New insights into molecules and pathways of cancer metabolism and therapeutic implications
Abstract
Cancer cells are abnormal cells that can reproduce and regenerate rapidly. They are characterized by unlimited proliferation, transformation and migration, and can destroy normal cells. To meet the needs for cell proliferation and migration, tumor cells acquire molecular materials and energy through unusual metabolic pathways as their metabolism is more vigorous than that of normal cells. Multiple carcinogenic signaling pathways eventually converge to regulate three major metabolic pathways in tumor cells, including glucose, lipid, and amino acid metabolism. The distinct metabolic signatures of cancer cells reflect that metabolic changes are indispensable for the genesis and development of tumor cells. In this review, we report the unique metabolic alterations in tumor cells which occur through various signaling axes, and present various modalities available for cancer diagnosis and clinical therapy. We further provide suggestions for the development of anti-tumor therapeutic drugs.
Abbreviations
-
- 1-MT
-
- 1-methyl tryptophan
-
- 2DG
-
- 2-deoxyglucose
-
- 3-BP
-
- 3-bromopyruvat
-
- AEA
-
- endocannabinoids anandamide
-
- AML
-
- acute myeloid leukemia
-
- AMPK
-
- AMP-activated protein kinase
-
- AR
-
- adrenergic receptor
-
- ASNase1
-
- asparaginase 1
-
- ASS1
-
- argininosuccinate synthetase 1
-
- AXIN
-
- axis inhibition protein
-
- BA
-
- bile acid
-
- BCAR4
-
- breast cancer anti-estrogen resistance 4
-
- CAC
-
- colitis-associated cancer
-
- CAD
-
- carbamoyl-phosphate synthetase 2, aspartate transcarbamylase and dihydrooratase
-
- CAF
-
- cancer-associated fibroblast
-
- CCAR1
-
- cell division cycle and apoptosis regulator protein 1
-
- CKB
-
- creatine kinase, brain-type
-
- CRC
-
- colorectal cancer
-
- CRL
-
- cullin-RING E3 ligase
-
- CRP
-
- C-reactive protein
-
- CSC
-
- cancer stem cell
-
- CTP
-
- citrate transporter protein
-
- CUEDC2
-
- CUE domain-containing protein 2
-
- D2HG
-
- D-2-hydroxyglutarate
-
- DCA
-
- deoxycholic acid
-
- EDP
-
- epoxydocosapentaenoic acid
-
- EGFR
-
- epidermal growth factor receptor
-
- EMT
-
- epithelial-mesenchymal transition
-
- ER
-
- endoplasmic reticulum
-
- ERα
-
- estrogen receptor α
-
- EV
-
- extracellular vesicle
-
- FXR
-
- farnesoid X receptor
-
- G6PD
-
- glucose-6-phosphate dehydrogenase
-
- GAPDH
-
- glyceraldehyde-3-phosphate dehydrogenase
-
- GBM
-
- glioblastoma multiforme
-
- GBTC
-
- gallbladder and biliary tract cancer
-
- Gln
-
- glutamine
-
- GLUT3
-
- glucose transporter 3
-
- GPT2
-
- glutamic pyruvate transaminase 2
-
- GR
-
- glucocorticoid receptor
-
- HCC
-
- hepatocarcinoma
-
- HCV
-
- hepatitis C virus
-
- HISLA
-
- HIF-1alpha-stabilizing lncRNA
-
- HK2
-
- hexokinase 2
-
- HMGCL
-
- 3-hydroxy-3-methylglutaryl-CoA lyase
-
- HMOX1
-
- heme oxygenase 1
-
- HMW
-
- high-molecular-weight
-
- HSP90
-
- heat shock protein 90
-
- IBD
-
- intrahepatic bile duct
-
- IDH
-
- isocitrate dehydrogenase
-
- IDH1
-
- isocitrate dehydrogenase 1
-
- IDH2
-
- isocitrate dehydrogenase 2
-
- IDO
-
- indoleamine 2,3-dioxygenase
-
- IL-6
-
- interleukin-6
-
- KDM8
-
- lysine demethylase 8
-
- KYN
-
- trigger kynurenine
-
- LAPTM4B
-
- lysosomal protein transmembrane 4 beta
-
- LDH
-
- lactate dehydrogenase
-
- LDHA
-
- lactate dehydrogenase A
-
- LIC
-
- leukemia-initiating cell
-
- lncRNA
-
- long non-coding RNA
-
- LSC
-
- leukemia stem cell
-
- lysoPC
-
- lysophosphatidylcholine
-
- MCT1
-
- monocarboxylate transporter-1
-
- MM
-
- multiple myeloma
-
- MPC
-
- mitochondrial pyruvate carrier
-
- mTOR
-
- mammalian target of rapamycin
-
- mTORC2
-
- mTOR complex 2
-
- NMDA
-
- N-methyl-D-aspartic acid
-
- NNMT
-
- methyltransferase nicotinamide N-methyltransferase
-
- NSCLC
-
- non-small cell lung carcinoma
-
- NSE
-
- neuron-specific enolase
-
- OOA
-
- oxaloacetic acid
-
- OXCT1
-
- 3-oxoacid CoA-transferase 1
-
- PCK1
-
- phosphoenolpyruvate carboxykinase 1
-
- PCK2
-
- phosphoenolpyruvate carboxykinase 2
-
- PDAC
-
- pancreatic ductal adenocarcinoma
-
- PDGFRA
-
- platelet-derived growth factor receptor alpha
-
- PDH
-
- pyruvate dehydrogenase
-
- PDK1
-
- pyruvate dehydrogenase kinase 1
-
- PDK2
-
- pyruvate dehydrogenase kinase isozyme 2
-
- PD-L1
-
- programmed death-ligand 1
-
- PEA
-
- palmitylethanolamide
-
- PEP
-
- phosphoenolpyruvate
-
- PFKFB3
-
- 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3
-
- PFKFB4
-
- 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 4
-
- PHD2
-
- prolyl hydroxylase 2
-
- PHGDH
-
- phosphoglycerate dehydrogenase
-
- pHGG
-
- pediatric high-grade glioma
-
- PI3K
-
- phosphoinositide 3-kinase
-
- PKB
-
- protein kinase B
-
- PKM2
-
- pyruvate kinase M2
-
- Plk1
-
- polo-like kinase 1
-
- PP1
-
- protein phosphatase 1
-
- PP2A
-
- protein phosphatase 2A
-
- PPAR
-
- peroxisome proliferator-activated receptor
-
- PPP
-
- pentose phosphate pathway
-
- PRMT5
-
- protein arginine methyltransferase 5
-
- PUMA
-
- p53 upregulated modulator of apoptosis
-
- R5P
-
- ribose 5-phosphate
-
- RIF1
-
- replication timing regulatory factor 1
-
- ROS
-
- reactive oxygen species
-
- SCC
-
- squamous cell carcinoma
-
- SDH
-
- serine dehydratase
-
- SIRT5
-
- sirtuin5
-
- SNS
-
- sympathetic nervous system
-
- SRC-3
-
- steroid receptor coactivator-3
-
- SREBP
-
- serol regulatory element-binding protein
-
- SRSF5
-
- serine and arginine-rich splicing factor 5
-
- STAT3-Socs3
-
- signal transducers and activators of transcription 3-suppressor of cytokine signaling 3
-
- TAM
-
- tumor-associated macrophage
-
- T-betaMCA
-
- tauro-beta-muricholic acid
-
- TCA
-
- tricarboxylic acid
-
- TFEB
-
- transcription factor EB
-
- TGF-β
-
- transforming growth factor-beta
-
- TIL
-
- tumor-infiltrating T-lymphocyte
-
- TKT
-
- transketolase
-
- TME
-
- tumor microenvironment
-
- Trp
-
- tryptophan
-
- UC
-
- urea cycle
-
- UGDH
-
- UDP-glucose 6-dehydrogenase
-
- VEGF
-
- vascular endothelial growth factor
-
- WTp53
-
- wild-type p53
-
- YAP
-
- Yes-associated protein
-
- ZIP14
-
- ZRT- and IRT-like protein 14
1 INTRODUCTION
The Warburg effect (aerobic glycolysis) indicates that tumor cells prefer high-activity glycolysis to meet their survival demands [1]. However, until recently, this pathologic phenomenon has not been extensively researched and discussed. An epoch-making finding revealed that 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 4 (PFKFB4), a leading metabolic enzyme, activates glycolysis steroid receptor coactivator-3 (SRC-3) transcriptional activity and drives glucose flux towards the pentose phosphate pathway (PPP) functionally, which explains why tumors do not show active mitochondrial metabolic activity (Table 1) [2]. High tumor-associated glucose consumption frequently involves alterations at both molecular and cellular levels, which drive the malignant features of solid tumors. Thus, such metabolic pathways provide promising clinical targets.
