Epidemiology of twinning in the National Birth Defects Prevention Study, 1997 to 2007
Presented as posters at the 15th Annual Meeting of the National Birth Defects Prevention Network., February 27–29, 2012, Arlington, VA; and the 17th Annual Maternal and Child Health Epidemiology Conference, December 14–16, 2011, New Orleans, LA.
This research was supported in part by appointments to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC. This work was supported through cooperative agreements under PA 96043, PA 02081, and FOA DD09-001 from the Centers for Disease Control and Prevention to the Centers for Birth Defects Research and Prevention participating in the National Birth Defects Prevention Study.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Abstract
Background
Our objective was to evaluate associations between twinning and maternal demographic factors and periconceptional exposures among infants with and without orofacial clefts.
Methods
We used data from the National Birth Defects Prevention Study; 228 twins and 8242 singletons without birth defects (controls), and 117 twins and 2859 singletons with orofacial clefts, born 1997 to 2007, were included in the analyses. Because of the occurrence of twinning due to the use of assisted reproductive technologies, logistic regression models were computed to estimate odds ratios and 95% confidence intervals for each exposure, stratified by fertility treatment use. To evaluate factors by zygosity, we used sex-pairing data and a simulation approach to estimate the zygosity of like-sex twin pairs for unassisted conceptions.
Results
Among control mothers who did not use fertility treatments, predictors of twinning included non-Hispanic black maternal race (adjusted odds ratio, 1.6; 95% confidence interval, 1.0–2.4), and tobacco smoking (adjusted odds ratio, 1.6; 95% confidence interval, 1.1–2.4). Among control mothers who used fertility treatments, older maternal age, higher income, and state of residence were associated with twinning. Associations were generally stronger among mothers of dizygotic (estimated) twins than monozygotic (estimated) twins. Results for mothers of infants with isolated orofacial clefts were similar to those of controls.
Conclusion
We observed an increased twinning frequency with increasing maternal age, but factors such as maternal race/ethnicity and socioeconomic status may also contribute. Among women receiving fertility treatments, factors associated with twinning suggested a relation with treatment specifics (e.g., treatment type and number of embryos implanted) and availability of insurance coverage. Birth Defects Research (Part A) 103:85–99, 2015 © 2014 Wiley Periodicals, Inc.
Introduction
In 2011, 1 in every 30 babies born in the United States was a twin (Martin et al., 2013). Twinning is associated with numerous pregnancy complications and adverse maternal and fetal outcomes (Helmerhorst et al., 2004; Boulet et al., 2008; Morcel et al., 2010; Yang et al., 2011). Mothers of multiples have twice the risk of pregnancy-related mortality and an increased risk of preterm labor and cesarean delivery (Conde-Agudelo et al., 2000). Compared with singletons, twins are at a higher risk of low birth weight, birth defects, prematurity, and infant mortality (Martin and Park, 1999; Li et al., 2003a; Tang et al., 2006; Chauhan et al., 2010; Zhang et al., 2011). The increased risk for adverse outcomes is particularly concerning given the increasing rate of twin births in the United States from 1980 (18.9 per 1000) to 2011 (33.2 per 1000) (Martin et al., 2013).
Recent studies have estimated that approximately 19% of U.S. twin births are attributable to assisted reproductive technology (ART) and an additional 19% of twin births are attributable to non-ART ovulation stimulation treatments (Sunderam et al., 2012; Kulkarni et al., 2013). Other factors that are associated with twinning include a family history of twinning, older maternal age, multiparity, obesity, and African-American race (Khoury and Erickson, 1983; Allen and Parisi, 1990; Martin and Park, 1999; Hoekstra et al., 2010). The relationships between twinning and oral contraceptives, folic acid-containing multivitamins, and maternal smoking have been examined, with conflicting results (Rothman, 1977; Olsen et al., 1988; Czeizel et al., 1994; Li et al., 2003b; Muggli and Halliday, 2007; Hoekstra et al., 2010).
Although twinning has been studied extensively, much of the work involving risk factors for twinning was conducted before fertility treatments were in widespread use. Given the steady increase in use of assisted reproduction, understanding the factors associated with multiple births in this population is important (Centers for Disease Control and Prevention et al., 2011). In addition, few studies have evaluated factors associated with twinning among mothers whose offspring have birth defects (Tang et al., 2006; Zhang et al., 2011). Our objectives were to use data from the National Birth Defects Prevention Study (NBDPS) to evaluate maternal demographic factors and periconceptional exposures associated with twinning, stratified by use of fertility treatments. We assessed these associations among mothers of unaffected controls. We also included mothers of infants or fetuses with a birth defect so that we might compare these findings with those of control mothers. Because twinning is associated with an increased risk of birth defects, we were interested in factors associated with twinning that were unique to the case group, as we hypothesized that these factors may be related to both the birth defect and twinning. To minimize heterogeneity, we selected one phenotype—isolated cleft lip with/without cleft palate or cleft palate only (cases)—as these are some of the more common birth defects that have previously been associated with twinning (Mastroiacovo et al., 1999; Tang et al., 2006; Zhang et al., 2011).
Materials and Methods
Study Population
The NBDPS was a multi-center case–control study of major birth defects in the United States that completed data collection in 2013. NBDPS is a collaborative effort of the Centers for Birth Defects Research and Prevention in Arkansas, California, Georgia, Iowa, Massachusetts, North Carolina, New Jersey, New York, Texas, and Utah. Institutional Review Boards at each site approved the study. Methods for recruitment of participants and data collection have been described in detail (Yoon et al., 2001; Rasmussen et al., 2003). Briefly, eligible cases included infants or fetuses with major birth defects identified through population-based surveillance systems at each site. Controls, live-born infants without major birth defects, were randomly selected using birth certificates or birth hospital records from the same ascertainment area and time period as the cases. Per study protocol, only one infant per family was eligible for NBDPS participation; when both twins met inclusion criteria, the first-born twin was included.
Mothers of cases and controls participated in a computer-assisted telephone interview, which included questions regarding pregnancy history, demographics, and exposures that occurred from 3 months before conception through the end of the pregnancy. Mothers were interviewed in English or Spanish between 6 weeks and 24 months after their expected date of delivery (EDD).
Our study population included mothers of control twins (n = 228) and singletons (n = 8242), and mothers of isolated cleft case twins (n = 117) and singletons (n = 2859) with EDD between October 1, 1997 and December 31, 2007. Mothers of higher order multiples were excluded. Clinical information was reviewed by a clinical geneticist (S.A.R.) to identify cases with isolated clefts (no additional unrelated major defect and no known genetic conditions) (Rasmussen et al., 2003).
Outcome
The outcome of interest for this analysis was twin pregnancy, as compared to singleton pregnancy. During the interview, mothers were asked, “In this pregnancy, how many babies were you carrying?” If necessary, a second question was asked, “Did you have a single baby, twins, or more babies?” Secondary sources of plurality information were birth certificates and/or maternal medical records. Mothers of 17 controls and five cases did not answer the plurality question, but clinical records indicated they were singletons. Approximately 18% of maternally reported twin control infants (n = 41/228) and twin cases (n = 21/117) were reported as singletons on the birth certificate. This could be due to clerical errors or to death of a co-twin in utero. Therefore, we elected to defer to the maternal interview response. All infants reported as singletons during the interview were also identified as singletons on birth certificates. One control mother was excluded due to missing information on plurality in both information sources.
Exposure
We examined the association between twinning and maternal characteristics that were previously reported to be associated with twinning including fertility treatments, race/ethnicity, age, height, prepregnancy weight, prepregnancy body mass index, parity, education, income, tobacco smoking, oral contraceptive use, and use of a folic acid-containing multivitamin. All exposures were self-reported by mothers. Fertility treatment was defined as any use of fertility-enhancing medications (e.g., clomiphene citrate) and/or ART (in vitro fertilization [IVF], gamete intrafallopian transfer, zygote intrafallopian transfer, tubal embryo transfer, and intracytoplasmic sperm injection). Women were excluded from the analyses stratified by use of fertility treatments if they reported use of only nonmedical fertility treatments (e.g., consumption of teas, use of acupuncture). As our focus was on maternal characteristics associated with twinning, mothers reporting only paternal treatments (e.g., vasectomy reversal) were also excluded.
