The anatomy of the male inferior hypogastric plexus: What should we know for nerve sparing surgery
Abstract
The aim of this study was to investigate the nerve supply to the structures in the male lesser pelvis and review its clinical relevance, especially during nerve sparing surgery. Three formalin-embalmed and 16 Thiel-embalmed male hemipelves were used. They were microdissected after repeated treatments with nitric acid diluted 1:10 with milliQ-water. The inferior hypogastric plexus (IHP) is a fan-like structure lateral from the rectum on the fascia of the levator ani. Nerves emerging from the proximal, solid part of the plexus follow the internal iliacal vessels and reach the prostate from dorsolateral. The innervation of the urethra and the corpora cavernosa derives from two origins: one follows the ejaculatory duct and the seminal vesicle, reaching the proximal urethra and the prostate from dorsal; the other follows the inferior vesical artery to reach the prostate from lateral, and then forms the neurovascular bundle on both sides of the prostatic fascia, spreading to the pelvic floor muscles and the corpora cavernosa along with the distal urethra. A connection between the two parts was demonstrated in approximately one third of the samples investigated. The nerve supply to the urinary bladder, the urethra, and the corpora cavernosa emerges mainly from the IHP. The innervation of the proximal urethra and its autonomic muscular structures has a dorsal (ejaculatory duct) and lateral (inferior vesical artery) origin. To maintain good erectile and continence function it is important to save both the dorsal and lateral neurovascular roots. Clin. Anat. 31:788–796, 2018. © 2018 Wiley Periodicals, Inc.
INTRODUCTION
It is common knowledge that the viscera inside the pelvis are innervated from the inferior hypogastric plexus (IHP), which contains nerves from the sacral plexus and the superior hypogastric plexus. The superior hypogastric plexus is a network of sympathetic nerves taking its origin in the thoracic and lumbar segments of the spinal cord. Out of this preaortic plexus rises the hypogastric nerve (HN), carrying sympathetic fibers toward the lesser pelvis, where they join the parasympathetic splanchnic nerves (SN) coming from the sacral plexus and building a fan-like meshwork. The latter is called the IHP or pelvic plexus. It provides nerves for all organs in the lesser pelvis, in particular the rectum, the urinary bladder (UB), the seminal vesicles (SV), the prostate, the urethra, and the penis in males (Schiebler and Arnold, 1977; Mauroy et al., 2003).
There is a large body of evidence that the autonomic nerves are responsible for erectile function and partly for continence (Costello et al., 2004; de Groat et al., 2015; Fowler et al., 2008; Sadananda et al., 2011). The sympathetic nerves have their origin within spinal cord segments T12-L2 and the parasympathetic nerves come from S2–4. The SN and their parasympathetic fibers course toward the pelvic organs enabling the detrusor, the UB sphincter muscles, and the anal sphincter (Jung et al., 2012; Moore et al., 2006). Although this autonomic plexus and its origin are well known, the exact route of the fibers through the lesser pelvis to reach their target organs remains unclear. There is also some uncertainty about exactly how the organs, especially the so-called continence organ, are innervated.
To effect the “continence organ,” different structures are involved. Mainly this term stands for the pelvic floor muscle and the sphincter muscle around the urethra and rectum (Yucel and Baskin, 2004; Slaby et al., 1994). The pelvic floor muscles are represented by the levator ani, and in the older literature, the urogenital diaphragm is also represented by the transverus perinei muscle, which was believed to form the external sphincter of the urethra. Strasser et al. (1996) showed that the urogenital diaphragm is not a horizontal muscle under the levator ani, not is the sphincter muscle along the male urethra a circular structure within the urogenital diaphragm. It is a much more longitudinal muscle starting from the base of the UB and extending up to the bulb of the penis. This structure is commonly called the rhabdosphincter and seems to be omega-shaped and to surround the urethra. It covers the urethra from ventral and lateral but not from dorsal. Different authors describe it as either a muscular structure comprising two different tissue types, an inner smooth muscle cell area and a striated muscle fiber part; or according to a recent concept of two different muscles it comprises the inner sphincter, the so-called lissosphincter, composed of smooth muscle fibers, and an outer coat-like sphincter, the rhabdosphincter, composed of striated muscular tissue (Sievert et al., 2008).
