatment? The NADIM trial (NCT03081689) was a milestone study concerning the feasibility of neoadjuvant chemoimmunotherapy. Although it had a single-arm design, the results showed an MPR rate of 83%, a pCR rate of 63%, and a pathological downstage rate of 90% [55, 56]. The subsequent NADIM II trial (NCT03838159) confirmed that, compared with neoadjuvant chemotherapy, neoadjuvant chemoimmunotherapy in patients with stage IIIA-B NSCLC significantly improved the pCR rate (7% vs. 37%, relative risk = 5.34), MPR rate (14% vs. 52%), and objective response rate (ORR; 48% vs. 74%). Although there was an increase in grade 3-4 adverse events (10% vs. 24%), they were generally manageable and did not affect subsequent surgical treatment. The PD-L1 status had predictive value for the pCR rate (P = 0.008) [57, 58]. Later, as the first phase III analysis of neoadjuvant chemoimmunotherapy, the CheckMate 816 trial (NCT02998528) showed that neoadjuvant chemoimmunotherapy significantly increased the MPR rate (36.9% vs. 8.9%) and pCR rate (24.0% vs. 2.2%, P < 0.001) compared with neoadjuvant chemotherapy, reaching a pCR rate of 23.0% (vs. 0.9%) in patients with stage IIIA disease. The proportion of patients undergoing surgery was higher among patients who received neoadjuvant chemoimmunotherapy than among the control group (83% vs. 75%), but there was no increase in surgical difficulty [59, 60].
The feasibility of neoadjuvant chemoimmunotherapy has been confirmed in four other recent randomized phase III clinical trials using perioperative ICI therapy: AEGEAN (NCT03800134) [61], NEOTORCH (NCT04158440) [62], KEYNOTE-671 (NCT03425643) [63], and CheckMate 77T (NCT04025879) [64]. The MPR rates in these studies were 30.2%-48.5%, and the pCR rates were 17.2%-25.3%. The MPR and pCR rates varied among trials varied, presumably because of differences in the pathological evaluation protocols. The International Association for the Study of Lung Cancer further standardized the pathological evaluation of postoperative resection specimens after neoadjuvant therapy, recommending evaluation of surgical specimens to determine the percentages of surviving tumor, necrosis, and stroma displaying fibrosis and inflammation. Moreover, MPR should be regarded as a reduction in the percentage of active tumors below the optimal threshold value of clinical significance, which is determined by histologic type and prior evidence of a specific treatment regimen. The optimal threshold for MPR was previously defined as 10% for all types of lung cancer, whereas recent studies suggest that the optimal threshold varies according to histologic type (squamous: 10%, adenocarcinoma: 65%). Thus, further validation is needed [65].
In terms of safety, the CheckMate 159 [49] and LCMC3 [51] trials showed that the rates of grade 3 and 4 treatment-related adverse events (TRAEs) were 4.5% and 6.0%, respectively; these were lower than the rate of 33.5% observed in the chemoimmunotherapy arm of the CheckMate 816 trial. However, a meta-analysis showed that although neoadjuvant chemoimmunotherapy increased the incidence of TRAEs compared with immunotherapy monotherapy (73.9% vs. 42.9%), the incidence of severe adverse events did not significantly increase (18% vs. 12.3%, P = 0.32). Moreover, the rates of surgical resection were similar between the two arms (84.4% vs. 89.2%), whereas the incidence of delayed surgery was lower in the neoadjuvant chemoimmunotherapy arm [66]; therefore, the overall adverse effects of the neoadjuvant chemoimmunotherapy strategy were manageable.
Considering that combined modalities improve the MPR rate, the second question regarding neoadjuvant/perioperative chemoimmunotherapy is as follows: what is the optimal duration of inductive chemoimmunotherapy? In addition to ongoing clinical trials concerning the efficacies of various ICIs in neoadjuvant chemoimmunotherapy strategies [67-69], the neoSCORE trial (NCT04459611) is currently exploring the optimal number of neoadjuvant cycles for chemoimmunotherapy. Thus far, this trial has demonstrated numerical superiority in the three-cycle group compared with the two-cycle group (MPR rate: 41.4% vs. 26.9%, P = 0.260; pCR rate: 24.1% vs. 19.2%, P = 0.660) [70]. The optimal number of neoadjuvant therapy cycles is mainly determined by the MPR rate, but there is a logical paradox: if a patient does not undergo surgery, their pathological remission status cannot be determined. Therefore, an accurate method for preoperative evaluation of the pathological result is urgently needed. Indeed, artificial intelligence-based deep learning approaches have emerged to overcome this limitation; one relevant study showed that a combined model integrating clinical features and artificial intelligence-based deep learning scores could effectively predict whether patients with NSCLC achieved MPR after neoadjuvant chemoimmunotherapy (internal validation cohort: area under the curve = 0.77, 95% CI = 0.64-0.89; external validation cohort: area under the curve = 0.75, 95% CI = 0.62-0.87). The study also revealed that the underlying biological basis of deep learning scores may be related to microenvironmental activation of signaling pathways that mediate tumor proliferation and promote antitumor immune cell infiltration [71]. However, the mechanisms underlying neoadjuvant chemoimmunotherapy outcomes have also been reported. Hui et al. [72] scanned the entire immune microenvironment and found a decreased number of intratumoral-activated Tregs in MPR tumors, along with clonal expansion of peripheral cytotoxic CD8+ T cells. Another study revealed therapy-promoting expansion of cytotoxic T cells and activation of memory CD8+ T cells into an effector phenotype, as well as MPR-associated reduction of neutrophil heterogeneity in the aged CCL3+ neutrophil/secreted phosphoprotein 1(+)/tumor-associated macrophage pathway [73].