| Metabolic enzyme | Cancer type | Function | Reference |
|---|---|---|---|
| PFKFB4 | Breast cancer | Activate the transcriptional activity of SRC-3 and drive the pentose phosphate pathway. | Dasgupta et al., 2018 [2] |
| TRIM11 | Sustain the ubiquitination of estrogen receptor αand metastasis behavior. | Tang et al., 2020 [76] | |
| PHGDH | Breast cancer | Decrease the integration with nucleotides of one-carbon units. | Pacold et al., 2016 [91] |
| Breast cancer | Support tumorigenesis in serine-limited conditions. | Sullivan et al., 2019 [89] | |
| Melanoma | |||
| PCK2 | Melanoma | PCK2 deletion regulates glucose metabolism and alleviates oxidative phosphorylation. | Luo et al., 2017 [22] |
| HMGCL | Melanoma | Respond to the MEK-ERK pathway and induce acetoacetate production. | Kang et al., 2015 [63] |
| Leukemia | |||
| PCK1 | Melanoma | Activate T cells to overexpress glycolytic phosphoenolpyruvate. | Ho et al., 2015 [26] |
| Hepatocarcinoma | Prevent INSIG1/2 from integrated with intracellular lipid and trigger sterol regulatory element-binding protein signaling. | Xu et al, 2020 [60] | |
| PFKFB3 | Breast cancer | Trigger mitotic-associated translation and oxidative respiration. | Domenech et al., 2015 [5] |
| Cervical cancer | Prevent DNA from degradation and sustain glycolysis. | Li et al., 2018 [11] | |
| Plk1 | Cervical cancer | Support the pentose phosphate pathway and increase macromolecules' biosynthesis. | Ma et al.,2017 [4] |
| G6PD | Osteosarcoma | Trigger NADPH and ribose synthesis and attenuated reactive oxygen species. | Du et al., 2013 [52] |
| ASNase1 | Allow conversion between asparagine and aspartate. | Sullivan et al., 2018 [99] | |
| UGDH | Lung cancer | Induce epithelial-mesenchymal transition and metastatic growth. | Wang et al., 2019 [6] |
| GAPDH | Respond to glucose signal. | Li et al., 2014 [12] | |
| PP1 | Dephosphorylate axis inhibition protein and stimulate Wnt/β-catenin signaling. | Mei et al., 2018 [71] | |
| HMOX1 | Stabilize Bach1 and support metastasis. | Lignitto et al., 2019 [126] | |
| CKB | Colorectal cancer | Induce liver-colonization. | Loo et al., 2015 [7] |
| GLUD1 | Facilitate glutamine to be incorporated into the tricarboxylic acid cycle. | Wang et al., 2018 [79] | |
| GPT2 | Colon cancer | Regulate glutamine catabolism. | Smith et al., 2016 [80] |
| HK2 | Lung cancer | Promote the Warburg effect. | Kim et al., 2019 [25] |
| Glioblastoma | Impair central nervous system with activated glycolysis and mitochondrial translocation | Wolf et al., 2011 [13] | |
| Cdc25A | Glioblastoma | Sustain glycolysis. | Liang et al., 2016 [9] |
| IDH1 mutant | Glioblastoma/glioma | Impair chromosomal topology and activate platelet-derived growth factor receptor alpha. | Flavahan et al.,2016 [42] |
| Induce D2HG production to trigger neuronal activity. | Chen et al., 2017 [43] | ||
| Alleviate pyruvate dehydrogenase phosphorylation, upregulate HIF-1 and pyruvate dehydrogenase kinase-3, and induce glutamate generation. | Izquierdo-Garcia et al., 2015 [45] | ||
| PKM2 | Ovarian cancer | Control glycolytic rate. | Chao et al., 2017 [14] |
| Methyltransferase nicotinamide N-methyltransferase | Induce cancer-associated fibroblast phenotype alterations and cause depletion of S-adenosyl methionine. | Eckert et al., 2019 [95] | |
| PDK2 | Leukemia | Regulate glycolysis, home leukemia-initiating cells, and trigger symmetric cell division. | Hao et al., 2019 [15] |
| KDM8 | Prostate cancer | Interact with pyruvate kinase M2 and modulate glycolytic gene activities under hypoxic conditions. | Wang et al., 2019 [17] |
| CAD | Prostate cancer | Induce both pyrimidine synthesis and transversion mutations at the nucleic acid and protein levels. | Lee et al.,2018 [116] |
| Lung cancer | |||
| Breast cancer | |||
| LDHA | Hepatocarcinoma | Modulate aerobic glycolysis. | Zhong et al., 2017 [16] |
| PDK1 | Regulate the tricarboxylic acid cycle in hypoxia-inducible factor-1 independent pathway. | Ma et al., 2014 [18] | |
| PRMT5 | Activate the sterol regulatory element-binding protein methylation and lipogenesis. | Liu et al., 2016 [59] | |
| OXCT1 | Drive ketone metabolism to the tricarboxylic acid cycle and inactivate AMP-activated protein kinase. | Huang et al., 2016 [62] | |
| TKT | Regulate R5P expression and nucleotide synthesis. | Li et al., 2019 [51] | |
| P5C synthase and P5C reductase 1 | Kidney cancer | Direct proline biosynthesis from glutamine. | Liu et al., 2012 [82] |
| Prostate cancer | |||
| Burkitt lymphoma | |||
| Cytochrome c oxidase | Pancreatic cancer | Mediate oxidative phosphorylation and ATP production. | Ishida et al., 2013 [114] |
| SDH | Induce pyruvate production. | Yu et al., 2019 [90] | |
| PP2A | Gastric cancer | Target MST1/2, trigger YAP signaling and suppress the Hippo tumor suppressor with the regulatory subunit, STRN3. | Tang et al., 2020 [73] |
| CRLs | Colitis-associated cancer | Induce ST7 ubiquitination in an inflammatory tumor microenvironment. | Liu et al., 2019 [77] |
| IDO | Multiple myeloma | Block T cells and decrease antitumor bioactive substances production. | Yan et al., 2019 [101] |
| LDH | Squamous cell carcinoma | LDH defectiveness sustains glycolysis. | Flores et al., 2019 [33] |
- Abbreviations: ASNase1, asparaginase 1; CAD, carbamoyl-phosphate synthetase 2, aspartate transcarbamylase and dihydrooratase; CKB, creatine kinase, brain-type; CRL, cullin-RING E3 ligase; G6PD, glucose-6-phosphate dehydrogenase; GAPDH, glyceraldehyde-3-phosphate dehydrogenase; GLUD1, glutamate dehydrogenase 1; GPT2, glutamic pyruvate transaminase 2; HK2, hexokinase 2; HMGCL, 3-hydroxy-3-methylglutaryl-CoA lyase; HMOX1, heme oxygenase 1; IDH1, isocitrate dehydrogenase 1; IDO, indoleamine 2,3-dioxygenase; KDM8, lysine demethylase 8; LDH, isocitrate dehydrogenase.; LDHA, lactate dehydrogenase A; OXCT1, 3-oxoacid CoA-transferase 1; PCK1, phosphoenolpyruvate carboxykinase 1; PCK2, phosphoenolpyruvate carboxykinase 2; PDK1, pyruvate dehydrogenase kinase 1; PDK2, pyruvate dehydrogenase kinase isozyme 2; PFKFB3, 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3; PFKFB4, 6-phosphofructo-2-kinase/fructose-2,6-bisphosphatase 4; PHGDH, phosphoglycerate dehydrogenase; PKM2, pyruvate kinase M2; Plk1, polo-like kinase 1; PP1, protein phosphatase 1; PP2A, protein phosphatase 2A; PRMT5, protein arginine methyltransferase 5; SDH, serine dehydratase; TKT, transketolase; TRIM11, tripartite motif containing 11; UGDH, UDP-glucose 6-dehydrogenase.