As there are two different muscle types, it was hypothesized that two different neurological structures are responsible for the innervation: a somatic part via the pudendal nerve on one side, and an autonomic part via nerves coming from the IHP on the other (Karam et al., 2005a; Karam et al., 2005b). Hollabaugh et al. (1997) demonstrated a branch from the pudendal nerve innervating the striated muscle around the urethra. This so-called continence nerve reaches the muscle after the pudendal nerve is already in the ischio-anal fossa inside the pudendal canal.
The innervation via the IHP seems to pass through the lesser pelvis following the internal iliac vessels.
The aim of this study was to determine the exact anatomical branching of the IHP and improve knowledge about the autonomic innervation of the male urogenital organs.
MATERIALS AND METHODS
Collecting Process
- The institute of Anatomy was not notified within 24 hr after the body donor's death;
- Infectious diseases (e.g., tuberculosis, HIV);
- Morbid obesity;
- Open or unhealed wounds (e.g., after surgery);
- Amputation of body parts or organs (e.g., after different research performed on the material);
- Surgical removal of organs for organ donation programs prior to death;
- Female gender of the donor
There was no upper age limit.
Dissection
To obtain a brief overview of the anatomy of the IHP and its location in the male pelvis, three formalin-fixed hemipelves were grossly dissected. The formalin-embalmed material was not studied further as it was only used for orientation, so the Thiel-embalmed material could be dissected exactly.
For microdissection, Thiel-fixed specimens were used according to the following protocol: Prior to microdissection, the vessels were injected with polyurethane (PU4ii, VasQec®, Switzerland), blue colored PU4ii into veins and red PU4ii into arteries (Haenssgen et al., 2014). Pressure was applied during the injection, so the capillary system was also filled. A macroscopic gross dissection was then performed, removing most of the connective tissue and fat, to gain access to the tissue of interest. To obtain better insight into the pelvis, the pelves were cut in half or one ilium was removed. The IHP was more clearly imaged in the halved pelvis because the organs could be pulled apart and away from the nervous structures. With only the ilium removed, the organs remained intact, and making it possible to reveal the exact routes of the nerves and the relationship between the left and right IHP and all the nerves prior to reaching their target organs.
In order that very small nerves could also be identified, the tissue was macerated according to Bangerter et al. (2017). Briefly: the pelves were embedded in nitric acid diluted 1:10 in miliQ water for 6–8 hr, then rinsed under tap water for 15–30 min and embedded in tap water for one hour. The acid solution removed fat tissue and colored the nerves more whitish. The tap water caused swelling of the small nerves, which made their preparation easier. This procedure was performed at any time during the dissection process, whenever it was no longer possible to distinguish small nerves from connective tissue.
In addition to maceration, to obtain an even more specific view in the end, microdissection was performed using a surgical microscope (OPMI® Pico, Carl Zeiss Surgical GmbH, Germany).
Imaging
During the dissection, images were taken with a Canon EOS 5 D and processed with Adobe Photoshop CC 2015.1.2.
For histology samples, tissue was taken from the UB, the prostate, and the SV in the same pelvis. The material was embedded in 4% paraformaldehyde and fixed in paraffin. Afterwards, it was cut in 5 µm slices and stained using Hematoxylin-eosin. The histology samples were examined with a Zeiss Axio Imager M2 microscope.
RESULTS
Overview of Nerve Supply in the Male Pelvis
Formalin embalming resulted in robust tissue preservation but the connective tissue surrounding the nerves and blood vessels had a stiff and firm consistency. This made precise microdissection of tiny delicate nerves nearly impossible, and often they could not be distinguished from connective tissue strands. Therefore, formalin-embalmed samples were used to obtain an overview of the gross anatomy of the autonomic nerves in the lesser pelvis (Fig. 1A), and this was used as a guide to gain knowledge of the anatomy of the IHP and its location and connections.
