Prediction of major adverse cardiac events is the first critical task in the management of immune checkpoint inhibitor-associated myocarditis
Abbreviations
-
- CI
-
- confidence interval
-
- CMR
-
- cardiac magnetic resonance.
-
- ECG
-
- electrocardiogram
-
- ECHO
-
- echocardiography
-
- G
-
- grade
-
- HR
-
- hazard ratio
-
- ICIs
-
- immune checkpoint inhibitors
-
- irAEs
-
- immune-related adverse events
-
- LV
-
- left ventricular
-
- MACE
-
- major adverse cardiac events
-
- MDT
-
- multidisciplinary team
-
- OR
-
- odds ratio
-
- OS
-
- overall survival
-
- PUMCH
-
- Peking Union Medical College Hospital
Dear Editor,
The application of immune checkpoint inhibitors (ICIs), anti-tumor immunotherapy unleashing the host immune system to eradicate tumor cells, has revolutionized the treatment of various advanced cancers and showed remarkable anti-tumor effects [1]. However, emphasis must be placed on fatal immune-related adverse events (irAEs), especially some fulminant irAEs like ICI-related cardiovascular AEs [2, 3]. However, due to the low rate of cardiovascular AEs, little is known about the effective methods for evaluating the risk of catastrophic cardiac events in ICI-associated myocarditis and its management [4, 5].
The Peking Union Medical College Hospital (PUMCH) nationwide multidisciplinary irAE Management Task Force was founded in July 2018 (Supplemental Material). It encompasses 33 cancer centers across China. The PUMCH irAE Task Force cardio-oncology multidisciplinary team (MDT) promotes inpatient/outpatient consultation for patients with suspected cardiovascular AEs from multiple hospitals. In this study, we aimed to summarize our recent experience with ICI-associated myocarditis management and to identify indicators for major adverse cardiac events (MACE) and the association of MACE with overall survival (OS).
Between July 2018 and November 2020, 52 patients diagnosed with ICI-associated myocarditis through multidisciplinary consultation of the PUMCH irAE Task Force were enrolled for this study. According to a consensus statement of ICI-associated myocarditis [6], 20 (38.5%) participants had definite myocarditis, 13 (25.0%) had probable myocarditis, and 19 (36.5%) had possible myocarditis. Data on relevant variables were retrospectively collected. OS was defined as the primary outcome. The clinical characteristics, irAE-related information, and outcomes were compared between patients with and without MACE. The patients enrollment and assessments are detailed in the Supplementary file.
Supplementary Table S1 shows the baseline characteristics of these 52 patients. There was no difference in baseline characteristics of participants with and without MACE. The median time from initiation of ICIs to the onset of ICI-associated myocarditis was 30 days (interquartile range [IQR] 21-56 days) (Supplementary Table S2). A total of 32 (61.5%) participants had grade 3-4 myocarditis. More than half of the participants (28/52 [53.8%]) developed troponin elevation > 10 times the upper limit of the normal range. New onset arrhythmia (II-III° atrioventricular block, atrial fibrillation, ventricular arrhythmias, and so on; 30/52 [57.7%]) and dynamic ST-T changes (17/52 [32.7%]) were commonly manifested on electrocardiogram (ECG). Echocardiography (ECHO) abnormalities (wall motion abnormality, left ventricular [LV] systolic dysfunction, and so on) were detected in 18 patients (34.6%). Systemic steroid treatment was used in almost all participants (49/52 [94.2%]), and 13 (25.0%) of them received steroid pulse therapy. Details of ICI-associated myocarditis-related information are presented in Supplementary Table S2.
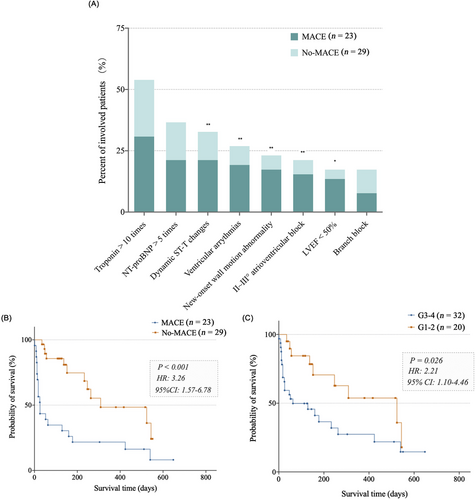
A total of 23 participants (44.2%) experienced at least one MACE. The median time from clinical myocarditis to the onset of MACE was 8 days (IQR 2-13 days). Cardiovascular death was the most common MACE (14/23 [60.9%]), followed by cardiogenic shock (12/23 [52.2%]), hemodynamically significant complete heart block (8/23 [34.8%]), and sudden cardiac arrest (3/23 [13.0%]) (data not shown). Patients who received ICI monotherapy, except those who received a combination of ICIs and chemotherapy, were more likely to experience a subsequent MACE (MACE group 13/23 [56.5%] vs. non-MACE group 7/29 [24.1%], P = 0.017). Cardiac abnormalities, including new-onset ECG anomalies, ECHO abnormalities and high levels of cardiac biomarkers, were more common in the MACE group (Figure 1A, Supplementary Table S2). Multivariate logistic regression with adjusting variates of age and ICIs as the first-line treatment revealed that dynamic ST-T changes (odds ratio [OR] = 4.43, 95% confidence interval [CI]: 1.17-16.76, P = 0.028), ventricular arrhythmias (OR = 8.72, 95% CI: 1.57-48.28; P = 0.013), II–III° atrioventricular block (OR = 6.35, 95% CI: 1.28-31.51; P = 0.024), and new-onset wall motion abnormality (OR = 5.44, 95% CI: 1.24-23.90; P = 0.025) were independent indicative factor for MACE (Supplementary Table S3). Moreover, we divided these patients into two groups according to whether they developed these ECG or ECHO abnormalities (positive group vs negative group: 24 [46.2%] vs 28 [53.8%]), and found that patients showing these abnormalities were more likely to develop MACE (16/24 [66.7%] vs 7/28 [25.0%], P = 0.003) (data not shown).