Cancer cells possess multiple prime metabolic signaling pathways, sometimes re-routing glucose flux consumption to other metabolic pathways, which contributes to maintain an aerobic microenvironment in the tumor. For example, unlike proliferating leukemia cell populations that switch cellular respiration to aerobic glycolysis, oxidative phosphorylation, and proliferation pathways of leukemia stem cells (LSCs) are very reliant on amino acid metabolism [3]. We have previously reported that regulatory alterations of the metabolic network in cancer cells extend beyond the Warburg effect and individual metabolic flux. Thus, it is imperative to interrogate the metabolome of tumors to elucidate the properties associated with clinical intervention. In this review, we summarize the unique metabolic alterations in tumor cells which occur through various signaling axes. Based on these metabolic alterations, we present various modalities available for cancer diagnosis and clinical therapy and further provide suggestions for the development of anti-tumor therapeutic drugs.
2 GLUCOSE METABOLISM
2.1 Phosphorylation
Phosphorylation is vital to coordinate cancer metabolism as well as the biosynthesis of cancer-related metabolites. Ma et al. [4] showed that the active dimer of polo-like kinase 1 (Plk1) and phosphorylated glucose-6-phosphate dehydrogenase (G6PD) caused sustained activation of the PPP and resulted in increased biosynthesis of macromolecules in HeLa cells (cervical cancer cells cultured in vitro) (Table 1). Additionally, the metabolic enzyme 6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 (PFKFB3) is highly regulated by phosphorylation. In breast cancer cells, it has been reported that prolongation of mitotic arrest causes AMP-activated protein kinase (AMPK)-dependent phosphorylation of PFKFB3, and thereby induce mitosis-associated translation. This results in an increase in glycolysis which replaces oxidative respiration in breast cancer (Table 1) [5].
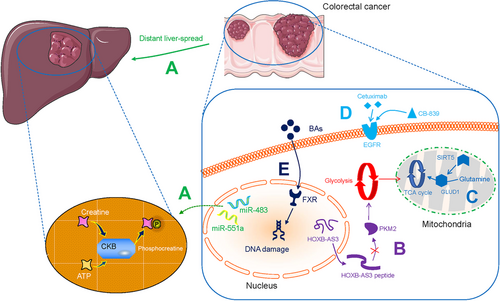
Phosphorylation often accelerates cancer invasion and metastasis. Wang et al. [6] found that the activation of epidermal growth factor receptor (EGFR) in metastatic lung cancer induced the phosphorylation of UDP-glucose 6-dehydrogenase (UGDH) at tyrosine 473 and stimulated the expression of SNAI1 mRNA; activated EGFR also promoted epithelial-mesenchymal transition (EMT) (Table 1). Loo et al. [7] identified multiple miRNAs, including miR-551a and miR-483, which stimulated creatine kinase, brain-type (CKB) and thereby induced the phosphorylation of creatine to produce phosphocreatine, leading to sustained ATP production and the colonization of colorectal cancer (CRC) cells in the liver (Table 1 and Figure 1A).
Phosphorylation is also associated with converting physiological signaling factors to cancer-promoting factors. Kim et al. [8] showed that the nuclear oncogenic wild-type p53 (WTp53) downregulated pyruvate-directed oxidative phosphorylation by triggering a p53 upregulated modulator of apoptosis (PUMA)-inactivated mitochondrial pyruvate carrier (MPC) in hepatocarcinoma (HCC; Figure 2A). Liang et al. [9] discovered that the phosphatase Cdc25A is activated by phosphorylation at Y59 by EGFR-c-Src signaling, and regulates the cell cycle. They further demonstrated that the activated Cdc25A sustains glycolysis and is related to the grades of human glioblastoma malignancy (Table 1). Phosphorylation-dependent networks cause metabolic abnormalities and instigate malignancies, and thus can be explored to identify potential therapeutic targets.

2.2 Acetylation
Acetylation of various targets promotes cancer development and is thought to occur as a response to glucose consumption. Chen et al. [10] discovered that serine and arginine-rich splicing factor 5 (SRSF5) was hyperacetylated in lung carcinoma, blocked Smurf1-coordinated ubiquitylation, sustained the splicing of cell division cycle and apoptosis regulator protein 1 (CCAR1), and responded to increased acetyl CoA biosynthesis and upregulated glucose consumption. Li et al. [11] demonstrated that cisplatin triggered the acetylation of accumulated PFKFB3 in the cytoplasm, contributing to the prevention of DNA degradation in glycolytic HeLa cells (Table 1). Li et al. [12] proposed that acetylation at lysine 254 increased glyceraldehyde-3-phosphate dehydrogenase (GAPDH) activity, and responded to intracellular glucose consumption in lung cancer (Table 1). Therefore, acetylation significantly supports cancer cell proliferation and aggressive invasion.
2.3 Enzyme catalysis
Aberrant overexpression of glycolysis-associated enzymes in tumor tissue is common and is associated with the Warburg effect. In human glioblastoma multiforme (GBM), hexokinase 2 (HK2) promotes the migration of chemotherapy-resistant GBM cells into the central nervous system, this effect is associated with protein kinase B (PKB)-stimulated glycolysis and mitochondrial translocation (Table 1) [13]. In ovarian cancer, pyruvate kinase M2 (PKM2) has been shown to control glycolytic rate (Table 1) [14]. In leukemia, pyruvate dehydrogenase kinase isozyme 2 (PDK2) in the bone marrow regulates the levels of glycolysis and recruits leukemia-initiating cells (LICs), which triggers symmetric cell division (Table 1) [15]. Multiple glycolysis enzymes jointly coordinate the Warburg effect. For example, Zhong et al. [16] proposed that the CUE domain-containing protein 2 (CUEDC2) is regulated by the glucocorticoid receptor (GR)-glucose transporter 3 (GLUT3) peptide axis as well as the 14-3-3ζ-lactate dehydrogenase A (LDHA) pathway, and promotes the conversion of pyruvate to be converted to lactate in HCC (Table 1, Figure 2B and Figure 3).
Furthermore, the concentration of oxygen in the tumor microenvironment (TME) affects glycolytic enzymes indirectly. Wang et al. [17] found that the histone lysine demethylase lysine demethylase 8 (KDM8) interacts with PKM2 and subsequently modulates hypoxia-inducible factor-1 alpha (HIF-1α) to upregulate glycolytic gene activities in prostate cancer cells under hypoxic conditions (Table 1). Furthermore, Ma et al. [18] reported that aberrantly expressed Lin28A and Lin28B and decreased let-7 results in upregulating pyruvate dehydrogenase kinase 1 (PDK1) in the HIF-1 independent pathway and modulating tricarboxylic acid (TCA) cycle in the aerobic tumor environment of HCC (Table 1 and Figure 2C). Proliferating tumors enable the Warburg effect in both ambient oxygen levels and in the anaerobic TME via glycolytic-associated genes and enzymes. Previously, this aspect has received little attention.