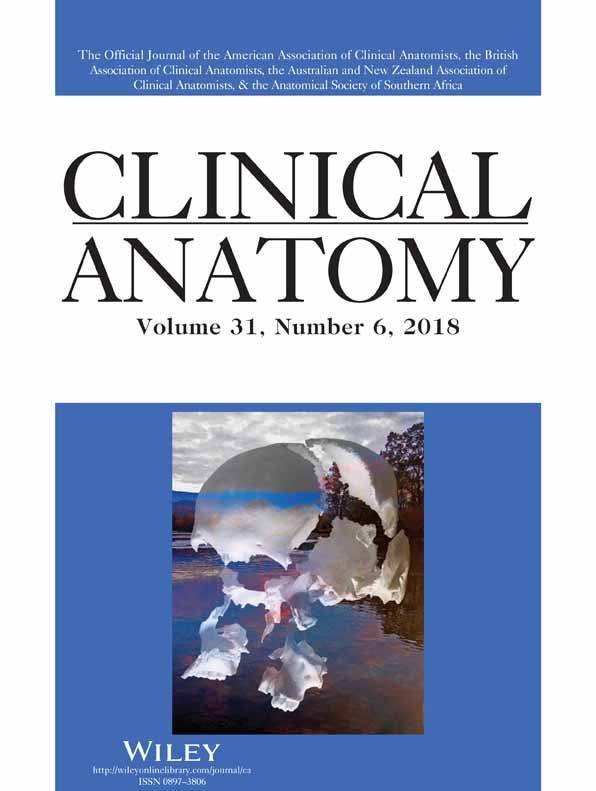
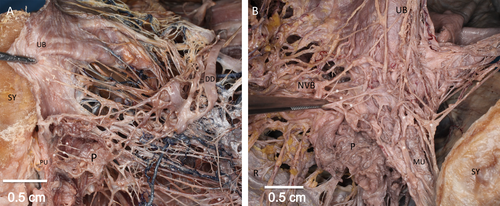
Overview of a formalin-embalmed (A) and thiel-embalmed (B) male hemi pelvis. A, Medial view of a grossly dissected hemipelvis. The promontory (PM) and pubic SY form the left and right borders, respectively, around the pelvic organs. The rectum (R) is pulled towards caudal and medial to reveal the IHP. On the tip of the IHP, the HN is visible, marking the connection with the superior hypogastric plexus. Coming from dorsal, the pelvic SN join the IHP. The UB, prostate (P), and urethra (orange line) receive multiple NB from the IHP. B, Thiel-embalming allows the same structures to be revealed in greater detail. The blue tweezers mark the lumbar spine; the pubic SY and the PM mark the ventral and dorsal borders of the lesser pelvis respectively. Again, the rectum (R) is pulled towards caudal and medial (lower border of the image) to reveal the nerves. In the middle of the image, the solid part of the IHP is visible. Also visible are the UB, the prostate (P), the ductus deferens (DD), and NB out of the IHP towards the viscera. The NB are surrounded by the square labeled at the edge with NB. Also in the square, in a second plane, the dark blue colored branches of the pelvic vessels are visible behind the nerves.
Gross dissection of formalin-embalmed material showed the nervous structure forming a main part of the IHP medial from the levator ani between the rectum and the UB. In the cranial region, there was always a connection to the superior hypogastric plexus via the HN. Starting from this point, the IHP spread in a triangular, fan-like form. Towards the dorsal part, the IHP connected to the roots of the sacral plexus via the SN carrying the parasympathetic fibers. The branches from the IHP toward the rectum were visible toward the dorsomedial region, and the nerves for the UB, the SV, the prostate and the urethra were present toward the anterior. After this gross overview of the structures in the male lesser pelvis had been obtained, even the smallest branches entering the organ wall could be dissected precisely in the Thiel-embalmed material (Fig. 1B).
Nerves to the UB
Following the HN, the solid part of the IHP could be displayed in all hemipelves. It was always found on top of the fascia of the levator ani, medial of the internal iliac vessels. This part seemed to be built from solid nerve fibers forming a dense network. Its consistency was variable, ranging from a solid plate to a more or less divisible nervous structure. Numerous nerve branches (NB) arose from this solid part and followed the umbilical artery toward the top of the UB. This was similar in all dissected pelves.
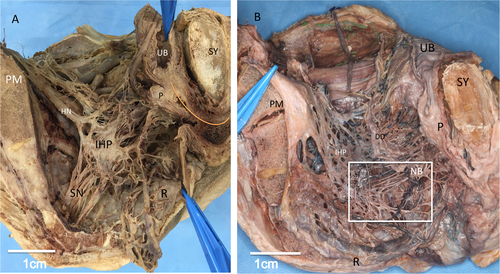
The nerves going ventrally were followed and the supply to the UB was investigated. Two main portions could be distinguished: nerves coming directly out of the IHP running to the dorsal, that is, to the apex of the UB (Figs. 2A and 2A′), following the umbilical artery and nerves coming out of the IHP to form a subplexus (SP) around the SV. This SP provided nerves for the basal part of the UB (the so-called trigone of the bladder), the SV, and the prostate (Fig. 2B).