Maternal cigarette smoking, oral contraceptives, and folic acid-containing multivitamins were assessed for the exposure window from 1 month before through the first month of pregnancy. To be consistent with previous analyses of twinning and body composition, maternal height and maternal prepregnancy weight were examined separately and were categorized as quartiles among mothers of singleton controls (height: < 159, 159–163, 164–168, and > 168 cm; prepregnancy weight: < 57, 57–64, 65–74, > 74 kg) (Basso et al., 2004; Reddy et al., 2005; Hoekstra et al., 2010). Prepregnancy BMI was categorized according to National Institutes of Health guidelines: underweight (< 18.5), normal weight (18.5–24.9), overweight (25–29.9), and obese (≥ 30) (National Heart Lung and Blood Institute, ). Study site and year of EDD were also included as covariates.
Statistical Analyses
Logistic regression analyses were used to estimate crude odds ratios (ORs) and corresponding 95% confidence intervals (CI). Models were also stratified by fertility treatment, comparing maternal fertility use to unassisted conception. In the analyses of mothers who reported unassisted conceptions, we calculated adjusted estimates using multivariable logistic regression, controlling for covariates selected a priori using causal diagrams, also known as directed acyclic graphs (Greenland et al., 1999).
Previous studies have shown that predictors of twinning may vary depending on zygosity (Basso et al., 2004; Hankins and Saade, 2005; Hoekstra et al., 2010). The NBDPS does not routinely collect information on zygosity or sex of the co-twin. Therefore, the sex of many of the co-twins was obtained through linkage with birth certificates using maternal name, infant name, and infant date of birth to merge records. The co-twin's sex for 176 of 228 control twin pairs (77.2%) was identified: 60 male–male pairs, 52 female–female pairs, and 64 male–female pairs. These data were not available for Utah participants; therefore the twin (n = 17) and singleton (n = 591) controls from this Center were excluded from the zygosity sub-analysis. Due to small sample size, the zygosity sub-analysis was not conducted for case twins among which there were 49 (60.5%) same sex pairs, and 32 (39.5%) unlike sex pairs.
Unlike-sex twin pairs are dizygotic (DZ), but the zygosity of like-sex pairs cannot be identified without further information. To estimate the zygosity of like-sex pairs, we used a simulation modeling approach. The steps in this approach were: calculate the proportion of male twins in our sample, estimate the proportion of DZ twins among control twins, estimate the proportion of MZ twins among the like-sex twins in our sample, simulate 1,000 datasets with zygosity randomly assigned to each like-sex twin pair, estimate ORs for each factor of interest in each dataset using logistic regression, and, finally, obtain summary ORs and 95% uncertainty intervals for each factor of interest (see Appendix). The parameters for modeling zygosity were obtained from equations described in 2009 by Hardin et al. We also estimated ORs and 95% CIs for the association between the variables of interest and twinning for the like-sex and unlike-sex pairs as a more traditional method of accounting for zygosity. SAS version 9.3 (Cary, NC) was used to conduct all analyses.
Results
Approximately 2.7% (n = 228/8470) of control mothers reported a twin gestation compared with 3.9% (n = 117/2976) of case mothers (i.e., fetus/infant with orofacial cleft). The interview participation rate was 68.4% for mothers of cases and 65.7% for mothers of controls. Approximately 31.1% of mothers of control twins and 29.9% of mothers of case twins reported use of fertility treatments (Table 1). Fertility treatment use was significantly associated with twinning for control mothers (OR, 14.5; 95% CI, 10.7–19.8) and case mothers (OR, 9.5; 95% CI, 6.2–14.8). ART use and clomiphene citrate use were significantly associated with twinning among control mothers (OR, 51.0; 95% CI, 31.8–81.7; and OR, 6.1, 95% CI, 3.5–10.7, respectively) and case mothers (OR, 23.6; 95% CI, 12.8–43.6; and OR, 5.3, 95% CI, 2.5–11.1, respectively).
| Controls | Isolated orofacial clefts | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mothers of twins | Mothers of singletons | Mothers of twins | Mothers of singletons | |||||||||||
| Maternal characteristic | n | % | n | % | cOR | LCL | UCL | n | % | n | % | cOR | LCL | UCL |
| Total | 228 | 8242 | 117 | 2859 | ||||||||||
| Fertility treatment use (any) | ||||||||||||||
| Yes | 71 | 31.1a | 249 | 3.0 | 14.5 | 10.7 | 19.8 | 35 | 29.9 | 121 | 4.2 | 9.5 | 6.2 | 14.8 |
| No | 155 | 68.0 | 7906 | 95.9 | Ref | 82 | 70.1 | 2706 | 94.7 | Ref | ||||
| Assisted reproductive technology use | ||||||||||||||
| Yes | 39 | 17.1 | 39 | 0.5 | 51.0 | 31.8 | 81.7 | 20 | 17.1 | 28 | 1.0 | 23.6 | 12.8 | 43.6 |
| No | 155 | 68.0 | 7906 | 95.9 | Ref | 82 | 70.1 | 2706 | 94.7 | Ref | ||||
| Clomiphene citrate use | ||||||||||||||
| Yes | 15 | 6.6 | 125 | 1.5 | 6.1 | 3.5 | 10.7 | 9 | 7.7 | 56 | 2.0 | 5.3 | 2.5 | 11.1 |
| No | 155 | 68.0 | 7906 | 95.9 | Ref | 82 | 70.1 | 2706 | 94.7 | Ref | ||||
| Age at delivery (years) | ||||||||||||||
| <25 | 39 | 17.1 | 2802 | 34.0 | 0.6 | 0.4 | 0.9 | 27 | 23.1 | 992 | 34.7 | 0.7 | 0.4 | 1.1 |
| 25–29 | 55 | 24.1 | 2273 | 27.6 | Ref | 31 | 26.5 | 769 | 26.9 | Ref | ||||
| 30–34 | 79 | 34.7 | 2044 | 24.8 | 1.6 | 1.1 | 2.3 | 35 | 29.9 | 667 | 23.3 | 1.3 | 0.8 | 2.1 |