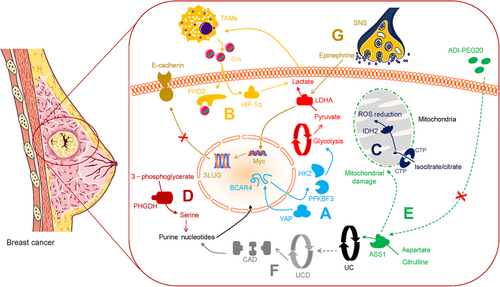
2.4 Glycolysis and long non-coding RNAs (lncRNAs)
lncRNAs are RNA molecules that are not translated into proteins. However, they regulate the metabolic characteristics of cancers such as CRC. Tang et al. [19] discovered that in CRC cells, upregulated lncRNA GLCC1 in conditions of glucose depletion protected the ubiquitination of c-MYC transcriptional factor by integration with heat shock protein 90 (HSP90). In addition, the peptides encoded by lncRNAs are involved in regulating metabolism in CRC tumor cells. The lncRNA, HOXB-AS3-encoded peptide (HOXB-AS3 peptide) inhibited the expression of PKM2 and downregulated glycolysis, suggesting that HOXB-AS3 peptide deficiency is a critical oncogenic event in CRC (Figure 1B) [20]. Zheng et al. [21] found that Yes-associated protein (YAP)-upregulated lncRNA breast cancer anti-estrogen resistance 4 (BCAR4), coordinated Hedgehog signaling and enhanced the transcription of HK2 and PFKFB3 to generate secretory lactate (Figure 4A). These observations not only validate lncRNAs as regulators of tumors with potential clinical value but also reveal regulatory mechanisms for controlling tumors proliferation and energy metabolism.
2.5 Glycolysis and mitochondria
The unique metabolic profile of cancer cells is characterized by suppressed mitochondrial glucose oxidation. Luo et al. [22] demonstrated that reduced mitochondrial phosphoenolpyruvate carboxykinase 2 (PCK2) led to glucose carbon flow via oxaloacetic acid (OOA)-malate-pyruvate and acetyl-CoA-fatty acid axis and suppressed the oxidative phosphorylation in melanoma (Table 1). Altered mitochondrial metabolism is a crucial factor in pediatric high-grade gliomas (pHGGs). Shen et al. [23] found that dichloroacetate can stimulate mitochondrial oxidation and reduce the Warburg effect, and consequently interrupt the metabolism of tumor cells (Table 2). Reversing mitochondrial oxidation suppression holds promise in metabolic oncology.
| Anti-tumor effector | Molecular mechanism | Reference |
|---|---|---|
| Dichloroacetate | Reduce the Warburg effect. | Shen et al., 2020[23] |
| 2DG | Combining 2DG with rapamycin inhibits glycolysis. | Zhao et al., 2016 [37] |
| Clomifene | Induce mutant enzyme downregulations and occupy the allosteric site of mutations. | Zheng et al., 2017 [47] |
| Enasidenib | Enhance molecular remissions and mitigate hematopoietic differentiation damage in acute myeloid leukemia. | Stein et al., 2019 [48] |
| AGI-5198 | Decrease D2HG, inhibit metastasis, impair cell cycling, and activate apoptosis in chondrosarcoma. | Li et al., 2015 [49] |
| Polydatin | Act as glucose-6-phosphate dehydrogenase inhibition and block pentose phosphate pathway. | Mele et al., 2018 [54] |
| EDPs | Block angiogenesis as well as endothelial cell transmission and vascular endothelial growth factor receptor 2-induced protease generation. | Zhang et al., 2013 [68] |
| Hakai | Inhibit E-cadherin ubiquitination and suppress EMT | Martinez-Iglesias et al., 2020 [78] |
| CB-839 | Improve therapeutic efficacy in cetuximab-resistant colorectal cancer. | Cohen et al., 2020 [86] |
| Combining arsenic trioxide or homoharringtonine with CB-839 decreases glutathione synthesis and upregulate mitochondrial reactive oxygen species | Gregory et al., 2019 [87] | |
| 1-MT | Improve the therapeutic efficacy of Doxorubicin in cancer treatment. | Lan et al., 2020 [102] |
| ADI-PEG20 | Induce argininosuccinate synthetase deprivation. | Huang et al., 2013 [104] |
| Be sensitive to prostate cancer cells with mitigated argininosuccinate synthetase and suppress early protective autophagy. | Kim et al., 2009 [105] | |
| Induce autophagy-dependent death of breast cancer cells with the loss of argininosuccinate synthetase 1. | Qiu et al., 2014 [106] | |
| Vitamin D/25-hydroxyvitamin D | Decrease the risk of colorectal cancer and induce an immune response. | Song et al., 2016 [110, 111] |
| Promote T-cell function and decrease inflammation of tumor microenvironment in breast cancer. | Karkeni et al., 2019 [112] | |
| Propranolol | Synergize with anti-cancer vaccine in cancer immunotherapies | Daher et al., 2019 [123] |
- Abbreviations: 2DG, 2-deoxyglucose; EDP, epoxydocosapentaenoic acid; EMT, epithelial-mesenchymal transition.
2.6 Glycolysis and T-cell
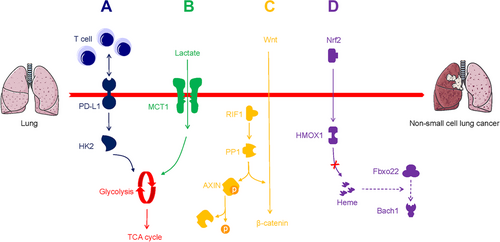
It is acknowledged that aerobic glycolysis restricts T-cell-mediated tumoricidal effector functions. Li et al. [24] reported that CD147 sustained the Warburg effect in HCC through the phosphoinositide 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) axis, which is correlated with T-cell immunosuppression (Figure 2D). Kim et al. [25] found that programmed death-ligand 1 (PD-L1) triggered HK2 to promote the Warburg effect in non-small cell lung carcinoma (NSCLC), a low expression of CD8+ T-cell function-associated genes was noted (Figure 5A and Table 1). However, aerobic glycolysis promotes effector T-cells from immunopathological impairments triggered by the TME. Ho et al. [26] validated that T-cells overexpressed the glycolytic metabolite phosphoenolpyruvate (PEP) in melanoma via phosphoenolpyruvate carboxykinase 1 (PCK1) activity, which bolstered T-cell functions (Table 1). Further exploration of metabolic checkpoints for T-cells could contribute to the elucidation of new forms of tumor immunity.
2.7 Glycolysis and macrophage
The TME contains abundant infiltrating immune cells, including tumor-associated macrophages (TAMs) [27]. Chen et al. [28] reported that to sustain the Warburg effect in breast cancer, extracellular vesicles (EVs) delivered HIF-1alpha-stabilizing lncRNA (HISLA), which antagonized the binding of prolyl hydroxylase 2 (PHD2) to HIF-1α to stabilize HIF-1α (Figure 4B). This consequently led TAM to sustain aerobic glycolysis and exhibit anti-apoptotic ability, while secretory lactate remarkably upregulated HISLA in TAMs reciprocally. In addition, metastatic lung adenocarcinoma-derived lactate stimulated mTORC1/transcription factor EB (TFEB)/ATP6V0d2/HIF-2α and promoted the expression of vascular endothelial growth factor (VEGF) [29]. Within the TME, altered TAMs acquire invasive properties which can be correlated with aerobic glycolysis.
2.8 Glycolysis and cancer stem cell (CSC)
CSCs possess self-renewal properties and the capability to differentiate into various tumor cell subpopulations [30]. Due to the Warburg effect, a high level of glucose depletion is observed in the TME. Tumor cells tend to increase stem cells phenotype to adapt to microenvironmental changes [31]. Significantly, the Warburg effect is implicated in the invasive activity of CSCs. Luo et al. [32] validated the critical role of breast CSCs, and showed that in these cells glycolysis was active while under dormancy, whereas antioxidant responses were exhibited in the proliferating state. These observations suggest that the metabolic vulnerabilities of CSCs may provide novel ways to target cancer cells.
2.9 Glycolysis and lactate metabolism
Recently many approaches have been attempted to target the Warburg effect, though valid therapeutic outcomes were not achieved. Flores et al. [33] reported that squamous cell carcinoma (SCC) cells with defective activity of lactate dehydrogenase (LDH) showed decreased glucose uptake and glycolytic metabolite production (Table 1). It is possible that tumorigenesis does not require active aerobic glycolysis, which overrides the dogma that tumors must rely on high glucose metabolically. Faubert et al. [34] provided evidence to prove that compared with glucose, lactate was the dominant carbon source for the TCA cycle in NSCLC, and was transported using the monocarboxylate transporter-1 (MCT1; Figure 5B). Hensley et al. [35] observed and further identified the value of lactate as an available non-glucose carbon source in well-perfused tumor areas. These studies strongly indicate that tumors can use lactate as a fuel in vivo, and may not rely exclusively on aerobic glycolysis.