Close-up of the UBs autonomic nerve supply in Thiel-embalmed material. A, Overview of the male hemi-pelvis: The UB is pulled towards anterior in the direction of the pubic SY. The PM marks the posterior border. In the middle of the image, the DD and its connection to the SV and the prostate (P) are visible. From posterior, the IHP sends its autonomic nerves towards the UB. The autonomic nerves coming directly out of the IHP to reach the back and the top of the UB are marked with white arrows. A′, Zoom-in on the cranio-dorsal aspect of the UB: The forceps pulls the bladder towards ventral. The top and back of the UB are displayed to reveal the autonomic nerves in this area. Again, the nerve supply is marked with white arrows. B, Zoom-in on the base of the UB and the plexus around the SV: The UB is pulled lateroventral in the direction of the pubic SY. The forceps in the left lower corner holds the DD with the SV and the surrounding SP. Between the UB and the SV, the nerves and vessels to the base of the UB and the prostate (P) are indicated with white arrows.
Up to 40 different nerves came directly out of the solid part of the plexus in all pelves. They were found directly under the peritoneum. By gently pulling the visceral peritoneum off the top of the UB, their entire pathways through the lesser pelvis were revealed. On their way to the UB, they made connections to the nerves around the vas deferens and ended on the top of the UB. They seemed to innervate the detrusor.
Apparently, the nerve supplies to the base of the UB, the prostate, and the prostatic part of the urethra originate from the same SP. In all individuals, there was a more or less dominant SP around the SV. It was located on the outer superior part of this glandular structure. Following the ejaculatory duct, the nerves entered the prostate and reached the bottom of the UB (Fig. 2B), where the lissosphincter lies.
Nerves to the Prostate and the Rhabdosphincter
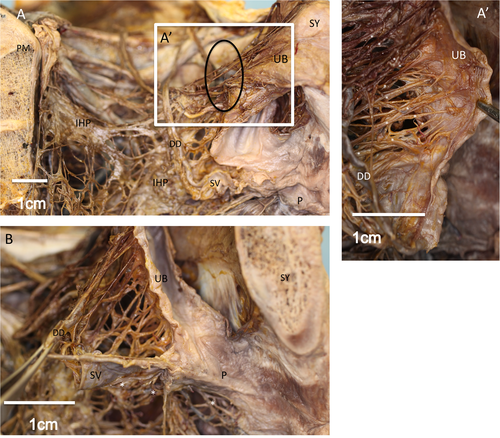
To locate the nerves around the prostate more exactly, a separate and more detailed microdissection was performed in this area. This showed nerves following the SV and the ejaculatory duct into the prostate and toward the prostatic urethra (PU; Fig. 3A). These nerves showed connections to the trigone of the bladder, where the internal urethral orifice (OU) lies. They seemed to reach the urethra directly between the bottom of the UB and the base of the prostate (Fig. 3A). To explore this area, the prostate was gently stripped away from the base of the bladder. This allowed for a preparation of the nerves following the SV. The nerves lying on the lateral wall of the SV turned more medially and were then found cranial of the SV to enter between the base of the prostate and the UB, ending in the area of the lissosphincter. Some nerve fibers also followed the SV and the vas deferens into the prostate. To reveal these structures, the prostate was also dissected. In the prostatic tissue, we observed small nerves ending at the PU.
Insight into the autonomic innervation of the different organs in the lesser pelvis. A, Autonomic innervation of the base of prostate (BP), SV, and proximal urethra: The pubic SY is located in the upper part of the image. The UB is cut in half to reveal the internal OU, the SP around the SV, and the BP. The prostate is dissected to reveal nerves towards the proximal urethra. The autonomic nerves appear as yellow structures as all the fat is removed. Nerves are indicated by white arrows. These structures represent the nervous tissue towards the PU and the base of the UB. B, Anterior-lateral portion of the autonomic prostate innervation: The nerves (indicated by arrows) ending on the side and in front of the organ are identified as part of the NVB. The UB is pulled towards medial and the pubic SY is located on the left border.
There were also nerves from the lower part of the IHP that did not enter the plexus around the SV but ran downwards between the rectum and the prostate and then went laterally, around the prostate, ending on the side and in front of the organ. These nerves were identified as part of the so-called neurovascular bundle (NVB; Fig. 3B).
In five of the 16 hiel-embalmed (31.25%) hemipelves there were nerve fibers running along the SV, turning more laterally. They did not enter the prostate but ran down toward its lateral side to join the nerves coming out of the IHP, not forming a SP around the SV.