| >35 | 55 | 24.1 | 1123 | 13.6 | 2.0 | 1.4 | 3.0 | 24 | 20.5 | 431 | 15.1 | 1.4 | 0.8 | 2.4 |
| Race/ethnicity | ||||||||||||||
| Non-Hispanic white | 158 | 69.3 | 4828 | 58.6 | Ref | 78 | 66.7 | 1803 | 63.1 | Ref | ||||
| Non-Hispanic black | 31 | 13.6 | 927 | 11.3 | 1.0 | 0.7 | 1.5 | 10 | 8.6 | 169 | 5.9 | 1.4 | 0.7 | 2.7 |
| Hispanic | 27 | 11.8 | 1944 | 23.6 | 0.4 | 0.3 | 0.6 | 22 | 18.8 | 682 | 23.9 | 0.7 | 0.5 | 1.2 |
| Other | 12 | 5.3 | 534 | 6.5 | 0.7 | 0.4 | 1.2 | 7 | 6.0 | 204 | 7.1 | 0.8 | 0.4 | 1.7 |
| Height (cm) | ||||||||||||||
| <159 | 53 | 23.3 | 2084 | 25.3 | Ref | 23 | 19.7 | 756 | 26.4 | Ref | ||||
| 159–163 | 56 | 24.6 | 2085 | 25.3 | 1.1 | 0.7 | 1.5 | 30 | 25.6 | 675 | 23.6 | 1.5 | 0.8 | 2.5 |
| 164–168 | 53 | 23.3 | 1874 | 22.7 | 1.1 | 0.8 | 1.6 | 23 | 19.7 | 644 | 22.5 | 1.2 | 0.7 | 2.1 |
| >168 | 62 | 27.2 | 1881 | 22.8 | 1.3 | 0.9 | 1.9 | 36 | 30.8 | 666 | 23.3 | 1.8 | 1.0 | 3.0 |
| Pre-pregnancy weight (kg) | ||||||||||||||
| <57 | 48 | 21.1 | 2060 | 25.0 | Ref | 22 | 18.8 | 720 | 25.2 | Ref | ||||
| 57–64 | 56 | 24.6 | 2327 | 28.3 | 1.0 | 0.7 | 1.5 | 31 | 26.5 | 759 | 26.7 | 1.3 | 0.8 | 2.3 |
| 65–75 | 66 | 29.0 | 1880 | 22.8 | 1.5 | 1.0 | 2.2 | 27 | 23.1 | 639 | 22.4 | 1.4 | 0.8 | 2.5 |
| >75 | 53 | 23.3 | 1875 | 22.8 | 1.2 | 0.8 | 1.8 | 36 | 30.8 | 698 | 24.4 | 1.7 | 1.0 | 2.9 |
| Pre-pregnancy body mass index (kg/m2) | ||||||||||||||
| Underweight (<18.5) | 10 | 4.4 | 426 | 5.2 | 0.9 | 0.5 | 1.7 | 8 | 6.8 | 184 | 6.4 | 1.1 | 0.5 | 2.4 |
| Normal (18.5–24.9) | 117 | 51.3 | 4347 | 52.7 | Ref | 55 | 47.9 | 1437 | 50.3 | Ref | ||||
| Overweight (25–29.9) | 55 | 24.1 | 1794 | 21.8 | 1.1 | 0.8 | 1.6 | 24 | 20.5 | 598 | 20.9 | 1.0 | 0.6 | 1.7 |
| Obese (> 30) | 38 | 16.7 | 1317 | 16.0 | 1.1 | 0.7 | 1.6 | 25 | 21.4 | 506 | 17.7 | 1.3 | 0.8 | 2.1 |
| Parity | ||||||||||||||
| 0 | 94 | 41.2 | 3286 | 39.9 | Ref | 48 | 41.0 | 1123 | 29.3 | Ref | ||||
| 1 | 75 | 32.9 | 2730 | 33.1 | 1.0 | 0.7 | 1.3 | 37 | 31.6 | 976 | 34.1 | 0.9 | 0.6 | 1.4 |
| 2+ | 59 | 25.9 | 2206 | 26.8 | 0.9 | 0.7 | 1.3 | 32 | 27.4 | 751 | 26.3 | 1.0 | 0.6 | 1.6 |
| Education | ||||||||||||||
| < High school graduate | 22 | 9.7 | 1547 | 18.8 | 0.7 | 0.4 | 1.1 | 13 | 11.1 | 573 | 19.1 | 0.7 | 0.3 | 1.3 |
| High school graduate | 42 | 18.4 | 1974 | 24.0 | Ref | 27 | 23.1 | 761 | 26.6 | Ref | ||||
| > High school graduate | 164 | 71.9 | 4714 | 57.2 | 1.6 | 1.2 | 2.3 | 77 | 65.8 | 1524 | 53.3 | 1.4 | 0.9 | 2.2 |
| Annual household income | ||||||||||||||
| < $10,000 | 26 | 11.4 | 1447 | 17.6 | 0.9 | 0.6 | 1.4 | 19 | 16.2 | 573 | 20.0 | 0.9 | 0.5 | 1.6 |
| $10,000-$50,000 | 113 | 49.6 | 2549 | 30.9 | Ref | 48 | 41.0 | 838 | 29.3 | Ref | ||||
| > $50,000 | 71 | 31.1 | 3431 | 41.6 | 2.1 | 1.6 | 2.9 | 45 | 38.5 | 1234 | 43.2 | 1.6 | 1.0 | 2.4 |
| Smokingb | ||||||||||||||
| Yes | 41 | 18.0 | 1492 | 18.1 | 1.0 | 0.7 | 1.4 | 24 | 20.5 | 693 | 24.2 | 0.8 | 0.8 | 1.3 |
| No | 187 | 82.0 | 6627 | 80.4 | Ref | 92 | 78.6 | 2135 | 74.7 | Ref | ||||
| Oral contraceptive useb | ||||||||||||||
| Yes | 15 | 6.6 | 614 | 7.5 | 0.9 | 0.5 | 1.5 | 10 | 8.6 | 221 | 7.7 | 1.1 | 0.6 | 2.2 |
| No | 211 | 93 | 7581 | 92.0 | Ref | 107 | 91.5 | 2621 | 91.7 | Ref | ||||
| Folic acid useb | ||||||||||||||
| Yes | 142 | 62.3 | 4132 | 50.1 | 1.6 | 1.2 | 2.1 | 76 | 65.0 | 1364 | 47.7 | 2.0 | 1.4 | 3.0 |
| No | 86 | 37.7 | 4076 | 49.5 | Ref | 41 | 35.0 | 1486 | 52.0 | Ref | ||||
| Study site | ||||||||||||||
| Arkansas | 19 | 8.3 | 1050 | 12.7 | 0.7 | 0.4 | 1.2 | 12 | 10.3 | 321 | 11.2 | 1.4 | 0.6 | 3.3 |
| California | 8 | 3.5 | 1018 | 12.4 | 0.3 | 0.1 | 0.6 | 15 | 12.8 | 455 | 15.9 | 1.2 | 0.5 | 2.8 |
| Georgia | 24 | 10.5 | 866 | 10.5 | Ref | 9 | 7.7 | 328 | 11.5 | Ref | ||||
| Iowa | 36 | 15.8 | 899 | 10.9 | 1.4 | 0.9 | 2.4 | 9 | 7.7 | 308 | 10.8 | 1.1 | 0.4 | 2.7 |
| Massachusetts | 51 | 22.4 | 977 | 11.9 | 1.9 | 1.2 | 3.1 | 19 | 16.2 | 391 | 13.7 | 1.7 | 0.8 | 4.0 |
| New Jersey | 27 | 11.8 | 546 | 6.6 | 1.8 | 1.0 | 3.1 | 7 | 6.0 | 156 | 5.5 | 1.6 | 0.6 | 4.5 |
| New York | 12 | 5.3 | 718 | 8.7 | 0.6 | 0.3 | 1.2 | 19 | 16.2 | 233 | 8.2 | 3.0 | 1.3 | 6.7 |
| North Carolina | 14 | 6.1 | 580 | 7.0 | 0.9 | 0.4 | 1.7 | 7 | 6.0 | 164 | 5.7 | 1.6 | 0.6 | 4.3 |
| Texas | 20 | 8.8 | 989 | 12.0 | 0.7 | 0.4 | 1.3 | 9 | 7.7 | 326 | 11.4 | 1.0 | 0.4 | 2.6 |
| Utah | 17 | 7.5 | 599 | 7.3 | 1.0 | 0.5 | 1.9 | 11 | 9.4 | 177 | 6.2 | 2.3 | 0.9 | 5.7 |
| Year of estimated date of delivery | ||||||||||||||
| 1997 | 2 | 0.9 | 103 | 1.3 | c | 0 | 0.0 | 38 | 1.3 | c | ||||
| 1998 | 29 | 12.7 | 733 | 8.9 | 1.8 | 1.0 | 3.4 | 13 | 11.1 | 266 | 9.3 | 1.0 | 0.5 | 2.2 |
| 1999 | 22 | 9.7 | 842 | 10.2 | 1.2 | 0.6 | 2.3 | 16 | 13.7 | 327 | 11.4 | 1.0 | 0.5 | 2.1 |
| 2000 | 26 | 11.4 | 871 | 10.6 | 1.4 | 0.7 | 2.6 | 13 | 11.1 | 291 | 10.2 | 0.9 | 0.4 | 2.0 |
| 2001 | 22 | 9.7 | 775 | 9.4 | 1.3 | 0.3 | 2.5 | 14 | 12.0 | 285 | 10.0 | 1.0 | 0.5 | 2.2 |
| 2002 | 22 | 9.7 | 683 | 8.3 | 1.5 | 0.8 | 2.8 | 10 | 8.6 | 246 | 8.6 | 0.8 | 0.4 | 1.9 |
| 2003 | 20 | 8.8 | 875 | 10.6 | 1.1 | 0.6 | 2.0 | 6 | 5.1 | 222 | 7.8 | 0.6 | 0.2 | 1.5 |
| 2004 | 19 | 8.3 | 890 | 10.8 | 1.0 | 0.5 | 1.9 | 8 | 6.8 | 299 | 10.5 | 0.6 | 0.3 | 1.3 |
| 2005 | 26 | 11.4 | 835 | 10.1 | 1.5 | 0.8 | 2.7 | 12 | 10.3 | 305 | 10.7 | 0.8 | 0.4 | 1.8 |
| 2006 | 23 | 10.1 | 841 | 10.2 | 1.3 | 0.7 | 2.4 | 11 | 9.4 | 289 | 10.0 | 0.8 | 0.4 | 1.8 |
| 2007 | 17 | 7.5 | 792 | 9.6 | Ref | 14 | 12.0 | 290 | 10.1 | Ref | ||||
- Results in bold indicate statistical significance at p <0.05; cOR, crude odds ratio; LCL, lower 95% confidence limit; UCL, upper 95% confidence limit; Ref, referent category.