2.10 The promise of glucose metabolism-glycolysis inhibition
Targeting aerobic glycolysis has become a promising chemotherapeutic strategy in the clinic. The glycolysis inhibitor 2-deoxyglucose (2DG) is a potent anti-cancer agent, and can function as an adjuvant drug in chemotherapy [36]. Zhao et al. [37] reported that rapamycin inhibited mTORC1 with LDHA downregulation, and the combination of rapamycin with 2DG potently influenced glycolysis in malignancies (Table 2). Nonetheless, glycolysis inhibitors including 2DG have not been used in clinical applications owing to nonspecific distribution to tumor tissue, and low bioavailability. Dong et al. [38] developed a nanoplatform that could target cancer cells and further modulate the TME based on photodynamic therapy and 2DG-triggered endoplasmic reticulum (ER) stress. Zhang et al. [39] designed a liposomal nanocarrier that readily transmitted 3-bromopyruvate (3-BP), another glycolysis inhibitor, into cancer cells without distinct side effects. Delivering glycolysis inhibitors using nanoscale functional materials represents a crucial step forward in the precise treatment of malignancies.
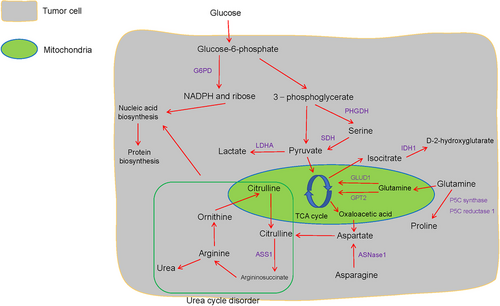
2.11 Mutant isocitrate dehydrogenase (IDH)-dependent pathway
Previously, an isocitrate dehydrogenase 1 (IDH1) mutant subset was reported in prostate cancer [40]. Cytosolic IDH mutations that convert isocitrate into D-2-hydroxyglutarate (D2HG) initiate events that allow primary clinical detection and prognosis prediction in gliomas (Figure 3) [41]. Flavahan et al. [42] identified IDH mutants that contribute to gliomagenesis via impaired chromosomal topology and trigger activities of the platelet-derived growth factor receptor alpha (PDGFRA) oncogene (Table 1). Chen et al. [43] discovered that D2HG induced neuronal activity by simulating the binding of glutamate to the N-methyl-D-aspartic acid (NMDA) receptor, and indicated that the IDH1 mutant caused a high risk of seizures in glioma patients (Table 1). Jiang et al. [44] reported that isocitrate/citrate could enter the mitochondria via the citrate transporter protein (CTP), this metabolite was involved in isocitrate dehydrogenase 2 (IDH2)-induced oxidation, resulting in NADPH production, reactive oxygen species (ROS) stress downregulation, and stabilized the TME in lung, colon, and breast cancer (Figure 4C). Also, Izquierdo-Garcia et al. [45] proposed that IDH1 mutations inhibited the pyruvate dehydrogenase (PDH) phosphorylation, upregulated HIF-1 and pyruvate dehydrogenase kinase-3 in glioblastoma cells, and reprogrammed pyruvate metabolism to aid glutamate generation (Table 1).
Significantly, Okoye-Okafor et al. [46] revealed that inhibitors of mutant IDH1 contributed to D-2HG reduction, myeloid differentiation, and granulocytic differentiation regulated by precursor cells in acute myeloid leukemia (AML). Zheng et al. [47] also showed that clomifene, an IDH1 mutant inhibitor, occupied the allosteric site of mutations in a dose-dependent non-competitive manner, and led to the downregulation of the mutant enzyme (Table 2). Another oral IDH2 mutant inhibitor, Enasidenib, is reported to enhance molecular remissions and mitigate hematopoietic differentiation damage in patients with AML (Table 2) [48]. IDH mutations are also present in chondrosarcoma. Li et al. [49] indicated that another dose-dependent IDH1 mutant inhibitor, AGI-5198, decreased the level of D-2HG, downregulated colony formation and metastasis, derailed cell cycle regulation, and activated apoptosis (Table 2). In short, the therapeutic effects of novel mutant IDH inhibitors are very useful for cancer patients displaying mutations in IDH.
2.12 PPP
The PPP physiologically regulates redox homeostasis via G6PD that transforms glucose-6-phosphate and contributes to ribose-5-phosphate and NADPH production (Figure 3) [50]. Though PPP is related to the Warburg effect, its precise role in cancer metabolism remains unclear. Li et al. [51] reported that transketolase (TKT), which is a part of a branch of the PPP that is known to sustain HCC progression, modulates ribose 5-phosphate (R5P) expression and nucleotide synthesis (Table 1 and Figure 2E). Du et al. [52] found that the p53 family member TAp73 activates the expression of the G6PD and triggers the biosynthesis of NADPH and ribose with attenuated ROS in osteosarcoma (Table 1 and Figure 3). Importantly, the PPP also plays a critical role in the regional spread and distant metastasis of cancers. McDonald et al. [53] revealed that the oxidative branch of the PPP propelled regional migration, while its suppression partly alleviated chromatin rewiring, oncogenic gene activity, and tumorigenesis in pancreatic ductal adenocarcinoma (PDAC). This indicates that an increase in PPP flux promotes tumor proliferation via a metabolic-epigenetic signaling pathway. Clinical analysis indicates that PPP blockade can be recognized as a reliable anti-tumor tool and the G6PD inhibitor polydatin functions as a novel anti-PPP agent of cancers, such as tongue cancer [54] (Table 2).
3 LIPID METABOLISM
3.1 Oncogenic effect
Lipid metabolism is a critical event in the survival of malignancies [55-57]. Serol regulatory element-binding protein (SREBP) has been historically recognized as a crucial element in lipid metabolism [58]. Liu et al. [59] proposed that SREBP activated high-level de novo lipogenesis in HCC via protein arginine methyltransferase 5 (PRMT5)-mediated methylation, which prevented ubiquitin-proteasome-mediated degradation of SREBP (Table 1). Xu et al. [60] reported that activated PCK1 prevented INSIG1/2 from complexing with intracellular lipid and trigged SREBP signaling related to lipogenesis in HCC, suggesting that SREBP has a central role in lipid metabolism (Table 1). However, in lung adenocarcinoma, hepatic metabolism is reprogrammed through an altered pro-inflammatory response via signal transducers and activators of transcription 3-suppressor of cytokine signaling 3 (STAT3-Socs3) signaling, with the disruption of AKT, AMPK, and SREBP signaling, altered lipid metabolism is noted in these cells [61]. Active tumors present hyperactivation of lipid metabolism and reprogramming of physiological metabolic processes in distant organs.
Huang et al. [62] found that in HCC cells under nutrient stress, mitochondrial ketolytic promoter 3-oxoacid CoA-transferase 1 (OXCT1) was activated by serum starvation-stimulated mTOR complex 2 (mTORC2)-AKT axis, and drove ketone metabolism to the TCA cycle, while also inactivating AMPK. This observation suggests that HCC cells with poor nutrition status may rely on ketone bodies to support survival (Table 1 and Figure 2F). Human primary melanoma and hairy cell leukemia cells also show metabolic ketogenesis. Kang et al. [63] found that 3-hydroxy-3-methylglutaryl-CoA lyase (HMGCL) was activated by BRAF V600E-expressing melanoma and leukemia cells, resulting in the activation of the MEK-ERK pathway, the production of acetoacetate (Table 1). Ketolysis and ketogenesis are important for cancer cell activities, and targeting ketone body metabolism can be a novel strategy to develop drug candidates against malignancies.