The most lateral lying structure from the prostate was a venous plexus, followed more medially by the arteries and nerves. We identified the main artery in this area as the inferior vesical artery. On their way, several nerves left the NVB and ended at different levels of the prostate, penetrating the gland to reach the PU. The final nerves ended in front of the prostate, where the rhabdosphincter lies, and in the corpora cavernosa.
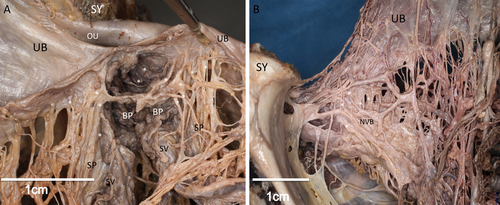
To provide a good view of the structures close to the prostate and the surrounding muscles, the soft tissue was disconnected from the pubic symphysis (SY). This revealed a meshwork of NB coming from posterior (from the lower part of the IHP) and traveling lateral from the prostate on the fascia of the levator ani. Some of these nerves could be seen to penetrate the prostate and end at the prostatic part of the urethra (Fig. 4A). A second set of nerves traveled to the corpora cavernosa and formed a more ventral-lying network (Fig. 4B).
Microdissection of the nerves around the prostate. A, Microdissection of the nerves to the PU: The nerves responsible for innervating the PU originate from the dorsal, that is, lower part of the IHP. The pubic SY is located on the left side and the DD on the right. The UB is pulled towards anterior. The prostate (P) is dissected to make the small nerves (arrows) to the PU visible. The route of the PU is marked with the orange line. B, Microdissection of the lateral nervous supply, ending in the anterior part of the prostate: Medial view of the UB, the prostate, the rectum and the NVB. In the lower right corner, the pubic SY is visible. The UB is pulled towards cranial and lateral. The prostate (P) is dissected. Beneath the prostate, the MU is visible. On top of these structures lies a meshwork of nerves (arrows) coming from posterior [where the rectum (R) lies]. The tweezers are holding the NVB. It can clearly be seen how small NB (arrows) leave the NVB and reach the urethra through the prostate and also how they follow the MU towards the corpora cavernosa.
We believe these nerves are part of the NVB. They were also found to innervate the rhabdosphincter or continue with the urethra through the pelvic floor, ending at the corpora cavernosa.
The routes of the different nerves are summarized in the scheme in Figure 5. The IHP is marked as the red triangular structure on the rectum.
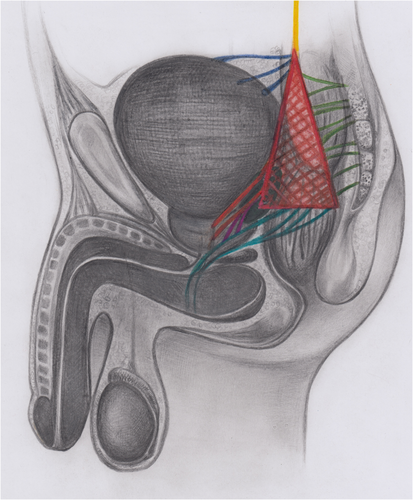
Scheme of innervation of the UB, the urethra and the corpora cavernosa. The IHP is marked as the red triangular structure on top of the rectum. From cranial, the hypogastric nerve runs down into the lesser pelvis (in yellow). From dorsal, the SN provide the parasympathetic nerve fibers (in green). Towards anterior, the nerve supply to the top of the UB is marked in dark blue. The nerves forming the SP around the SV are displayed in orange and the NVB lateral of the prostate in light blue. The connection between the SP around the SV and the NVB is illustrated in purple.
Histological Assessment
To demonstrate the nervous tissue in the dissected area we took histological samples of the UB, where the nerves were clearly visible. This material was processed for microscopic examination. The stained material clearly revealed nerves beside the muscular structures of the UB (Fig. 6).