- a Percentages may not sum to 100 due to missing values.
- b Any reported use 1 month prior to pregnancy through 1 month after conception.
- c Not calculated for cell size < 4.
Results were generally similar for case and control mothers (Table 1). Among control mothers, twinning increased with increasing maternal age: 58.8% of mothers of twins were age 30 years or greater, compared with 38.4% of mothers of singletons. Among control mothers, other factors significantly associated with an increased prevalence of twinning in bivariate analyses were higher education (> than a high school graduate), higher income (> $50,000 per year), and use of a folic acid-containing multivitamin. Hispanic control mothers were also less likely to have twins compared with non-Hispanic white mothers. Among mothers of cases with clefts, significant predictors of twinning were taller maternal height, higher maternal income, and use of a folic-acid containing multivitamin. A sensitivity analysis restricted to mothers who reported plurality during the interview that matched birth certificates (control twins: n = 187; case twins: n = 96) resulted in very similar findings (data not shown).
Several factors were found to be significantly associated with twinning among control mothers who reported unassisted conception (Table 2). For these women, the association between non-Hispanic black race and twinning was of borderline significance after adjusting for study site (adjusted odds ratio [aOR], 1.6; 95% CI, 1.0–2.4). Increasing parity was modestly associated with twinning, with ORs of borderline statistical significance after adjusting for maternal age, race/ethnicity, education level, annual household income, and study site (one previous live birth: aOR 1.4, 95% CI 0.9–2.1; two+ previous live births: aOR 1.6, 95% CI 1.0–2.5). Maternal tobacco smoking was significantly associated with twinning after adjusting for maternal age, race/ethnicity, education level, annual household income, parity, study site, and year of EDD (aOR 1.6, 95% CI 1.1–2.4).
| Unassisted conception | Fertility treatment use | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mothers of twins | Mothers of singletons | Mothers of twins | Mothers of singletons | ||||||||||||||
| Maternal characteristic | n | % | n | % | cOR | LCL | UCL | aOR | LCL | UCL | n | % | n | % | cOR | LCL | UCL |
| N | 155 | 7906 | 71 | 249 | |||||||||||||
| Age at delivery (years) | |||||||||||||||||
| <25 | 39 | 25.2 | 2767 | 35.0 | 0.7 | 0.4 | 1.0 | 0.7 | 0.5 | 1.2 | 0 | 0.0 | 18 | 7.2a | c | ||
| 25–29 | 46 | 29.7 | 2188 | 27.7 | Ref | Refb | 8 | 11.3 | 54 | 21.7 | Ref | ||||||
| 30–34 | 39 | 25.2 | 1920 | 24.3 | 1.0 | 0.6 | 1.5 | 1.0 | 0.6 | 1.6 | 39 | 54.9 | 98 | 39.4 | 2.7 | 1.2 | 6.2 |
| >35 | 31 | 20.0 | 1031 | 13.0 | 1.4 | 0.9 | 2.3 | 1.4 | 0.9 | 2.3 | 24 | 33.8 | 79 | 31.7 | 2.1 | 0.9 | 4.9 |
| Race/ethnicity | |||||||||||||||||
| Non-Hispanic white | 91 | 58.7 | 4561 | 57.7 | Ref | Refd | 65 | 91.6 | 209 | 83.9 | Ref | ||||||
| Non-Hispanic black | 29 | 18.7 | 906 | 11.5 | 1.6 | 1.1 | 2.5 | 1.6 | 1.0 | 2.4 | 2 | 2.8 | 11 | 4.4 | c | ||
| Hispanic | 25 | 16.1 | 1909 | 24.2 | 0.7 | 0.4 | 1.0 | 0.7 | 0.4 | 1.0 | 2 | 2.8 | 18 | 7.3 | c | ||
| Other | 10 | 6.5 | 521 | 6.6 | 1.0 | 0.5 | 1.9 | 1.0 | 0.5 | 1.8 | 2 | 2.8 | 11 | 4.4 | c | ||
| Height (cm) | |||||||||||||||||
| <159 | 35 | 22.6 | 2020 | 25.6 | Ref | Refe | 17 | 23.9 | 44 | 17.8 | Ref | ||||||
| 159–163 | 47 | 30.3 | 2007 | 25.4 | 1.4 | 0.9 | 2.2 | 1.3 | 0.9 | 2.1 | 9 | 12.7 | 62 | 24.9 | 0.4 | 0.2 | 0.9 |
| 164–170 | 34 | 21.9 | 1802 | 22.8 | 1.1 | 0.7 | 1.8 | 1.1 | 0.7 | 1.8 | 19 | 26.8 | 61 | 24.5 | 0.8 | 0.4 | 1.7 |
| >170 | 35 | 22.6 | 1783 | 22.6 | 1.2 | 0.7 | 1.9 | 1.1 | 0.7 | 1.8 | 26 | 36.6 | 80 | 32.1 | 0.8 | 0.4 | 1.7 |
| Pre-pregnancy weight (kg) | |||||||||||||||||
| <57 | 34 | 21.9 | 2009 | 25.4 | Ref | Reff | 12 | 16.9 | 40 | 16.1 | Ref | ||||||
| 57–64 | 37 | 23.9 | 2241 | 28.4 | 1.0 | 0.6 | 1.6 | 0.9 | 0.6 | 1.6 | 19 | 26.8 | 64 | 25.7 | 1.2 | 0.4 | 2.3 |
| 65–75 | 43 | 27.7 | 1806 | 22.8 | 1.4 | 0.9 | 2.2 | 1.4 | 0.9 | 2.3 | 23 | 32.4 | 55 | 22.1 | 1.4 | 0.6 | 3.1 |
| >75 | 36 | 23.2 | 1771 | 22.4 | 1.2 | 0.7 | 1.9 | 1.2 | 0.7 | 2.0 | 17 | 23.9 | 90 | 36.1 | 0.6 | 0.3 | 1.4 |
| Pre-pregnancy body mass index (kg/m2) | |||||||||||||||||
| Underweight (<18.5) | 7 | 4.5 | 419 | 5.3 | 0.9 | 0.4 | 2.0 | 1.1 | 0.5 | 2.4 | 2 | 4.1 | 5 | 2.0 | 1.3 | 0.2 | 6.9 |
| Normal (18.5–24.9) | 78 | 50.3 | 4188 | 53.0 | Ref | Reff | 38 | 53.5 | 123 | 49.4 | Ref | ||||||