3.2 Anti-cancer effect
There is abundant evidence showing that fatty acids possess anti-cancer properties. In previous studies, T-cells pretreated with fatty acids were injected into patients to identify changes in functional T-cells [64]. It has been revealed that fatty acids may be used by CD8+ T-cells as energy sources. Thus, anti-tumor effects were observed when cells were simultaneously subjected to hypoxic and hypoglycemic environments [65]. Zhang et al. [66] also found that CD8+ tumor-infiltrating T-lymphocytes (TILs) improved peroxisome proliferator-activated receptor (PPAR)-alpha signaling and degradation of fatty acids under hypoglycemia and hypoxia. Further enhancing fatty acid catabolism sustains the effector function of T-cells, and improves antitumor efficacy.
Fatty acid metabolism is of great therapeutic interest in cancer patient populations. Omega-3 polyunsaturated fatty acids in the diet can partially inhibit CRC development [67]. Zhang et al. [68] discovered that epoxydocosapentaenoic acids (EDPs) derived from omega-3 fatty acids could block angiogenesis as well as endothelial cell migration and VEGF receptor 2-induced protease generation (Table 2). Omega-3 fatty acids may also be involved in certain anti-cancer metabolism pathways and exhibit potential preventive and inhibitory effects in cancer.
4 PROTEIN MODIFICATION
4.1 Dephosphorylation
Serine/threonine-protein phosphatase-mediated dephosphorylation is a key process in physiological conditions, though mutations in phosphatases are found to sustain malignant progression [69, 70]. Mei et al. [71] reported that the replication timing regulatory factor 1 (RIF1) triggered protein phosphatase 1 (PP1) to dephosphorylate axis inhibition protein (AXIN), and stimulated the Wnt/β-catenin axis to support the proliferative invasion of NSCLC cells (Table 1 and Figure 5C). Another phosphatase, protein phosphatase 2A (PP2A), modulates most of the protein dephosphorylation events in the cell by distinct regulatory subunits. Alterations in the subunits disturbed PP2A function and induce oncogenic signaling [72]. Tang et al. [73] found that a PP2A regulatory subunit, STRN3, recruited and dephosphorylated MST1/2, which helps trigger the YAP signaling and suppress the Hippo tumor suppressor of gastric cancer (Table 1). Recently, Liu et al. [74] identified that PP2A inhibitors synergize with chemotherapeutic agents to suppress aberrant signal transduction in cancer. Targeting aberrant protein phosphatase represents a promising therapeutic strategy in cancer treatment.
4.2 Ubiquitination
E3 ubiquitin ligase-induced ubiquitination significantly modulates protein posttranslational modifications in tumor maintenance [75]. Tang et al. [76] found that tripartite motif-containing 11 (TRIM11) sustained tumor-promoting estrogen receptor α (ERα) ubiquitination to further stabilize this receptor in metastatic breast carcinoma (Table 1). Liu et al. [77] demonstrated that in an inflammatory microenvironment, upregulation of Cullin-RING E3 Ligases (CRLs) and activation of c-Myc induced ST7 ubiquitination in colitis-associated cancer (CAC) (Table 1). Blocking the E3 ubiquitin-ligase may be a reasonable anti-tumor strategy in the clinic. Remarkably, Hakin-1, which functions as a specific inhibitor of the E3 ubiquitin-ligase Hakai, was found to inhibit the ubiquitination of E-cadherin and suppress EMT (Table 2), implying a potential strategy to restrict CRC [78]. The ubiquitination of some pivotal molecules by E3 ubiquitin-ligase modulates the activity of oncogenic signaling, and this feature may be potentially explored for designing molecularly targeted drugs for cancer treatment.
5 AMINO ACID METABOLISM
5.1 Glutamine metabolism
High levels of glutamine (Gln) in the blood provide a readily available source of carbon and nitrogen to support cancer cell activities. Wang et al. [79] reported that mitochondrial sirtuin5 (SIRT5) activated glutamate dehydrogenase 1 (GLUD1) and consequently facilitated the incorporation of Gln into the TCA cycle. This indicates the critical role of Gln metabolic rewiring in the malignant phenotypes of CRC (Table 1 and Figure 1C). Similarly, colon cancer-derived mitochondrial glutamic pyruvate transaminase 2 (GPT2)-regulated Gln catabolism is involved in the Warburg effect, which takes advantage of the fact that Gln is the dominant carbon source Gln for the TCA cycle (Figure 3 and Table 1) [80].
The oncogenic transcription factor c-MYC is regulated by the Menin gene, and drives cancer cell proliferation and metabolism in vitro and in vivo [81]. In kidney cancer, prostate cancer, and Burkitt lymphoma, c-MYC also triggers the upregulation of glutaminolysis to fuel tumor growth by increasing P5C synthase and P5C reductase 1-mediated proline biosynthesis from Gln; suggesting a metabolic link between Gln and proline (Table 1 and Figure 3) [82].
Alteration of Gln metabolism contributes to nucleotide biosynthesis and attenuates DNA damage. This leads to an increase in conventional radiotherapy resistance [83]. Targeting Gln metabolic pathways, such as glutaminolysis, may provide a therapeutic strategy to kill tumor cells. The oral glutaminase inhibitor CB-839 was reported to suppress Gln-derived metabolite production during tumor development [84, 85]. Cohen et al. [86] found that cetuximab (which targets EGFR) in combination with CB-839 improved therapeutic efficacy in cetuximab-resistant CRC (Table 2 and Figure 1D). Gregory et al. [87] reported that combining CB-839 with arsenic trioxide or homoharringtonine decreased Gln synthesis in hematologic malignancies, upregulated ROS in the mitochondria, and triggered tumor cell death (Table 2). Dual targeting of oncogenic signaling by combining CB-839 with another anti-tumor agent may be a potential strategy for reversing conventional resistance to therapy.
5.2 Serine metabolism
Compared to normal tissue, cancer cells exhibit altered metabolism with the overexpression of serine synthesis pathway enzymes, such as phosphoglycerate dehydrogenase (PHGDH), which converts 3-phosphoglycerate derived from glucose-6-phosphate into serine [88] (Figure 3). Sullivan et al. [89] found that the overexpression of PHGDH improved serine levels and sustained purine and nucleotide biosynthesis, which supported melanoma and breast cancer growth under serine deprivation (Table 1 and Figure 4D). Activation of serine synthesis resulted in the conversion of glucose to pyruvate via serine dehydratase (SDH), and rewired glycolysis in a pyruvate kinase-independent manner in pancreatic cancer cells [90] (Table 1 and Figure 3). Pacold et al. [91] reported that PHGDH suppression inhibited the production of nucleotides which derived from one-carbon units from glycolytic serine, even in the presence of exogenous serine, demonstrating that serine was a vital source of one-carbon for purine as well as deoxythymidine synthesis in breast cancer (Table 1). Thus, PHGDH might be a novel metabolic vulnerability, and the preclinical evaluation of PHGDH inhibitor could contribute to further therapeutic applications [92].
5.3 Methionine metabolism
For mammalian cells, methionine metabolism is essential for epigenetic reprogramming and cell growth [93]. The methionine cycle flux also impacts the epigenetic state of tumor cells. Metabolomic studies indicated that in NSCLC stem cells, methionine cycle activity is dysregulated, and methionine consumption exceeded methionine regeneration. [94]. Proteomic and genomic analyses showed that methyltransferase nicotinamide N-methyltransferase (NNMT) expression contributed to the cancer-associated fibroblast (CAF) phenotype and caused depletion of S-adenosyl methionine, which is critical for ovarian cancer metastasis [95] (Table 1). Methionine-related interventions are potentially used to treat diseases of metabolic origin. Gao et al. [96] revealed that methionine limitation induced clinical responses in pathological models of chemotherapy-tolerated RAS-driven CRC and soft-tissue sarcoma. Targeting methionine uptake can partly influence cancer metabolism, which ultimately regulates multiple aspects of therapeutic outcomes in cancer.
5.4 Aspartate metabolism
Unlike other amino acids, aspartate is not readily available in the blood, so proliferating cells, such as tumor cells, produce aspartate by themselves. For example, TCA cycle-derived OOA mediates aspartate biosynthesis, which plays a pivotal role in cellular processes [97] (Figure 3). Surprisingly, mitochondrial respiration generates sufficient electron acceptors for sustaining aspartate production [98]. However, aspartate has poor cell permeability, while the amino acid asparagine is available in tumors. Sullivan et al. [99] found that asparaginase 1 (ASNase1) allowed inter-conversion between asparagine and aspartate in 143B cells (human osteosarcoma cells in vitro), and subsequently provided sufficient endogenic aspartate, leading to a significant acceleration of tumor growth (Table 1 and Figure 3). These studies revealed that facilitating metabolic aspartate depletion could help to treat cancer.