The third and most critical question regarding neoadjuvant/perioperative chemoimmunotherapy is as follows: can the remarkable pathological response be translated into an improved prognosis? Cross-study comparisons should be performed with caution. However, considering the different study designs and chemotherapy regimens, it is intriguing that the HRs for disease progression, disease recurrence, or death were 0.68 in the CheckMate 816 trial, 0.81 (95% CI = 0.67-0.99) in the IMpower010 trial, and 0.76 (95% CI = 0.63-0.92) in the KEYNOTE-091 trial. These findings indicate that neoadjuvant ICI therapy has a more central role. In support of this perspective, the findings in related studies have suggested that the tumor-draining lymph nodes are important components of the antitumor immunotherapy response; therefore, standard lymph node dissection during surgical resection may affect subsequent efficacy of adjuvant immunotherapy [74-76]. The next priority involves determining whether a perioperative approach would provide benefits beyond either approach alone.
Although positive results were obtained in all perioperative trials, comparable advantages were reported over the CheckMate 816 trial in terms of the 2-year event-free survival (EFS) rate (CheckMate 816: 63.8%; KEYNOTE-671: 61.5%; AEGEAN: 63.3%) and the HR for EFS (CheckMate 816: HR = 0.63 [95% CI = 0.43-0.91]; KEYNOTE-671: HR = 0.59 [95% CI = 0.48-0.72]; AEGEAN: HR = 0.68 [95% CI = 0.53-0.88]; CheckMate 77T: HR = 0.58 [97.36% CI = 0.42-0.81]). Moreover, in the comparison of HR among patients with stage IIIA disease, advantages were almost identical (CheckMate 816: HR = 0.54 [95% CI = 0.37-0.80]; KEYNOTE-671: HR = 0.57 [95% CI = 0.44-0.74]; AEGEAN: HR = 0.57 [95% CI = 0.39-0.83]; NEOTORCH: HR = 0.44 [95% CI = 0.287-0.661]) (Table 5, Figure 1). Very recently, the KEYNOTE-671 firstly reported a statistically significant and clinically important OS improvement (HR 0.72, 95% CI = 0.56-0.93) [77]. However, considering the cost-effectiveness ratio and ICI-related toxicity, more evidence is required to support the use of a perioperative immunotherapy strategy; the final answer to this question will be determined by eventual survival outcomes.
| Trial | No. of patients (stage) | Regimen | MPR rate | pCR rate | Median EFS (months) (HR; 95% CI) |
|---|---|---|---|---|---|
|
AEGEAN [61] (NCT03800134) |
524 (IIIA-B) | Durvalumab vs. placebo + CT × 3 cycles → S → durvalumab vs. placebo × 12cycles | NA |
Stage IIIA: 18.5% vs. 4.8%; Stage IIIB: 10.2% vs. 3.1% |
Stage IIIA: NR vs.19.5 (HR = 0.57; 95% CI = 0.39-0.83); Stage IIIB: 31.9 vs. 18.9 (HR = 0.83; 95% CI = 0.52-1.32) |
|
KEYNOTE-671 [63] (NCT03425643) |
558 (IIIA-B) | Pembrolizumab vs. placebo + CT × 4 cycles → S → pembrolizumab × 13 cycles | NA | NA | Stage III: NR (HR = 0.54; 95% CI = 0.42-0.70); |
|
NEOTORCH [62] (NCT04158440) |
401 (IIIA-B) | Toripalimab vs. placebo + CT × 4 cycles → S → toripalimab vs. placebo × 13 cycles | 45.8% | 24.8% | Stage III: NR vs. 15.5 (HR = 0.40; 95% CI = 0.27-0.57) |
| CheckMate 77T [64] | 295 (IIIA-B) | Nivolumab vs. placebo + CT × 4 cycles → S → nivolumab vs. placebo × 1 year | NA | 23.0% | Stage III: 30.2 vs. 13.4 (HR = 0.51; 95% CI = 0.36-0.72) |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; CT, chemotherapy; S, surgery; MPR, major pathological response; pCR, pathological complete response; EFS, event-free survival; HR, hazard ratio; CI, confidence interval.
2.5.3 Neoadjuvant dual immunotherapy
The results of the NEOSTAR trial (NCT04230109) suggested that neoadjuvant nivolumab plus ipilimumab improved the rates of MPR (38% vs. 22%) and pCR (29% vs. 9%) compared with nivolumab alone, and the safety profiles were identical (10% vs. 13%); however, more patients in the combination group received nonsurgical treatment (4 vs. 1) [78]. Although dual ICI therapy had better efficacy, this efficacy was offset by the loss of surgical opportunities. PD-L1 expression was correlated with the pathological response. Another study (NCT02259621) evaluating nivolumab plus ipilimumab as a neoadjuvant regimen was discontinued because of the incidence of TRAEs reached 67%, including a 33% incidence of grade ≥ 3 TRAEs [79]. Other dual ICI therapy trials include analyses of volrustomig (anti-PD-1/CTLA4), as well as PD-1/PD-L1 inhibitors combined with oleclumab (anti-CD73), monalizumab (anti-NKG2A) [80], danvatirsen (anti-STAT3) [81], or relatlimab (anti-LAG3) [82]. Considering the limited efficacy in the advanced setting, these novel immune checkpoints require further investigations.