| Overweight (25–29.9) | 34 | 21.9 | 1720 | 21.8 | 1.1 | 0.7 | 1.6 | 1.1 | 0.7 | 1.7 | 21 | 29.6 | 61 | 24.5 | 1.1 | 0.6 | 2.1 |
| Obese (> 30) | 28 | 18.1 | 1245 | 15.8 | 1.2 | 0.7 | 1.8 | 1.2 | 0.8 | 2.0 | 10 | 14.1 | 58 | 23.3 | 0.6 | 0.3 | 1.2 |
| Parity | |||||||||||||||||
| 0 | 47 | 30.3 | 3114 | 39.4 | Ref | Refg | 46 | 64.8 | 142 | 57.0 | Ref | ||||||
| 1 | 55 | 35.5 | 2629 | 33.3 | 1.4 | 1.0 | 2.1 | 1.4 | 0.9 | 2.1 | 19 | 26.8 | 75 | 30.1 | 0.8 | 0.4 | 1.4 |
| 2+ | 53 | 34.2 | 2162 | 27.4 | 1.7 | 1.1 | 2.5 | 1.6 | 1.0 | 2.5 | 6 | 8.5 | 32 | 12.9 | 0.6 | 0.2 | 1.5 |
| Education | |||||||||||||||||
| < High school graduate | 21 | 13.6 | 1509 | 19.1 | 0.7 | 0.4 | 1.2 | 0.8 | 0.4 | 1.3 | 1 | 1.4 | 8 | 3.2 | c | ||
| High school graduate | 38 | 24.5 | 1929 | 24.4 | Ref | Refh | 4 | 5.6 | 31 | 12.5 | Ref | ||||||
| > High school graduate | 96 | 61.9 | 4461 | 56.4 | 1.1 | 0.7 | 1.6 | 1.0 | 0.6 | 1.4 | 66 | 93.0 | 210 | 84.3 | 2.4 | 0.8 | 7.2 |
| Annual household income | |||||||||||||||||
| < $10,000 | 25 | 16.1 | 1429 | 18.1 | 0.9 | 0.6 | 1.5 | 1.1 | 0.7 | 1.8 | 1 | 1.4 | 14 | 5.6 | c | ||
| $10,000-$50,000 | 64 | 41.3 | 3332 | 42.2 | Ref | Refi | 7 | 9.9 | 148 | 59.4 | Ref | ||||||
| > $50,000 | 54 | 34.8 | 2374 | 30.0 | 1.2 | 0.8 | 1.7 | 1.0 | 0.7 | 1.5 | 58 | 81.7 | 77 | 30.9 | 4.3 | 1.9 | 9.9 |
| Smokingj | |||||||||||||||||
| Yes | 38 | 24.5 | 1464 | 18.5 | 1.4 | 1.0 | 2.0 | 1.6 | 1.1 | 2.4 | 3 | 4.2 | 19 | 7.6 | c | ||
| No | 117 | 75.5 | 6345 | 80.3 | Ref | Reff | 68 | 95.8 | 229 | 92.0 | Ref | ||||||
| Oral contraceptive usej | |||||||||||||||||
| Yes | 10 | 6.5 | 603 | 7.6 | 0.8 | 0.4 | 1.6 | 0.8 | 0.4 | 1.6 | 5 | 7.0 | 7 | 2.8 | 2.6 | 0.8 | 8.5 |
| No | 144 | 92.9 | 7278 | 92.1 | Ref | Refg | 66 | 93.0 | 242 | 97.2 | Ref | ||||||
| Folic acid usej | |||||||||||||||||
| Yes | 73 | 47.1 | 3874 | 49.0 | 0.9 | 0.7 | 1.3 | 0.8 | 0.6 | 1.2 | 67 | 94.4 | 217 | 87.2 | 2.5 | 0.8 | 7.2 |
| No | 82 | 52.9 | 4016 | 50.8 | Ref | Reff | 4 | 5.6 | 32 | 12.9 | Ref | ||||||
| Study site | |||||||||||||||||
| Arkansas | 16 | 10.3 | 1005 | 12.7 | 0.7 | 0.4 | 1.5 | 0.8 | 0.4 | 1.5 | 3 | 4.2 | 33 | 13.3 | c | ||
| California | 8 | 5.2 | 996 | 12.6 | 0.4 | 0.2 | 0.9 | 0.4 | 0.2 | 0.9 | 0 | 0.0 | 11 | 4.4 | c | ||
| Georgia | 18 | 11.6 | 835 | 10.6 | Ref | Refk | 6 | 8.5 | 22 | 8.5 | Ref | ||||||
| Iowa | 24 | 15.5 | 845 | 10.7 | 1.3 | 0.7 | 2.4 | 1.3 | 0.7 | 2.5 | 12 | 16.9 | 43 | 17.3 | 1.0 | 0.3 | 3.1 |
| Massachusetts | 21 | 13.6 | 921 | 11.7 | 1.1 | 0.6 | 2.0 | 1.1 | 0.6 | 2.0 | 30 | 42.3 | 52 | 20.9 | 2.1 | 0.8 | 5.8 |
| New Jersey | 16 | 10.3 | 531 | 6.7 | 1.4 | 0.7 | 2.8 | 1.2 | 0.6 | 2.4 | 11 | 15.5 | 10 | 4.0 | 4.0 | 1.2 | 14.0 |
| New York | 9 | 5.8 | 690 | 8.7 | 0.6 | 0.3 | 1.4 | 0.6 | 0.3 | 1.3 | 2 | 2.8 | 20 | 8.0 | c | ||
| North Carolina | 12 | 7.7 | 555 | 8.0 | 1.0 | 0.5 | 2.1 | 1.3 | 0.6 | 2.8 | 2 | 2.8 | 17 | 6.8 | c | ||
| Texas | 19 | 12.3 | 958 | 12.1 | 0.9 | 0.5 | 1.8 | 0.9 | 0.5 | 1.8 | 1 | 1.4 | 18 | 7.2 | c | ||
| Utah | 12 | 7.7 | 570 | 7.2 | 1.0 | 0.5 | 2.0 | 1.2 | 0.6 | 2.7 | 4 | 5.6 | 23 | 9.2 | 0.6 | 0.2 | 2.6 |
| Year of estimated date of delivery | |||||||||||||||||
| 1997 | 1 | 0.7 | 96 | 1.2 | c | c | 1 | 1.4 | 1 | 0.4 | c | ||||||
| 1998 | 19 | 12.3 | 705 | 8.9 | 1.7 | 0.8 | 3.6 | 1.9 | 0.9 | 4.0 | 9 | 12.7 | 19 | 7.7 | 2.3 | 0.7 | 7.9 |
| 1999 | 17 | 11.0 | 800 | 10.1 | 1.4 | 0.6 | 2.9 | 1.5 | 0.7 | 3.2 | 5 | 7.0 | 30 | 12.1 | 0.8 | 0.2 | 3.1 |
| 2000 | 17 | 11.0 | 837 | 10.6 | 1.3 | 0.6 | 2.8 | 1.4 | 0.7 | 3.2 | 9 | 12.7 | 26 | 10.4 | 1.7 | 0.5 | 5.7 |
| 2001 | 17 | 11.0 | 748 | 9.5 | 1.4 | 0.7 | 3.1 | 1.6 | 0.7 | 3.5 | 5 | 7.0 | 19 | 7.6 | 1.3 | 0.3 | 5.0 |
| 2002 | 15 | 9.7 | 666 | 8.4 | 1.4 | 0.7 | 3.1 | 1.6 | 0.7 | 3.6 | 7 | 9.9 | 14 | 5.6 | 2.4 | 0.6 | 9.0 |
| 2003 | 13 | 8.4 | 836 | 10.6 | 1.0 | 0.5 | 2.2 | 1.0 | 0.4 | 2.1 | 7 | 9.9 | 31 | 12.5 | 1.1 | 0.3 | 3.8 |
| 2004 | 11 | 7.1 | 843 | 10.7 | 0.8 | 0.4 | 1.9 | 0.9 | 0.4 | 1.9 | 7 | 9.9 | 33 | 13.3 | 1.0 | 0.3 | 3.6 |
| 2005 | 18 | 11.6 | 793 | 10.0 | 1.4 | 0.7 | 3.0 | 1.5 | 0.7 | 3.1 | 8 | 11.3 | 31 | 12.5 | 1.2 | 0.4 | 4.3 |
| 2006 | 15 | 9.7 | 815 | 10.3 | 1.2 | 0.5 | 2.5 | 1.2 | 0.6 | 2.6 | 8 | 11.3 | 21 | 8.4 | 1.8 | 0.5 | 6.5 |
| 2007 | 12 | 7.7 | 765 | 9.7 | Ref | Refk | 5 | 7.0 | 24 | 9.6 | Ref | ||||||
- Results in bold indicate statistical significance at p <0.05; cOR, crude odds ratio; aOR, adjusted odds ratio; LCL, lower 95% confidence limit; UCL, upper 95% confidence limit; Ref, referent category.