5.5 Tryptophan metabolism
Indoleamine 2,3-dioxygenase (IDO) in tumor cells can metabolize tryptophan (Trp) and trigger kynurenine (KYN) biosynthesis, which suppresses T-cell proliferative growth and promotes an immunosuppressive TME [100]. Notably, intratumoral metabolites instigate other tumor-associated cell populations to stimulate Trp catabolism and impair immune function. In multiple myeloma (MM), tumor cells release IL-32 and trigger TAMS to produce IDO. This further antagonizes CD4+ T-cell proliferative growth, which decreases antitumor bioactive substance secretion [101] (Table 1). IDO modulates the immunosuppressive function via depletion of Trp and the accumulation of KYN. Thus, a combination of IDO inhibitors including 1-methyl tryptophan (1-MT) and chemotherapeutic agents containing doxorubicin could be considered as a potential treatment option [102] (Table 2).
5.6 Amino acid metabolism-arginine deprivation
Arginine accelerates tumorigenesis via the enzyme argininosuccinate synthetase 1 (ASS1) which catalyzes the synthesis of argininosuccinate from citrulline and aspartate, and is the rate-limiting enzyme in arginine biosynthesis [103] (Figure 3). This enzyme can be targeted for developing arginine deprivation therapy in multiple tumor types. Huang et al. [104] identified that ASS1-deleted myxofibrosarcoma cells were sensitive to PEGylated arginine deiminase (ADI-PEG20) therapy, and ASS1 deletion was associated with unfavorable clinical results in patients. The feasibility of ADI-PEG20 targeted treatment therapy may be directly linked to the loss of ASS 1 (Table 2).
The availability of ADI-PEG20 is directly implicated in ASS deficiency in other cancer types. Kim et al. [105] pointed out that prostate cancer cells with mitigated ASS were susceptible to autophagy suppression and ADI-PEG20 therapy, while early autophagy was reported to exert an initial protective effect for cancer cells. The above evidence suggests that ASS deletion, autophagy, and ADI-PEG20 efficiency could be interrelated (Table 2). ADI-PEG20 also induced autophagy-dependent death of breast cancer cells with the loss of ASS1, and attenuated de novo arginine synthesis derived from aspartate and citrulline, and arginine deprivation also caused mitochondrial damage and cytotoxic autophagy in cancer cells [106] (Table 2 and Figure 4E). Thus, robust arginine deprivation therapy merits exploration as a potential therapeutic strategy to treat cancer.
6 OTHER METABOLIC PATHWAYS
6.1 Bile acid metabolism
In most cases of sporadic CRC, intestinal bile acids (BAs) are risk factors linked to worse clinical outcomes. Fu et al. [107] showed that APC mutants could change the structure of BA, leading to the production of BAs such as tauro-beta-muricholic acid (T-betaMCA) and deoxycholic acid (DCA). This can lead to an impairment of intestinal farnesoid X receptor (FXR) function, resulting in DNA damage and adenoma-to-adenocarcinoma transformation in CRC (Figure 1E). BA metabolism alters the composition of the intestinal microbiome in the TME of CRC. Yachida et al. [108] observed increased BAs including deoxycholate in polypoid adenomas and/or intramucosal carcinomas, indicating a link between the human gut microbiome, BA metabolism, and the early stage of the development of CRC.
6.2 Vitamin D metabolism
Epidemiological data have shown that vitamin D has anti-cancer function as it was associated with a decrease in CRC risk. Maalmi et al. [109] reported that CRC patients with plasma 25-hydroxyvitamin D (25-(OH)-D3) levels < 30 nmol/L had an extremely high mortality, and 25-(OH)-D3 deprivation led to a poor clinical prognosis. Song et al. [110, 111] analyzed a large number of samples and discovered that elevated blood 25-(OH)-D3 levels were associated with a decreased risk of CRC (Table 2). In addition to CRC, vitamin D boosts CD8+ T-cell function and decreases inflammation of the TME in breast cancer tissue (Table 2) [112]. Due to its anti-inflammatory and anti-tumor properties, vitamin D may be a promising candidate for use as an adjuvant in standard cancer immunotherapies.
6.3 Trace element metabolism
Metabolic imbalances in trace elements are associated with multiple cancer-induced pathological conditions. For example, zinc homeostasis damage causes muscle wasting in cancer patients. Wang et al. [113] discovered that the activated zinc transporter ZRT- and IRT-like protein 14 (ZIP14) in metastatic cancer cells facilitated zinc uptake in muscle progenitor cells and inhibited MyoD and Mef2c, leading to mitigated muscle-cell differentiation. Another trace element, copper, enables cancer cell proliferation, especially in primary pancreatic cancer. Ishida et al. [114] highlighted that the tumor promoter copper interacts with cytochrome c oxidase and mediates oxidative phosphorylation and ATP production (Table 1). Trace elements in the TME may be capable of partially altering tumor metabolic phenotypes.
6.4 Urea cycle metabolism
Arginine is the main source of urea. Arginine is cleaved to produce urea and ornithine. Ornithine supports citrulline biosynthesis in the mitochondria, and subsequently to arginine renewal, and this series of reactions is termed as the urea cycle (UC) [115] (Figure 3). UC dysregulation is a general metabolic feature of multiple cancer types. Lee et al. [116] reported the critical role of the UC disorder in nitrogen conversion toward the activation of carbamoyl-phosphate synthetase 2, aspartate transcarbamylase and dihydrooratase (CAD). This contributes to subsequent pyrimidine synthesis and a detectable hallmark constituted by transversion mutations at the nucleotides, nucleic acid and protein levels in prostate cancer, breast cancer, and lung carcinoma models (Figure 4F, Figure 3, and Table 1). The UC is a metabolic vulnerability in EGFR-driven NSCLC, and sustains cellular energetics upon inhibiting EGFR [117].
6.5 Stress-mediated adrenaline metabolism
Stress mediates neurochemical and endocrinological alterations, and leads to increased levels of adrenaline in metastatic tumor initiation [118]. Chronic behavioral stress induces the sympathetic nervous system (SNS) and contributes to greater tumor burden and invasive growth in HCC and breast cancer. Huan et al. [119] identified that SNS supported HCC behaviors by targeting alpha1-adrenergic receptors (ARs) in Kupffer cells to modulate chronic liver inflammation, secretory interleukin-6 (IL-6) production, and transforming growth factor-beta (TGF-β) production (Figure 2G). Cui et al. [120] demonstrated that stress-activated SNS stimulated the production of epinephrine which triggered LDHA to generate lactate and stabilize Myc, subsequently triggered SLUG and further sustained breast cancer stem-like properties (Figure 4G). Activated SLUG inactivates E-cadherin and accelerates breast cancer cell metastasis (Figure 4G) [121, 122]. Significantly, Daher et al. [123] identified that β-blockers enhanced CD8+ T-cell responses and propranolol could synergize with anti-cancer vaccines in cancer immunotherapies (Table 2). Thus, chronic stress-induced adrenaline signaling regulates metabolic rewiring in cancer progression, and this complements existing therapeutic strategies with beta-blockade.
6.6 HMOX1-dependent pathway
In cancer development, the superinduction of oxidative stress response often causes depletion of tumor suppressors, with the concomitant accumulation of heme oxygenase 1 (HMOX1) and Bach1, a sensor and effector of heme [124]. HMOX1 contributes to create a microenvironment that promotes tumor initiation. In addition, HMOX1 and Nrf2 significantly correlate with specific organ colonization of malignancies [125]. Lignitto et al. [126] discovered that Nrf2 was presented in nearly 30% of lung cancer cases, and enabled metastasis by stimulating HMOX-1 activity which subsequently downregulated heme and suppressed Fbxo22 (a ubiquitin ligase)-induced degradation of Bach1 in NSCLC (Table 1 and Figure 5D). Potent HMOX-1 inhibitors may be effective in alleviating malignancies.