2.5.4 Neoadjuvant radiotherapy combined with immunotherapy
Altorki et al. [83] reported a significantly higher MPR rate with neoadjuvant durvalumab and stereotactic body radiotherapy, compared with durvalumab alone (53.3% vs. 6.7%); the pCR rate in the combined group reached 26.7%. No additional safety concerns were reported (grade 3-4 adverse events: 20% vs. 17%); only one (3%) of 33 patients in the combined group underwent delayed surgery because of adverse reactions. The results of another study suggested that durvalumab combined with neoadjuvant sub-ablative radiation did not prolong the duration of surgery, and no new safety concerns were identified (grade 3-4 adverse events: 38%) [84]. Therefore, neoadjuvant immunotherapy combined with radiotherapy might be a chemotherapy-free alternative for patients with a large tumor load and N2 metastases who can undergo surgery. The ongoing SQUAT study (WJOG 12119L) [85] will provide further insights concerning the benefits of neoadjuvant immunotherapy combined with radiotherapy.
3 UNRESECTABLE LA-NSCLC
3.1 Emerging explorations on top of PACIFIC modality
Unresectable LA-NSCLC is present in 25%-30% of patients with lung cancer, and the current standard of care is the PACIFIC modality. The latest 5-year follow-up data from this trial showed an mPFS of 16.9 vs. 5.6 months (HR = 0.55, 95% CI = 0.45-0.68) and a median OS (mOS) of 47.5 vs. 29.1 months (HR = 0.72, 95% CI = 0.59-0.89) for cCRT followed by consolidation durvalumab, compared with cCRT [86]. The clinical application of the PACIFIC protocol attracted substantial attention from clinicians, who began to question whether greater survival benefits could be achieved by shifting to earlier immunotherapy timing. Additionally, they discussed whether patients treated with sequential chemoradiotherapy (sCRT) followed by consolidation immunotherapy could also benefit from this modality. Finally, they asked whether more combined modalities of cCRT and immunotherapy would be developed. In the KEYNOTE-799 trial (NCT03631784) involving earlier immunotherapy, pembrolizumab combined with chemotherapy was administered for one cycle, followed by pembrolizumab combined with cCRT; subsequently, therapy was continued with pembrolizumab consolidation. The ORR and disease control rates in Cohort A (squamous) were 71.4% and 88.4%, respectively; Cohort B (non-squamous) had an ORR of 75.5% and a disease control rate of 93.1%. Additionally, the mPFS in Cohort A was 30.6 months with a 2-year PFS rate of 55.3%, whereas the mPFS in Cohort B was not reached with a 2-year PFS rate of 60.6%. In terms of safety, the KEYNOTE-799 study showed 8.0% and 6.9% incidences of grade ≥ 3 pneumonia in Cohorts A and B, respectively, along with 3.6% and 1.0% incidences of grade 5 lethal pneumonia. All fatal cases of pneumonia were potentially associated with pembrolizumab; one case was also potentially associated with radiotherapy [87, 88]. In contrast, the respective incidences of grade 3 and 4 pneumonia in the consolidation immunotherapy group were 4.4% and 3.8% in the PACIFIC trial [89], suggesting that greater attention to toxicity is needed for synchronized immunotherapy combined with radiotherapy. However, the GEMSTONE-301 trial enrolled patients who had unresectable stage III cancer without disease progression after concurrent or sequential chemoradiotherapy; both cCRT and sCRT followed by ICI consolidation resulted in PFS improvement [16]. Notably, the 3-year OS rates in PACIFIC and PACIFIC-R (NCT03798535) [90] and the sCRT and cCRT cohorts in the GEMSTONE-301 trial were 57.9%, 56.7%, 59.0%, and 54.1%, respectively (Table 6, Figure 3). Studies are currently testing differences in the combination patterns of ICI therapy and sCRT/cCRT according to differences in administration timing [91-96] (Figure 2). With respect to biomarkers, Moding et al. [97] assessed the MRD status via ctDNA dynamic monitoring to explore its value in predicting the prognosis of patients with LA-NSCLC who received consolidation immunotherapy after chemoradiotherapy. Overall, although the sample size was limited, the study demonstrated that the 1-year freedom from progression rate in the chemoradiotherapy group was significantly better among patients with undetectable ctDNA than among patients with detectable ctDNA (100% vs. 0%). Additionally, ctDNA dynamic monitoring results from patients receiving combined chemoradiotherapy and immunotherapy suggested that ICI consolidation did not improve freedom from progression in ctDNA(−) patients, whereas ctDNA(+) patients were more likely to benefit from ICI maintenance.
| Trial | No. of patients (stage) | Regimen | HR for PFS (95% CI) | HR for OS (95% CI) | Survival (months) |
|---|---|---|---|---|---|
|
PACIFIC [14] (NCT02125461) |
696 (IIIA-B) | cCRT → durvalumab vs. placebo × 1 year |
Stage IIIA: 0.53 (0.40-0.69); Stage IIIB: 0.64 (0.48-0.85) |
Stage IIIA: 0.61 (0.47-0.80); Stage IIIB: 0.86 (0.63-1.17) |
mPFS of stage III: 16.9 vs. 5.6; mOS of stage III: 47.5 vs. 29.1 |
|
(NCT03728556) |
378 (IIIA-C) | cCRT/sCRT → sugemalimab vs. placebo × 2 years |
Stage IIIA: 0.79 (0.46-1.35); Stage IIIB: 0.57 (0.40-0.81); Stage IIIC: 0.73 (0.39-1.36) |
Stage III: 0.69 (0.49-0.97) |
mPFS of stage IIIA: 13.1 vs. 6.2; stage IIIB: 10.5 vs. 6.2; stage IIIC: 8.4 vs. 5.4; mOS of stage III: NR vs. 25.9 |
|
PACIFIC-R [90] (NCT03798535) |
1318(IIIA-C) | cCRT/sCRT → durvalumab × 1year | NA | NA | mPFS of stage III: 24.1; stage IIIA: 23.7; stage IIIB-C: 19.2 |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; cCRT, concurrent chemoradiotherapy; sCRT, sequential chemoradiotherapy; PFS, progression-free survival; OS, overall survival; HR, hazard ratio; CI, confidence interval; mPFS, median progression-free survival; mOS, median overall survival; NA, not available.