After a median follow-up of 417 days (IQR, 145-545 days), a total of 32 participants (32/52, 61.5%) in the entire cohort died (14 [26.9%] CV deaths, 12 [23.1%] tumor progression-related deaths, and 6 [11.5%] comorbidity- and/or complication-related deaths) during the follow-up period, and the median OS of all patients since onset of myocarditis was 178 days (IQR, 26-540 days). We observed that MACE (hazard ratio [HR] = 3.26; 95% CI: 1.57-6.78; P < 0.001) and high CTCAE grades (G3-4) (HR = 2.21; 95% CI: 1.10-4.46; P = 0.026) were risk factors for all-cause mortality from the Kaplan–Meier plots (Figure 1B-C). Cox regression analysis involving variates of MACE and high CTCAE grades (G3-4) after adjusting variates of age and ICIs as the first-line treatment has demonstrated that MACE was an independent risk factor for all-cause mortality (OR = 3.30; 95% CI: 1.54-7.06; P = 0.002).
For patients manifesting ICI-associated myocarditis, the determination of how to identify early and provide adequate medical care for potentially catastrophic cardiac events is necessary. To date, few effective approaches or biomarkers are proposed for MACE prediction in ICI-associated myocarditis patients. As for estimating irAEs myocarditis or related MACE, cardiac magnetic resonance (CMR) imaging is of great value [6, 7]. However, the complicated process of CMR has hindered the spread of its use for cardiac estimation in patients with severe irAEs. Although serum troponin elevation has been shown to predict the occurrence of MACE [8], serum troponin > 10 times was not shown as an independent indicative factor for MACE in our study. ECG and ECHO can be performed at any moment and at the bedside, which can be widely used for cardiac event monitoring and evaluation in patients with ICI-associated myocarditis [4, 5]. Newly occurring arrhythmias suggest that cardiotoxicity to the conducting system may result in malignant ventricular arrhythmia and severe conduction block. Dynamic ST-T changes on ECG and new ventricular wall movement abnormalities in ECHO suggest extensive electrophysiological and functional myocardial injury [9]. This multicenter retrospective study suggested that patients with ICI-related myocarditis might develop MACE when co-presenting with dynamic ST-T changes, II-IIIo atrioventricular block, ventricular arrythmias, or new-onset wall motion abnormality. Besides, MACE was further demonstrated to be an independent risk factor for reduced long-term OS in these patients. These key information points should be heeded in the clinical management of myocarditis, which indicates closer monitoring, early aggressive therapy, and effective supportive treatment.
The CTCAE grading of adverse events is widely used in clinical practice to guide treatment strategies [5]. Since MACE is associated with poor prognosis, it is indicated that adequate steroid usage (1-4 mg/kg/d methylprednisolone) or steroid pulse therapy could be used in G3 patients developing MACE and G4 patients [4, 5]. In contrast, G3 patients without MACE are not necessary to undergo steroid pulse therapy in the initial stage of irAE-related therapy, and should be closely monitored for MACE indicators. As for G1-2 patients, since MACE is rarely experienced in these patients, steroid treatment should be more conservative [10].
Several limitations existed in the current study. Firstly, being a real-world study, the ICI treatment and combined anti-cancer treatment regimens were heterogeneous; thus, it was difficult to determine the ICI treatment-related predictors for MACE. Secondly, the reporting of ICI-associated myocarditis cases was based on the clinical need to request MDT support. Therefore, it was unrepresentative of the overall status of myocarditis in these 33 centers, where some cases may have not sought such support.
In conclusion, this study revealed significant ECG and ECHO anomaly findings in ICI-associated myocarditis as indicators for MACE. Knowing that patients with these indicators may have more fatal outcomes could help clinicians make better treatment decisions, such as using steroid pulse and immunosuppressant therapies, and improve patients’ outcomes.
DECLARATIONS
AUTHOR CONTRIBUTIONS
(I) Conception and design: MZW and WW; (II) Administrative support: MZW and WW; (III) Provision of study materials or patients: MZW, WW, YX, MJC, WZ, JZ, RLP, XXG, HQ, YXL, YQS, XYL, and YJS; (IV) Collection and assembly of data: YX, YJS, and WW; (V) Data analysis and interpretation: YX and YJS; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
CONFLICT OF INTEREST DISCLOSURES
The authors have no conflicts of interest to declare.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the PUMCH review board (S-K135). As a retrospective study, the requirement for written informed consent was waived.
FUNDING
This study was supported by the Youth Program of National Natural Science Foundation of China (to YX) (82003309), by the National Key Research and Development Program of China (to WW) (2016YFC0905102), and CAMS Innovation Fund for Medical Sciences (to WW) (CIFMS) (2017-I2M-2-002).
ACKNOWLEDGMENTS
The authors thank the patients for providing their information in this study. We thank all the experts in managing irAEs in the PUMCH multidisciplinary irAE Task Force. We greatly appreciate all the physicians in the 33 cancer centers for their intensive treatment of ICI-associated myocarditis patients.