6.7 Autophagy pathway
Autophagy predominates in cellular catabolic responses under nutrient or energy depletion [127], while tumor cell metabolism strikingly affects autophagic processes of the cell. Thomas et al. [128] found that genetic defects in mitochondrial complex I suppressed autophagy induced by mTOR inhibitors in cells with increased mitochondrial metabolism. However, the lack of the autophagy gene Atg5 in KRAS-driven cancer led to impaired asparagine metabolism, reduced mitochondrial function, and caused excessive mitochondrial fragmentation. This evidence supports the critical role of autophagy in KRAS-driven progression [129]. In addition, upon serum starvation or metabolic stress, the oncoprotein lysosomal protein transmembrane 4 beta (LAPTM4B) and the exocyst subcomplex Sec5 stimulated inactive EGFR to interact with the autophagy inhibitor Rubicon, resulting in a disassociation of the Beclin 1-Rubicon complex. Subsequently, initial autophagic activity was triggered, which correlated with tumorigenesis [130]. Autophagy may be positioned to tune tumor metabolism under poor nutritional conditions within the TME.
7 METABOLOMIC PROFILING
Metabolic profiling helps in understanding the molecular mechanisms involved in individual tumors in cancers such as HCC. Tan et al. [131] provided serum profiling data and identified the diagnostic usefulness of taurocholic acid, lysophosphoethanolamine, and lysophosphatidylcholine, which indicate the aberrant metabolic properties in all HCCs. Metabolomics can help in the identification of underlying inflammatory metabolite markers for early HCC diagnosis. Aleksandrova et al. [132] conducted metabolic profiling in HCC, intrahepatic bile duct (IBD), gallbladder, and biliary tract cancers (GBTC), and identified the diagnostic role of C-reactive protein (CRP), IL-6, non-high-molecular-weight (HMW) adiponectin, and C-peptide, suggesting that inflammation and hyperinsulinemia are involved in hepatocarcinogenesis (Table 3).
| Metabolic biomarker | Cancer type | Reference |
|---|---|---|
| Taurocholic acid, lysophosphoethanolamine and lysophosphatidylcholine | Hepatocarcinoma | Tan et al., 2013 [131] |
| CRP, IL-6, non HMW adiponectin, and C-peptide | Aleksandrova et al., 2014 [132] | |
| AEA and PEA | Hepatocarcinoma infected with HCV | Zhou et al., 2012[133] |
| Ethanolamine, lactic acid, phenylalanine, and ribose | Hepatocarcinoma after surgical resection. | Ye et al., 2012 [134] |
| Chain lengths ceramides and sphingomyelins | Epithelial ovarian cancer | Kozar et al., 2018 [135] |
| N-oleoyl taurine | Prostate cancer | Huang et al., 2019 [136] |
| Acetate | Colorectal cancer | Lin et al., 2019 [137] |
| 2-hydroxyisobutyrate, 3-indoxylsulfate, and alanine | Gastric cancer | Chan et al., 2016 [138] |
- Abbreviations: AEA, endocannabinoids anandamide; CRP, C-reactive protein; HCV, hepatitis C virus.; HMW, high-molecular-weight; IL-6, interleukin-6; NSE, neuron-specific enolase; PEA, palmitylethanolamide.
Zhou et al. [133] performed serum metabolic profiling and reported that higher concentrations of arachidonic acid and lower levels of lysophosphatidylcholines (lysoPCs) with polyunsaturated fatty acid acyl chains, led to HCC development in conditions of chronic inflammation, and elevated serum endocannabinoids anandamide (AEA), and palmitoylethanolamide (PEA) could lead to HCC in hepatitis C virus (HCV)-positive patients (Table 3).
In addition, metabolomics method sheds light on the metabolic regulation of HCC after surgical resection. Ye et al. [134] proposed that post-surgical HCC patients displayed complex metabolic responses that promoted anabolic metabolism; they further identified 16 elevated metabolites in HCC recurrence as well as five feasible diagnostic markers including ethanolamine, lactic acid, phenylalanine, and ribose (Table 3).
Metabolomic profiling is diverse and flexible, and provides opportunities to also identify metabolic markers in other cancer types. Kozar et al. [135] utilized serum metabolomic profiling and identified ceramides and sphingomyelin compounds of specific chain lengths as diagnostic markers in epithelial ovarian cancer (Table 3). In addition, serum metabolomics indicated that N-oleoyl taurine correlated with impaired metabolism and contributed to prostate cancer pre-diagnosis [136] (Table 3). Additionally, metabolomics based on HNMR revealed that 2-hydroxyisobutyrate, 3-indoxylsulfate, and alanine from urine in gastric cancer and acetate from fecal metabolites in patients with CRC exhibited higher diagnostic superiority than other metabolites in corresponding specimens (Table 3) [137, 138]. Metabolic signatures reflect the tumor tissue microenvironment, and metabolomics can enable the identification of sensitive diagnostic biomarkers for malignancies in a clinical setting.
8 CONCLUSIONS AND OUTLOOK
In this review, we summarized a variety of sufficiently unrecognized metabolic signaling pathways in tumorigenesis, invasive metastasis, aggressive growth, and immunosuppressive reactions. Research on cancer metabolism has made great progress, and the genetic background and metabolic signatures of tumors, including the idiographic concepts mentioned above, are worth further exploration.
Cellular metabolism is a key link between the extracellular environment and intracellular processes, and cancer-specific metabolic rewiring frequently converts normal physiological metabolic processes, such as protein modification and diverse enzymatic reactions, into necessary protective barriers for proliferating tumors [139-141]. Tumor cell populations compete with the normal tissue for glucose, and rate-limiting stimulators subsequently coordinate the Warburg effect. In addition, increased anaerobic glycolysis provides sufficient building blocks of bioactive substances including purines and pyrimidines in combination with other equally crucial metabolites. In condition of glucose starvation, other metabolites are metabolized which not only provides energy supplies but also stimulates oncogenic alterations.
Therefore, identifying and further targeting the metabolic nodes of tumor cells is the promising therapeutic interventions in patients with malignancies. Compared with most conventional diagnostic methods, metabolomics effectively analyzes accessible biofluid which contain abundant metabolic information therein in cancers. Some malignancies are lack of early diagnostic platform, and metabolomics contributes to search for circulating metabolic biomarkers and achieve clinical therapies such as early surgical resection of the cancer [142, 143]. New discoveries into cancer metabolic reprogramming provide metabolic vulnerabilities which promote cancer treatments. Increasing small molecule metabolic inhibitors loaded by nanomaterials are employed as adjuvants with conventional anti-tumor agents, which can improve biosafety of metabolic inhibitors. Furthermore, nanoplatform induces apoptosis of cancer cells by enhancing ROS production that suppresses tumor growth [144]. Nanoscale functional materials not only achieve anti-tumor functions of carried drugs but also improve cancer treatments.
In brief, tumor cells exhibit high metabolic activity and energy consumption, which causes exhaustion in cancer patients. Thus, it may be necessary to design therapeutic strategies to reduce the metabolic rate of tumor cells to decrease cancerous phenotypes caused by oncogenic mutations.
DECLARATIONS
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
COMPETING INTERESTS
The authors declare that they have no competing interests.
FUNDING
This work was supported partly by the National Natural Science Foundation of China (81541153 and 81772404), The Guangdong Science and Technology Department (2016A050503046, 2015A050502048, 2016B030309002 and 2019B090905011), The Fund of Southern Marine Science and Engineering Guangdong Laboratory (Zhanjiang) (ZJW-2019-007), and The Public Service Platform of South China Sea for R&D Marine Biomedicine Resources (GDMUK201808).
AUTHORS' CONTRIBUTIONS
Z.T. wrote the manuscript. Z.X. and J.Z. discussed and edited the manuscript. X.Z. and J.Z. designed the concept, edited the manuscript. X.Z. and J.Z. supervised the project. All authors agree on the final version.
ACKNOWLEDGEMENTS
Not applicable.