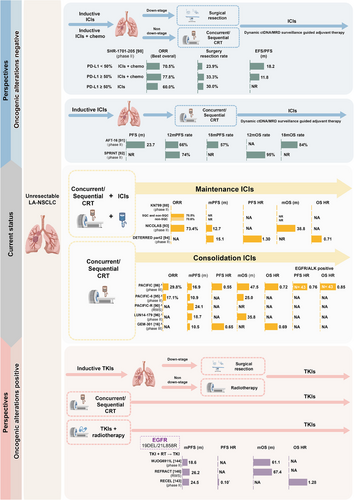
3.2 Redefinition of unresectable LA-NSCLC
Traditionally, most stage IIIB to all IIIC cases of LA-NSCLC were considered unresectable. The aforementioned impressive efficacy of neoadjuvant chemoimmunotherapy leads to questions regarding the conversion of unresectable status to resectable status via chemo-immune induction. In the SAKK series trials, 50.8% and 1.9% of patients had stages IIIB NSCLC and IIIC NSCLC, respectively. The results showed that patients with stage IIIB NSCLC had OS rates of 35% and 27% at 5 and 10 years, respectively, with an mOS of 26 months; the OS rates were 41% and 29% in patients with stage IIIC NSCLC [41]. More recently, Wu et al. [98] (NCT04580498) showed that 27 of 107 (25.2%) patients with multidisciplinary team-confirmed unresectable LA-NSCLC were successfully converted to resectable status after three cycles of PD-L1/transforming growth factor-β bispecific antibody induction therapy. The conversion rates were 37% for patients with stage IIIA disease, 44.4% for patients with stage IIIB disease, and 18.5% for patients with stage IIIC disease; all patients achieved R0 resection. The 1-year EFS rate in patients with conversion was 74.4%, and median EFS (mEFS) was not reached, whereas the 1-year EFS rate was 55.9%, and mEFS was 14.9 months in patients with failed conversion. However, the evidence thus far is insufficient to conclude that post-conversion surgical resection plays a role in this scenario. It is clear that patients with successful conversion are clinically sensitive to chemoimmunotherapy; this characteristic itself is an independent factor contributing to the differences in EFS. In an early study concerning whether resection after inductive cCRT was superior to definitive cCRT, no significant survival advantage was detected despite improvement in PFS (HR = 0.77) [99]. Considering that the radiation techniques in this trial were not particularly modern, a survival benefit with surgery is less likely because more advanced and improved radiation capabilities are currently available. However, this speculation should not prevent future studies from redefining the unresectable population, then refining and optimizing the trial design to clarify the role of surgery in this scenario.
3.3 Improvements in radiotherapy techniques for the treatment of unresectable LA-NSCLC
There are also efforts to optimize radiotherapy techniques for the treatment of stage III unresectable NSCLC. Compared with photon therapy and chemotherapy, consolidation immunotherapy after concurrent proton beam radiotherapy and chemotherapy has demonstrated a better safety profile [100, 101]. A retrospective case-control study of patients with stage III NSCLC receiving cCRT and adjuvant durvalumab examined whether intensity-modulated proton therapy (IMPT) or IMRT affected the use of ICIs and the occurrence of immunotherapy-related adverse events. The study included 67 patients (28 in the IMRT group and 39 in the IMPT group), all of whom received radiotherapy at doses of 60-64 Gy. The incidences of immunotherapy-related adverse events of any grade in the IMRT and IMPT groups were 21.4% and 30.8% (P = 0.062), and the incidences of pneumonia during immunotherapy were 25% and 23% (P = 0.8), respectively; safety was similar in both groups. Patient performance status scores after cCRT were significantly better in the IMPT group than in the IMRT group (performance status ≤ 1: 92.9% vs. 71.8%, P < 0.032) [102]. Preclinical evidence suggests that high-dose, low-segmentation radiotherapy enhances antitumor immunity and leads to significant tumor control blockade when used in combination with ICIs [103]. Notably, the radiotherapy safety profile was controlled in the NRG-Lu004 study (NCT03801902) under the accelerated segmentation mode [104]. Briefly, the functional lung dose was reduced with functional lung avoidance using four-dimensional positron emission tomography–computed tomography, and the functional lung avoidance schedule was compared with the conventional schedule. Overall, this accelerated hypofractionated radiation therapy approach allowed an Flung mean dose reduction of ≥ 2%, Flung V20 reduction of 24%, cardiac mean dose of < 30 Gy, and cardiac V50 of < 25%, all of which helped to reduce pulmonary toxicity [105]. Taken together, these findings suggest that the application of advanced technologies can improve radiotherapy safety. There remains a persistent question: does the application of advanced technologies improve radiotherapy efficacy? The answer to this question will be provided by ongoing studies; representative studies include NCT0390017, which is evaluating the efficacy of a hypofractionated radiotherapy technique in synchronous radiotherapy for LA-NSCLC, and NCT03742687, which is evaluating the efficacy of consolidation immunotherapy after proton stereotactic body radiotherapy in synchronous radiotherapy.
4 EGFR-MUTATED LA-NSCLC
EGFR mutations are present in 10%-30% of all cases of LA-NSCLC [106-108], and a targeted regimen is the most important treatment approach for patients with EGFR-sensitive mutations.