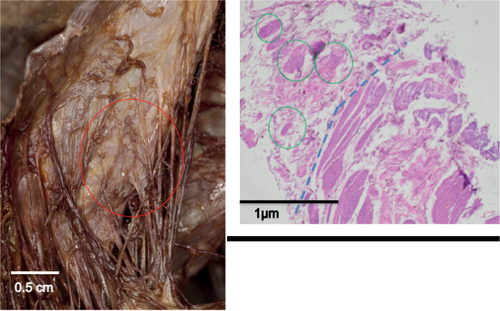
Correlative microscopy. A, Nerve supply to the cranio-dorsal part of the UB: In the upper left corner the pubic SY would be located. The nerves coming out of the IHP directly innervating the back of the UB are visible. The circle marks the area from which histological samples were collected. B, Hematoxylin-Eosin stain: Histological picture of the structures marked by the circle in A. The muscular tissue of the top of the UB is visible on the right side of the image. The nervous structures are marked by circles. B′: Zoom in on the nervous tissue: Histologically, the dissected structures were proven to be peripheral nerves. [Color figure can be viewed at wileyonlinelibrary.com]
DISCUSSION
The male sphincter complex was described by Koraitim (2008) as comprising an internal and an external muscular structure. The internal muscle lies directly under the urothelium of the proximal urethra and extends up to the membranous urethra (MU). It is composed of circular and longitudinal smooth muscle fibers. This structure is also called the lissosphincter. It is predominant in the upper part of the urethra underneath the internal OU in the deep trigone. More ventral to this structure is a striated muscle fiber plate. This so-called rhabdosphincter is the external part of the male sphincter complex. Several studies have shown the rhabdosphincter not to be a horizontal muscular plate but a more vertical, coat-like structure in front of the prostate. It surrounds the prostate and the urethra from ventral in an omega-shape from the base of the prostate to the MU.
This dual muscular system strongly suggests that the nerve supply must also be dual. Narayan et al. (1995) demonstrated a somatic component provided by the pudendal nerve, reaching the striated muscular formation from ventrally, after the pudendal nerve has entered the pudendal canal. These nerves travel far from the prostate under the levator ani.
The autonomic nerves must be provided by the IHP (pelvic plexus), which is located medial from the fascia on the levator ani and lateral of the rectum. With its anterior border, it reaches the SV and the UB (Burnett and Mostwin, 1998; Secin and Bianco, 2010). We confirmed this location and orientation as consistent in all dissected male pelves. This solid part was found right and left of the rectum, medial to the internal iliac vessels. Lunacek et al. (2005) described the lowest part of the IHP as giving origin to the cavernosal nerve, which travels between the prostate and the rectum in a caudal direction to then goes laterally around the prostate to reach the corpora cavernosa of the penis and also provides nerves to the rhabdosphincter. It has been shown that by sparing these nerves, continence, and erectile function are much better retained (Walz et al., 2007). We found the IHP to give origin to numerous nervous structures running down the pelvis in relation to the inferior vesical artery toward the prostate and the rhabdosphincter. We did not find these nerves to be part of one solid structure, as the term “cavernosal nerve” implies. The numerous nerves travel between the rectum and the prostate, to turn more laterally and there form the NVB (Fig. 4B), where they are accompanied by vessels ending at the rhabdosphincter and the corpora cavernosa. Concerning the nerve supply to the UB and urethra, we found two clearly different structures in our study: on one side the nerves coming from the inferior part of the IHP running toward the apex of the prostate and the rhabdosphincter; and a more superior part forming a SP around the SV and innervating the more proximal prostate and the PU with the lissosphincter. These nerves were very variable in thickness, number, and location. In some specimens, they could be clearly discriminated from one another. In other pelves (five out of 16; 31.25%), several connections between the SP around the SV and the NVB could be identified.
In the literature, the effect of nerve sparing surgery is controversial. Burkhard et al. (2006) showed a strong association between postoperative continence and nerve sparing surgery, and a meta-analysis by Nguyen et al. (2017) led to the same conclusion. These clinical results are supported by our anatomical findings. The nerves leaving the lower part of the IHP and traveling around the prostate either ended by reaching the rhabdosphincter or followed the urethra to reach the corpora cavernosa outside the pelvic structures. By saving these nerves during radical prostatectomy, erectile function and continence of the UB should be improved.
Second, our findings suggest an important role for the nerves surrounding the SV in maintaining continence and erectile function after surgical interventions, as the SP around the SV seems to be responsible for innervating the PU and not the cavernosal nerve (Figs. 3A and 4A). We think these nerves innervate the most proximal part of the lissosphincter and provide continence at rest. In addition, in approximately one third of the dissected hemipelves, we found nerves connecting the NVB and the SP around the SV. These nerves showed no connection to the PU but joined the NVB on its way toward the rhabdosphincter and the corpora cavernosa. This suggests that the SV, predominant on the lateral side, are guiding structures for important nerves worth preserving during surgery for good functional results. The landmark of the inferior vesical artery could save most of the NVB coming from the lower part of the IHP (as we found in our study), but the clinical relevance of saving the SV has to be investigated in further clinical trials.
CONFLICT OF INTEREST
No author has to declare any conflict of interest.