- a Percentages may not sum to 100 due to missing values.
- b Adjusted for maternal race/ethnicity, education level, annual household income, study site, year of expected date of delivery (EDD)
- c OR not calculated for cell size < 4.
- d Adjusted for study site.
- e Adjusted for year of mother's birth, maternal race/ethnicity, study site.
- f Adjusted for maternal age, race/ethnicity, height, education level, annual household income, parity, study site, year of EDD.
- Adjusted for maternal age, race/ethnicity, education level, annual household income, parity, study site, year of EDD.
- g Adjusted for maternal age, race/ethnicity, education level, annual household income, study site.
- h Adjusted for maternal age, race/ethnicity, study site, year of EDD.
- i Adjusted for maternal age, race/ethnicity, education level, study site, year of EDD.
- j Any reported use 1 month prior to pregnancy through 1 month after conception.
- k Model included study site and year of EDD.
Among the control mothers who reported any use of fertility treatments, twinning was more frequent among mothers aged 30 to 34 years compared with mothers aged 25 to 29 years (Table 2). The proportion of non-Hispanic white mothers was slightly higher among mothers of twins (91.6%) than among mothers of singletons (83.9%). The odds of twinning were 4.3 times higher for mothers with an annual household income ≥ $50,000 compared with those with an income between $10,000 and $50,000 (95% CI, 1.9–9.9). Twinning was less common among mothers 159 to 163 cm tall than among mothers <159 cm tall.
Among case mothers who did not report use of fertility treatments, non-Hispanic black women were more than twice as likely as non-Hispanic white women to have a twin pregnancy (aOR, 2.3; 95% CI, 1.1–4.6) (Table 3). Compared with women with no previous live births, women with at least two previous live births had a modestly increased risk of a twin pregnancy that was of borderline statistical significance (aOR, 1.7; 95% CI, 0.9–3.1). Mothers from New York were also significantly more likely to have a twin pregnancy than their counterparts from Georgia, although this association was of borderline significance after adjusting for year of EDD. Overall, the associations for case mothers were similar to the findings from the controls analysis, with the notable exception that there was no association observed for smoking and twinning among case mothers reporting unassisted conception. We did not observe any significant associations with twinning among case mothers who reported use of fertility treatments, although the small sample size limited our ability to detect associations in this group.
| Unassisted conception | Fertility treatment use | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mothers of twins | Mothers of singletons | Mothers of twins | Mothers of singletons | ||||||||||||||
| Maternal characteristic | n | % | n | % | cOR | LCL | UCL | aOR | LCL | UCL | n | % | n | % | cOR | LCL | UCL |
| N | 82 | 2706 | 35 | 121 | |||||||||||||
| Age at delivery (years) | |||||||||||||||||
| <25 | 26 | 31.7 | 974 | 36.0 | 0.8 | 0.4 | 1.4 | 0.7 | 0.4 | 1.3 | 1 | 2.9 | 9 | 7.4 | c | ||
| 25–29 | 25 | 30.5 | 730 | 27.0 | Ref | Refb | 6 | 17.1 | 35 | 28.9 | Ref | ||||||
| 30–34 | 21 | 25.6 | 617 | 22.8 | 1.0 | 0.6 | 1.8 | 1.0 | 0.6 | 1.9 | 14 | 40.0 | 40 | 33.1 | 2.0 | 0.7 | 5.9 |
| >35 | 10 | 12.2 | 385 | 14.2 | 0.8 | 0.4 | 1.6 | 0.8 | 0.4 | 1.6 | 14 | 40.0 | 37 | 30.6 | 2.2 | 0.8 | 6.4 |
| Race/ethnicity | |||||||||||||||||
| Non-Hispanic white | 46 | 56.1 | 1681 | 62.1a | Ref | Refd | 32 | 91.4 | 100 | 82.6 | Ref | ||||||
| Non-Hispanic black | 10 | 12.2 | 166 | 6.1 | 2.2 | 1.1 | 4.4 | 2.3 | 1.1 | 4.6 | 0 | 0.0 | 2 | 1.7 | c | ||
| Hispanic | 21 | 25.6 | 664 | 24.5 | 1.2 | 0.7 | 2.0 | 1.2 | 0.7 | 2.0 | 1 | 2.9 | 10 | 8.3 | c | ||
| Other | 5 | 6.1 | 194 | 7.2 | 0.9 | 0.4 | 2.4 | 0.9 | 0.4 | 2.4 | 2 | 5.7 | 9 | 7.4 | c | ||
| Height (cm) | |||||||||||||||||
| <159 | 17 | 20.7 | 721 | 26.6 | Ref | Refe | 6 | 17.1 | 28 | 23.1 | Ref | ||||||
| 159–163 | 20 | 24.4 | 640 | 23.7 | 1.3 | 0.7 | 2.6 | 1.4 | 0.7 | 2.6 | 10 | 28.6 | 30 | 24.8 | 1.6 | 0.5 | 4.8 |
| 164–170 | 13 | 15.9 | 607 | 22.4 | 0.9 | 0.4 | 1.9 | 1.0 | 0.5 | 2.0 | 10 | 28.6 | 30 | 24.8 | 1.6 | 0.5 | 4.8 |
| >170 | 27 | 32.9 | 633 | 23.4 | 1.8 | 1.0 | 3.4 | 1.9 | 0.9 | 1.4 | 9 | 23.7 | 29 | 24.0 | 1.4 | 0.5 | 4.6 |
| Pre-pregnancy weight (kg) | |||||||||||||||||
| <57 | 14 | 17.1 | 692 | 25.6 | Ref | Reff | 8 | 22.9 | 23 | 19.0 | Ref | ||||||
| 57–64 | 19 | 23.2 | 725 | 26.8 | 1.3 | 0.6 | 2.6 | 1.0 | 0.5 | 2.0 | 12 | 34.3 | 29 | 24.0 | 1.2 | 0.4 | 3.4 |