4.1 Resectable EGFR-mutated LA-NSCLC
4.1.1 Postoperative adjuvant targeted therapy in resectable EGFR-mutated LA-NSCLC
The BR19 (NCT00049543) [109] and RADIANT (NCT00373425) [110] trials initiated the early exploration of postoperative adjuvant targeted therapy for NSCLC; both trials yielded negative results because of their non-selective design. During the SELECT trial (NCT00462995), adjuvant erlotinib showed an improved 2-year DFS compared with historic EGFR-mutant controls [111]. The ADJUVANT (NCT01405079) and EVIDENCE (NCT02448797) trials confirmed that tyrosine kinase inhibitors (TKIs) had a DFS benefit in the adjuvant setting [112-114], whereas the IMPACT trial (NCT02164513) reported negative results for DFS [115]. Importantly, none of the trials demonstrated an OS benefit, and they revealed poor control of distant and brain metastases [112-114, 116, 117]. On top of the superior PFS and OS outcomes of third-generation EGFR-TKI observed in advanced NSCLC in FLAURA trial [118], the ADAURA trial (NCT02511106) explored the efficacy and safety of osimertinib as adjuvant therapy compared with placebo [119]. The patients received or did not receive postoperative adjuvant chemotherapy and were then randomized, revealing a dual benefit of TKI single-agent targeted therapy and sequential targeted therapy with chemotherapy. The data showed an mDFS of 65.8 vs. 21.9 months (HR = 0.23) in patients with stage II-IIIA disease and an mDFS of 65.8 vs. 28.1 months (HR = 0.27) in patients with stage IB-IIIA disease. For the planned final analysis of OS, the 5-year OS rates were 85% and 73% (HR = 0.49) among patients with stage II to IIIA disease; these rates were 88% and 78% (HR = 0.49) among patients with stage IB to IIIA disease. The results of subgroup analysis suggested that the survival benefit was more pronounced in patients with stage IIIA (HR = 0.37) disease than in patients with stage IB (HR = 0.44) or II (HR = 0.63) disease [120, 121] (Table 7, Figure 1). Analyses of other third-generation TKIs for adjuvant therapy are currently underway (Figure 2).
| Trial | No. of patients (stage) | Regimen | DFS rate | OS rate | Median DFS (months) (HR; 95% CI) | Median OS (months) (HR; 95% CI) |
|---|---|---|---|---|---|---|
|
ADAURA [121] (NCT02511106) |
69 (IIIA) | Osimertinib vs. placebo × 3 years | 4-year: 65% vs. 14% | 5-year: 85% vs. 67% | 55.1 vs. 12.9 (HR = 0.20; 95% CI = 0.14-0.29) | NR (HR = 0.37; 95% CI = 0.20-0.64) |
|
ADJUVANT-CTONG1104[113] (NCT01405079) |
143 (IIIA) | Gefitinib × 2 years vs. CT × 4 cycles | NA | NA | NA (HR for N2 = 0.52; 95% CI = 0.34-0.80) | NA (HR for N2 = 0.92; 95% CI = 0.58-1.45) |
|
EVIDENCE [114] (NCT02448797) |
181 (III) | Icotinib × 2 years vs. CT × 4 cycles | NA | NA | NA (HR = 0.38; 95% CI = 0.24-0.61) | NA |
|
IMPACT [115] (UMIN000006252) |
144 (IIIA); 5 (IIIB) | Gefitinib × 2 years vs. CT × 4 cycles | NA | NA | NA (HR = 0.966; 95% CI = 0.662-1.409) | NA (HR = 1.094; 95% CI = 0.647-1.848) |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; EGFR, epidermal growth factor receptor; CT, chemotherapy; NA, not available; DFS, disease-free survival; OS, overall survival; HR, hazard ratio; CI, confidence interval.
Although the above-described trials revealed successful use of adjuvant targeted therapy to manage NSCLC, they also revealed some problems (Figure 1). The ADJUVANT study showed a significant convergence of DFS curves after approximately 3 years of follow-up. Similarly, the ADAURA trial suggested rapid convergence of DFS curves after nearly 4 years of follow-up [122]. The phenomenon of rapid relapse after the end of adjuvant therapy suggests that adjuvant targeted therapy can only delay the time to disease recurrence; it cannot cure the disease.
There is no conclusive evidence regarding the optimal duration of adjuvant targeted maintenance. The results of the ICOMPARE trial (NCT02274818) suggested that adjuvant treatment with icotinib for 2 years significantly prolonged the mDFS (HR = 0.512) and improved the 6-year OS rate, compared with 1-year maintenance (74.6% vs. 51.3%) [123]. Adjuvant therapy-related studies of gastrointestinal stromal tumors [124] and breast cancer [125] suggested that further extension of adjuvant therapy can yield better survival benefits. However, patient's compliance decreased with the development of adverse events. Concomitantly, the increased socioethical and economic costs associated with a prolonged duration of targeted therapy should also be considered. There is evidence that ctDNA/MRD is a predictor of postoperative disease recurrence and poor prognosis [21, 22, 126]. Additionally, the time to disease recurrence based on assessment of ctDNA/MRD status was earlier than the time to recurrence based on clinical imagings [19, 127]. These findings support that ctDNA/MRD can be used to identify patients at high risk of recurrence; thus, we suggest that people at high risk of postoperative recurrence should be screened according to ctDNA/MRD status, then administered intensive adjuvant targeted therapy. The ADAURA trial is currently exploring the feasibility of combining the ctDNA/MRD status for adjuvant treatment with osimertinib, and we look forward to publication of the results.