| 65–75 | 20 | 24.4 | 611 | 22.6 | 1.6 | 0.8 | 3.2 | 1.3 | 0.6 | 2.7 | 7 | 20.0 | 25 | 20.7 | 0.8 | 0.3 | 2.6 |
| >75 | 28 | 34.2 | 646 | 23.9 | 2.1 | 1.1 | 4.1 | 1.6 | 0.8 | 3.2 | 8 | 22.9 | 42 | 34.7 | 0.5 | 0.2 | 1.7 |
| Pre-pregnancy body mass index (kg/m2) | |||||||||||||||||
| Underweight (<18.5) | 6 | 7.3 | 181 | 6.7 | 1.4 | 0.6 | 3.3 | 1.5 | 0.6 | 3.6 | 2 | 5.7 | 2 | 1.7 | c | ||
| Normal (18.5–24.9) | 33 | 40.2 | 1370 | 50.6 | Ref | Refg | 22 | 62.9 | 58 | 47.9 | Ref | ||||||
| Overweight (25–29.9) | 19 | 23.2 | 564 | 20.8 | 1.4 | 0.8 | 2.5 | 1.2 | 0.6 | 2.2 | 5 | 3.1 | 26 | 21.5 | 0.5 | 0.2 | 1.5 |
| Obese (> 30) | 19 | 23.2 | 470 | 17.4 | 1.7 | 0.9 | 3.0 | 1.6 | 0.9 | 2.9 | 6 | 17.1 | 31 | 25.6 | 0.5 | 0.2 | 1.4 |
| Parity | |||||||||||||||||
| 0 | 26 | 31.7 | 1036 | 38.3 | Ref | Refh | 22 | 62.9 | 72 | 59.5 | Ref | ||||||
| 1 | 28 | 34.2 | 932 | 34.4 | 1.2 | 0.7 | 2.1 | 1.3 | 0.7 | 2.3 | 9 | 25.7 | 37 | 30.6 | 0.8 | 0.3 | 1.9 |
| 2+ | 28 | 34.2 | 737 | 27.2 | 1.5 | 0.9 | 2.6 | 1.7 | 0.9 | 3.1 | 4 | 11.4 | 12 | 9.9 | 1.1 | 0.3 | 3.7 |
| Education | |||||||||||||||||
| < High school graduate | 13 | 15.9 | 556 | 20.6 | 0.7 | 0.4 | 1.4 | 0.7 | 0.3 | 1.3 | 0 | 0.0 | 7 | 5.8 | c | ||
| High school graduate | 25 | 30.5 | 740 | 27.4 | Ref | Refi | 2 | 5.7 | 13 | 10.7 | Ref | ||||||
| > High school graduate | 44 | 53.7 | 1410 | 52.1 | 0.9 | 0.6 | 1.5 | 1.0 | 0.6 | 1.6 | 33 | 94.3 | 100 | 82.6 | c | ||
| Annual household income | |||||||||||||||||
| < $10,000 | 18 | 22.0 | 564 | 20.8 | 1.1 | 0.6 | 1.9 | 1.2 | 0.6 | 2.1 | 1 | 2.9 | 9 | 7.4 | c | ||
| $10,000-$50,000 | 36 | 43.9 | 1190 | 44.0 | Ref | Refj | 9 | 25.7 | 33 | 27.3 | Ref | ||||||
| > $50,000 | 23 | 28.1 | 752 | 27.8 | 1.0 | 0.6 | 1.7 | 0.9 | 0.5 | 1.7 | 25 | 71.4 | 77 | 63.6 | 1.2 | 0.5 | 2.8 |
| Smokingk | |||||||||||||||||
| Yes | 18 | 22.0 | 676 | 25.0 | 0.8 | 0.5 | 1.4 | 0.9 | 0.5 | 1.5 | 6 | 17.1 | 9 | 7.4 | 2.6 | 0.8 | 7.8 |
| No | 63 | 76.8 | 2008 | 74.2 | Ref | Refg | 29 | 82.9 | 112 | 92.6 | Ref | ||||||
| Oral contraceptive usek | |||||||||||||||||
| Yes | 8 | 9.8 | 218 | 8.1 | 1.2 | 0.6 | 2.6 | 1.2 | 0.5 | 2.6 | 2 | 5.7 | 2 | 1.7 | c | ||
| No | 74 | 90.2 | 2480 | 91.7 | Ref | Refh | 33 | 94.3 | 119 | 98.4 | Ref | ||||||
| Folic acid usek | |||||||||||||||||
| Yes | 42 | 51.2 | 1246 | 46.1 | 1.2 | 0.8 | 1.9 | 1.2 | 0.8 | 2.0 | 34 | 97.1 | 100 | 82.6 | c | ||
| No | 40 | 48.8 | 1457 | 53.8 | Ref | Refg | 1 | 2.9 | 21 | 17.4 | Ref | ||||||
| Study site | |||||||||||||||||
| Arkansas | 10 | 12.2 | 307 | 11.4 | 1.4 | 0.5 | 3.8 | 1.4 | 0.5 | 3.8 | 2 | 5.7 | 10 | 8.3 | c | ||
| California | 14 | 17.1 | 435 | 16.1 | 1.4 | 0.6 | 3.5 | 1.4 | 0.6 | 3.5 | 1 | 2.9 | 13 | 10.7 | c | ||
| Georgia | 7 | 8.5 | 303 | 11.2 | Ref | Refl | 2 | 5.7 | 22 | 18.2 | Ref | ||||||
| Iowa | 9 | 11.0 | 290 | 10.7 | 1.3 | 0.5 | 3.7 | 1.4 | 0.5 | 3.7 | 0 | 0.0 | 13 | 10.7 | c | ||
| Massachusetts | 9 | 11.0 | 357 | 13.2 | 1.1 | 0.4 | 3.0 | 1.1 | 0.4 | 3.0 | 10 | 28.6 | 29 | 24.0 | c | ||
| New Jersey | 2 | 2.4 | 150 | 5.5 | c | c | 5 | 14.3 | 5 | 4.1 | c | ||||||
| New York | 14 | 17.1 | 223 | 8.2 | 2.7 | 1.1 | 6.8 | 2.5 | 1.0 | 6.3 | 5 | 14.3 | 8 | 6.6 | c | ||
| North Carolina | 3 | 7.3 | 158 | 5.8 | c | c | 4 | 11.4 | 5 | 4.1 | c | ||||||
| Texas | 8 | 9.8 | 315 | 11.6 | 1.1 | 0.4 | 3.1 | 1.0 | 0.4 | 2.9 | 1 | 2.9 | 7 | 5.8 | c | ||
| Utah | 6 | 7.3 | 168 | 6.2 | 1.5 | 0.5 | 4.7 | 1.8 | 0.6 | 5.7 | 5 | 14.3 | 9 | 7.4 | c | ||
| Year of estimated date of delivery | |||||||||||||||||
| 1997 | 0 | 0.0 | 36 | 1.3 | c | c | 0 | 0.0 | 0 | 0.0 | c | ||||||
| 1998 | 9 | 11.0 | 253 | 9.4 | 1.4 | 0.5 | 3.9 | 1.6 | 0.6 | 4.5 | 4 | 11.4 | 9 | 7.4 | 0.5 | 0.1 | 2.4 |
| 1999 | 8 | 9.8 | 308 | 11.4 | 1.0 | 0.4 | 2.9 | 1.1 | 0.4 | 3.3 | 8 | 22.9 | 16 | 13.2 | 0.6 | 0.2 | 2.1 |
| 2000 | 11 | 13.4 | 278 | 10.3 | 1.6 | 0.6 | 4.1 | 1.6 | 0.6 | 4.5 | 2 | 5.7 | 7 | 5.8 | c | ||
| 2001 | 12 | 14.6 | 271 | 10.0 | 1.8 | 0.7 | 4.6 | 1.9 | 0.7 | 5.0 | 2 | 5.7 | 12 | 9.9 | c | ||
| 2002 | 7 | 8.5 | 235 | 8.7 | 1.2 | 0.4 | 3.4 | 1.2 | 0.4 | 3.7 | 3 | 8.6 | 7 | 5.8 | c | ||
| 2003 | 4 | 4.9 | 202 | 7.5 | 0.8 | 0.2 | 2.7 | 0.9 | 0.2 | 3.1 | 2 | 5.7 | 16 | 13.2 | c | ||
| 2004 | 7 | 8.5 | 281 | 10.4 | 1.0 | 0.3 | 2.9 | 1.0 | 0.3 | 2.9 | 1 | 2.9 | 16 | 13.2 | c | ||
| 2005 | 10 | 12.2 | 289 | 10.7 | 1.4 | 0.5 | 3.7 | 1.3 | 0.5 | 3.6 | 2 | 5.7 | 13 | 10.7 | c | ||
| 2006 | 7 | 8.5 | 272 | 10.1 | 1.0 | 0.4 | 3.0 | 1.0 | 0.3 | 2.9 | 4 | 11.4 | 17 | 14.1 | 0.3 | 0.1 | 1.2 |
| 2007 | 7 | 8.5 | 280 | 10.4 | Ref | Refl | 7 | 20.0 | 8 | 6.6 | Ref | ||||||
- Results in bold indicate statistical significance at p < 0.05; cOR, crude odds ratio; aOR, adjusted odds ratio; LCL, lower 95% confidence limit; UCL, upper 95% confidence limit; Ref, referent category.