4.1.2 Postoperative adjuvant chemotherapy in resectable EGFR-mutated LA-NSCLC
The findings of retrospective studies have suggested that postoperative adjuvant chemotherapy provides minimal survival benefits to patients with an EGFR mutation [128, 129]. In contrast, the ADAURA trial reported a DFS benefit favoring osimertinib vs. placebo in patients with (HR = 0.16) and without adjuvant chemotherapy (HR = 0.23), regardless of disease stage [130]. Comprehensive genomic profiling of patients in the ADJUVANT trial suggested 5 potential predictive biomarkers for DFS: RB1 alterations (favoring adjuvant chemotherapy) and NKX2-1 copy number gain, CDK4 copy number gain, TP53 exon4/5 missense alterations, and MYC copy number gain (all favoring adjuvant gefitinib) [131]. Overall, although EGFR-TKI plays a determinant role in the adjuvant setting, adjuvant chemotherapy remains the recommendation according to international guidelines (stage IB [tumors of ≥ 4 cm] to IIIA; AJCC Seventh Edition) and for EGFR-mutated NSCLC.
4.1.3 Neoadjuvant targeted therapy in resectable EGFR-mutated LA-NSCLC
The EMERGING trial (NCT01407822, CTONG 1103) explored differences in the efficacy of erlotinib vs. chemotherapy as a neoadjuvant regimen for IIIA (N2) EGFR-mutated NSCLC. There was no statistically significant difference regarding ORR (54.1% vs. 34.3%), and the MPR rate was 9.7% vs. 0%; pCR was not observed in either group. Although there was a benefit in terms of PFS (mPFS: 21.5 vs. 11.4 months, HR = 0.36) and a significant decrease in the incidence of grade 3-4 adverse events (0% vs. 29.4%), OS remained negative (mOS: 42.2 vs. 36.9 months; HR = 0.83) [132, 133]. Another non-comparative phase II trial revealed similar results [134]: the NEOS trial (ChiCTR1800016948) showed an ORR of 71.1%, with an MPR of 11% and pCR of 4%. The downstaging rate was 53.3% when osimertinib was used as a neoadjuvant treatment strategy in patients with EGFR-mutated stage II-IIIB NSCLC [135, 136]. Recently, another phase II single-arm trial testing the efficacy of neoadjuvant osimertinib in EGFR-mutated NSCLC also showed negative results: 15% MPR, 0% pCR, and 44% lymph node downstaging rate [137]. Considering these findings, the efficacy of neoadjuvant TKI therapy is unsatisfactory, despite the use of third-generation EGFR-TKIs (Table 8). Additional trials are urgently needed to explore the roles of combined chemotherapy and TKI therapy, define the optimal TKI inductive duration, and test other neoadjuvant strategies (e.g., chemoimmunotherapy) in the neoadjuvant EGFR-mutated scenario (Figure 2).
| Trial | No. of patients (stage) | Regimen | MPR rate | pCR rate | ORR | Survival (months) (HR; 95% CI) |
|---|---|---|---|---|---|---|
|
EMERGING-CTONG 1103 [132, 133] (NCT01407822) |
272 (IIIA-N2) | Erlotinib × 42 days vs. CT × 2 cycles → S → erlotinib × 1 years vs. CT × 2 cycles | 9.7% vs. 0% | 0% vs.0% | 54.1% vs. 34.3% |
mOS: 42.2 vs.36,9 (HR = 0.83; 95% CI = 0.47-1.47); mPFS: 21.5 vs. 11.4 (HR = 0.36; 95% CI = 0.21-0.61) |
| NCT01217619 [154] | 19 (IIIA-N2) | Erlotinib × 56 days → S | NA | NA | 42.1% |
mOS: 51.6; mPFS: 11.2 |
| NCT00600587 [155] | 24 (IIIA-N2) | Erlotinib × 42 days (M+) vs. CT × 3 cycles(M-) → S | NA | 16.7% vs, 25%a | 58.3% vs. 25.0% |
mPFS: 6.9 vs. 9.0 (HR = 2.26; 95% CI = 0.91-5.61); mOS: 14.5 vs. 28.1(HR = 1.79; 95% CI = 0.73-4.40) |
| ASCENT [156] (NCT01553942) | 13 (III) | Afatinib × 2 months → cCRT ± S →CT (optional) → afatinib × 2 years | 57.1% | 14.3% | 69.0% |
mPFS: 34.6 |
|
(ChiCTR1800016948) |
22 (IIIA); 4 (IIIB) |
Osimertinib × 6 weeks → S | 10.7% | 3.6% | 71.1% | NR |
| NCT03433469 [137] | 9 (IIIA) | Osimertinib × 1-4 cycles → S | NA | 0 | NA | NR |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; EGFR, epidermal growth factor receptor; MPR, major pathological response; pCR, pathological complete response; ORR, objective response rate; HR, hazard ratio; CI, confidence interval; CT, chemotherapy; S, surgery; M, mutation; NA. not available; mOS, median overall survival; mPFS, median progression-free survival.
- a Pathological N2 complete response.
4.1.4 Perioperative immunotherapy in resectable EGFR-mutated LA-NSCLC
There is considerable evidence that immunotherapy has minimal effects on EGFR-mutated NSCLC, even after these cancers have become resistant to EGFR-TKIs [138, 139]; there is a risk of hyper-progression in the advanced setting [140]. As mentioned above, EGFR-TKIs have distinct roles at different stages of EGFR-mutated NSCLC. Thus, it is reasonably possible to determine whether perioperative immunotherapy is feasible in the EGFR-positive population. In the advanced disease setting, most perioperative immunotherapy trials excluded patients with EGFR mutations. However, some evidence is available. In the LCMC3 trial, no MPR was observed in patients with known EGFR mutations (n = 7). The CheckMate 816 trial excluded patients with known EGFR mutations or ALK fusions, although the trial protocol did not specify an EGFR/ALK testing requirement. A recent multicenter retrospective study with a limited sample size (n = 40) suggested that neoadjuvant chemoimmunotherapy in resectable driver-positive NSCLC had an ORR of 62.5%, R0 resection rate of 97.4%, MPR of 37.5%, pCR of 12.5%, and mDFS of 28.5 months [141]. The KEYNOTE-671 trial also recruited patients with EGFR-mutated cancer (n = 33); surprisingly, the neoadjuvant chemoimmunotherapy strategy achieved an EFS benefit relative to chemotherapy alone (HR = 0.09; Figure 1). Although potential clinical feasibility was observed, further validation is needed. Before approval, the application of perioperative immunotherapy to resectable oncogene-mutated LA-NSCLC should be used with caution.
In the adjuvant setting, although EGFR mutations showed a DFS benefit in the PEARLS trial, there was no DFS benefit from adjuvant atezolizumab in the IMpower010 trial. Importantly, considering that neoadjuvant TKIs have great potential for improving treatment outcomes, the prioritization of TKIs over adjuvant ICIs in patients with EGFR-mutated NSCLC would never be challenged in the postoperative setting.
4.2 Unresectable EGFR-mutated LA-NSCLC
cCRT is the standard of care for patients who have unresectable stage III NSCLC, with and without EGFR mutations. There are 2 open questions. First, is ICI maintenance reasonable in patients with EGFR-mutated cancer? Post hoc analysis of the PACIFIC trial data suggested that maintenance durvalumab had minimal benefit in the EGFR-positive population (n = 24) compared with placebo (n = 11; PFS: HR = 0.91, OS: HR = 1.02) [142]. Second, what is the role of EGFR-TKIs in unresectable EGFR-mutated LA-NSCLC? Several designs have been tested: concurrent EGFR-TKIs with thoracic radiation therapy with/without EGFR-TKI maintenance [143], cCRT followed by EGFR-TKI maintenance, and TKI induction followed by chemoradiotherapy. The WJOG 6911L trial used concurrent gefitinib (2 years) and definitive thoracic radiation therapy; it showed an ORR of 81.5%, a 2-year PFS rate of 29.6%, and an mOS of 61.1 months in a small population (n = 27) of patients with EGFR-mutated unresectable LA-NSCLC [144]. Using an identical study design, the REVEL trial (NCT01168973) showed an improved PFS compared with cCRT (HR = 0.053, P < 0.001) [145]. Moreover, the REFRACT trial (NCT02531737) revealed that targeted combination radiotherapy significantly improved PFS (HR = 0.40, P < 0.001) and OS (HR = 0.61, P = 0.039) in EGFR-mutated unresectable LA-NSCLC compared with CRT [146] (Table 9, Figure 3). The LOGIK0902/OLCSG0905 phase II study (UMIN000005086) explored the feasibility of gefitinib induction followed by standard CRT in EGFR-mutated stage III NSCLC; it showed a 2-year OS rate of 90% and 1- and 2-year PFS rates of 58.1% and 36.9%, respectively [147]. A meta-analysis of the optimal treatment combination for patients with locally advanced unresectable EGFR-mutated cancer suggested that radiotherapy and TKIs are essential for good treatment outcomes; concurrent radiotherapy and TKIs or CRT followed by TKIs resulted in a significantly longer PFS, compared with CRT alone or CRT with immunotherapy [148]. Overall, more precise treatment is the unavoidable trend for LA-NSCLC with activating driver mutations. Preclinical studies have provided a rationale for these treatment modalities [149, 150]. Ongoing studies will further explore the optimal timing of radiotherapy/CRT and targeted therapies, they may provide necessary answers in the near future (Figure 2).
| Trial | No. of patients(stage) | Regimen | ORR | PFS rate | OS rate | Median PFS (months) | Median OS (months) |
|---|---|---|---|---|---|---|---|
|
WJOG 6911L [144] (UMIN000008366) |
14 (IIIA); 13 (IIIB) |
Gefitinib × 2 years + TRO | 81.5% | 2-year: 29.6% | NA | 18.6 | 61.1 |
|
REFRACT [146] (NCT01168973) |
155 (IIIA); 285 (IIIB) |
CRT vs. RT + TKI ± CT vs. TKI | NA | NA | 5-year: 33.8% vs. 60.6% vs. 38.8% | 12.4 vs. 26.2 vs. 16.2 | 51.0 vs, 67.4 vs. 49.3 |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; EGFR, epidermal growth factor receptor; CRT, chemoradiotherapy; TRO, thoracic radiotherapy; RT, radiotherapy; TKI, tyrosine kinase inhibitor; CT, chemotherapy; NA, not available; ORR, objective response rate; PFS, progression-free survival; OS, overall survival.
5 LA-NSCLC WITH OTHER ONCOGENIC ALTERATIONS
Recent clinical explorations have focused on the treatment of LA-NSCLC harboring driver targets other than EGFR. The NAUTIKA1 trial (NCT04302025) [151] is a phase II umbrella trial investigating the efficacy and safety of neoadjuvant targeted therapies in patients who have resectable NSCLC with molecular alterations, including ALK, ROS1, NTRK, BRAF V600, and RET. Preliminary data from the ALK(+) cohort showed that no patients had radiographic disease progression or downstaging prior to surgery, and all patients underwent complete resection. The results of a retrospective study suggested that ALK-TKIs were clinically feasible for the neoadjuvant treatment of resectable stage III NSCLC, and alectinib showed a numerically superior pathological response compared with crizotinib (MPR: 56.3% vs. 30.8%, P = 0.26; pCR: 37.5% vs. 15.4%, P = 0.24). Very recently, ALINA (NCT03456076) firstly showed the superiority of 2-year adjuvant alectinib compared with adjuvant chemotherapy, with DFS HR of 0.24 (95% CI = 0.13-0.45) [152]. The LIBRETTO-432 trial (NCT04819100) explored the efficacy of adjuvant selpercatinib in patients with RET fusion-positive stage IB-IIIA NSCLC after definitive radiotherapy or surgery [153]. Clinical trials regarding LA-NSCLC with various molecular alterations are currently underway (Table 10).
| Trial | Stage and molecular alteration | No. of patients | Regimen | Primary endpoint | Estimated completion date |
|---|---|---|---|---|---|
| Adjuvant targeted therapy for resectable molecular alterations LA-NSCLC | |||||
|
ALINA (NCT03456076) |
IB-IIIA, ALK+ | 257 | Alectinib × 2 years vs. CT × 4 cycles | DFS | November 19, 2026 |
|
ALCHEMIST (NCT02201992) |
IB-IIIA, ALK+ | 168 | Crizotinib × 2 years vs. observation | OS | May 1, 2036 |
|
LIBRETTO-432 (NCT04819100) |
Definitive locoregional treatment IB-IIIA, RET+ | 170 | Selpercatinib vs. placebo until PD | EFS | November 30, 2032 |
| Neoadjuvant targeted therapy for resectable molecular alterations LA-NSCLC | |||||
|
NAUTIKA1 (NCT04302025) |
IB-III, ALK, ROS1, NTRK, BRAF V600, and RET alterations | 85 | TKIs × 8 weeks → S → CT × 4 cycles → TKIs × 2 years | MPR of TKIs; 3-5 grade AEs and participants without delayed surgery in KRAS cohort | March 6, 2029 |
|
ALNEO (NCT05015010) |
III, ALK+ | 33 | Alectinib × 8 weeks → S → alectinib × 96 weeks | MPR | May 28, 2026 |
|
SAKULA (UMIN00017906) |
II-III, ALK+ | 7 | Ceritinib × 12 weeks → S | MPR | October, 2019 |
|
Neo-KAN (NCT05472623) |
IB-IIIA, KRAS G12C+ | 42 |
Arm A: adagrasib × 6 weeks → S → CT ± RT; Arm B: adagrasib × 6 weeks+ nivolumab × 3 cycles → S → CT ± RT |
pCR | February 1, 2029 |
- Abbreviations: LA-NSCLC, locally advanced-non-small cell lung cancer; ALK, anaplastic lymphoma kinase; RET, proto-oncogene tyrosine-protein kinase receptor; TKI, tyrosine kinase inhibitors; S, surgery; CT, chemotherapy; MPR, major pathological response; pCR, pathological complete response; AE, adverse events; DFS, disease-free survival; OS, overall survival; PD, progressive disease; EFS, event free survival.
6 CONCLUSIONS
Theoretically, LA-NSCLC is likely to be cured; thus, improvements in the cure rate should be the main goal when establishing a blueprint for clinical management. Advances in ICIs and TKIs have led to rapid evolution in treatment strategies for LA-NSCLC, along with significant improvement in patient prognosis. Resectability and driver mutations, such as EGFR, are the 2 main factors for stratification of current treatment approaches and conceptualization of future trial designs.
For oncodriver-negative patients, ICI-based neoadjuvant strategies must be optimized. The use of biomarkers (e.g., MRD) to guide the identification of patients who are cured by neoadjuvant chemoimmunotherapy and surgery should also be prioritized to avoid unnecessary treatment with ICIs. The feasibility of converting patients from unresectable status to resectable status via potent neoadjuvant therapy is also a key issue that should be resolved, and a multidisciplinary tumor board plays an important role in this process. The contribution of modern radiation techniques to the perioperative scenario should be elucidated, and the efficacy of ICI rechallenge after disease relapse in the context of previous (neo)adjuvant ICI should be estimated. For patients with unresectable disease, there is a need to determine the optimal timing and sequence of ICIs to modify the PACIFIC protocol.
For patients with EGFR-mutated NSCLC, although adjuvant osimertinib provides a survival benefit, additional confirmatory evidence from real-world studies is required, along with randomized controlled trials of other third-generation EGFR-TKIs. The feasibility of EGFR-TKIs plus strategies in neoadjuvant settings should be examined. The administration of EGFR-TKIs in patients with unresectable EGFR-mutated NSCLC is another challenge. Finally, the role of targeted therapies beyond EGFR in the perioperative scenario must be fully explored.
Overall, the search for a strategy that can truly improve survival outcomes in this heterogeneous group of patients with LA-NSCLC remains a long-term challenge. However, ongoing research is contributing to the enhancement and optimization of traditional therapies. The development of novel agents will continuously improve the treatment outcomes of patients with LA-NSCLC.
AUTHOR CONTRIBUTIONS
Wen Li, Yang Xia contributed substantially to discussion of contents. Da Miao, Jing Zhao, and Ying Han contributed to the acquisition, analysis, or interpretation of data. Yang Xia, Da Miao, Jing Zhao, Ying Han, Jiaqi Zhou, Xiuzhen Li, Ting Zhang drafted and revised the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
We thank Jie Zhao (Key Laboratory of Respiratory Disease of Zhejiang Province, Department of Respiratory and Critical Care Medicine, Second Affiliated Hospital of Zhejiang University School of Medicine), and Xiaohui Chen (Department of Thoracic Surgery, Fujian Medical University Cancer Hospital, Fujian Cancer Hospital) for their valuable suggestions to this review.
CONFLICT OF INTEREST STATEMENT
All authors declare that they have no competing interests.
FUNDING INFORMATION
The study was supported by Natural Science Foundation of Zhejiang Province (LTGY23H010004); National Natural Science Foundation of China (82370028); Development Project of Zhejiang Province's “Jianbing” and “Lingyan” (2023C03067).
DECLARATIONS
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
Open Research
DATA AVAILABILITY STATEMENT
Not applicable.