- a Percentages may not sum to 100 due to missing values.
- b Adjusted for maternal race/ethnicity, education level, annual household income, study site, year of expected date of delivery (EDD).
- c OR not calculated for cell size < 4.
- d Adjusted for study site.
- e Adjusted for year of mother's birth, maternal race/ethnicity, study site.
- f Adjusted for maternal age, race/ethnicity, height, education level, annual household income, parity, study site, year of EDD.
- g Adjusted for maternal age, race/ethnicity, education level, annual household income, parity, study site, year of EDD.
- h Adjusted for maternal age, race/ethnicity, education level, annual household income, study site.
- i Adjusted for maternal age, race/ethnicity, study site, year of EDD.
- j Adjusted for maternal age, race/ethnicity, education level, study site, year of EDD.
- k Any reported use 1 month prior to pregnancy through 1 month after conception.
- l Model included study site and year of EDD.
Associations with twinning for the unlike-sex control twins and estimated dizygotic twins were similar to the associations observed for all control twins (Table 4). Fewer associations were observed for the like-sex and estimated monozygotic (MZ) control twins.
| Unlike-sex twins | Dizygotic twins (estimated) | Like-sex twins | Monozygotic twins (estimated) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maternal characteristic | n | cOR | LCL | UCL | cOR | LUI | UUI | n | cOR | LCL | UCL | cOR | LUI | UUI |
| Fertility treatment use (any) | ||||||||||||||
| Yes | 29 | 26.5 | 16.0 | 44.3 | 14.7 | 12.6 | 16.9 | 30 | 11.7 | 7.6 | 18.2 | 9.6 | 5.4 | 14.7 |
| No | 35 | Ref | Ref | 82 | Ref | Ref | ||||||||
| Assisted reproductive technology use | ||||||||||||||
| Yes | 16 | 84.6 | 43.3 | 165.3 | 59.7 | 49.1 | 71.2 | 17 | 38.4 | 20.9 | 70.6 | 40.1 | 17.7 | 66.2 |
| No | 35 | Ref | Ref | 82 | Ref | Ref | ||||||||
| Clomiphene citrate use | ||||||||||||||
| Yes | 8 | 14.9 | 6.7 | 32.8 | 10.2 | 7.8 | 12.9 | 8 | 6.3 | 3 | 13.4 | 6.6 | 1.7 | 12.4 |
| No | 35 | Ref | Ref | 82 | Ref | Ref | ||||||||
| Age at delivery (years)a | ||||||||||||||
| <25 | 8 | 0.9 | 0.3 | 2.4 | 0.7 | 0.5 | 0.9 | 18 | 0.6 | 0.3 | 1.1 | 0.6 | 0.3 | 1.2 |
| 25–29 | 7 | Ref | Ref | 24 | Ref | Ref | ||||||||
| 30–34 | 11 | 1.7 | 0.7 | 4.4 | 1.3 | 0.9 | 1.7 | 22 | 1.0 | 0.6 | 1.8 | 1.1 | 0.5 | 2.0 |
| >35 | 9 | 2.6 | 1.0 | 7.0 | 1.9 | 1.3 | 2.6 | 18 | 1.5 | 0.8 | 2.8 | 1.6 | 0.7 | 3.2 |
| Race/ethnicitya | ||||||||||||||
| Non-Hispanic white | 24 | Ref | Ref | 48 | Ref | Ref | ||||||||
| Non-Hispanic black | 7 | 1.3 | 0.6 | 3.1 | 1.5 | 1.0 | 1.9 | 17 | 1.6 | 0.9 | 2.8 | 1.7 | 0.7 | 3.0 |
| Hispanic | 4 | 0.4 | 0.1 | 1.1 | 0.4 | 0.3 | 0.6 | 11 | 0.5 | 0.3 | 1.0 | 0.5 | 0.2 | 1.0 |
| Other | 0 | b | 0.6 | 0.2 | 1.0 | 6 | 1.1 | 0.5 | 2.5 | 1.1 | 0.0 | 2.4 | ||
| Height (cm)a | ||||||||||||||
| <159 | 7 | Ref | Ref | 15 | Ref | Ref | ||||||||
| 159–163 | 12 | 1.8 | 0.7 | 4.5 | 1.7 | 1.3 | 2.3 | 24 | 1.6 | 0.9 | 3.1 | 1.8 | 0.8 | 4.1 |
| 164–170 | 7 | 1.2 | 0.4 | 3.3 | 1.4 | 1.0 | 2.0 | 20 | 1.6 | 0.8 | 3.1 | 1.8 | 0.7 | 4.0 |
| >170 | 9 | 1.5 | 0.6 | 4.1 | 1.6 | 1.1 | 2.3 | 21 | 1.7 | 0.9 | 3.2 | 1.9 | 0.7 | 4.4 |
| Pre-pregnancy weight (kg)a | ||||||||||||||
| <57 | 5 | Ref | Ref | 18 | Ref | Ref | ||||||||
| 57–64 | 8 | 1.4 | 0.5 | 4.4 | 1.3 | 0.9 | 1.8 | 23 | 1.2 | 0.6 | 2.1 | 1.3 | 0.5 | 2.7 |
| 65–75 | 9 | 2.0 | 0.7 | 6.1 | 1.7 | 1.1 | 2.4 | 23 | 1.4 | 0.8 | 2.7 | 1.6 | 0.6 | 3.4 |
| >75 | 11 | 2.5 | 0.9 | 7.1 | 1.6 | 1.1 | 2.3 | 17 | 1.1 | 0.5 | 2.1 | 1.2 | 0.5 | 2.5 |
| Pre-pregnancy body mass index (kg/m2)a | ||||||||||||||
| Underweight (<18.5) | 1 | b | 0.6 | 0.2 | 1.0 | 3 | b | 1.0 | 0.4 | 1.9 | ||||
| Normal (18.5–24.9) | 18 | Ref | Ref | 43 | Ref | Ref | ||||||||
| Overweight (25–29.9) | 6 | 0.8 | 0.3 | 2.0 | 1.0 | 0.7 | 1.3 | 20 | 1.1 | 0.6 | 1.8 | 1.2 | 0.5 | 2.2 |
| Obese (> 30) | 8 | 1.5 | 0.6 | 3.4 | 1.2 | 0.9 | 1.5 | 13 | 1.0 | 0.5 | 1.8 | 1.0 | 0.4 | 1.9 |
| Paritya | ||||||||||||||
| 0 | 9 | Ref | Ref | 28 | Ref | Ref | ||||||||
| 1 | 14 | 1.9 | 0.9 | 4.8 | 1.4 | 1.1 | 1.9 | 28 | 1.2 | 0.7 | 2.0 | 1.3 | 0.6 | 2.4 |
| 2+ | 12 | 2.0 | 0.9 | 4.8 | 1.6 | 1.2 | 2.2 | 26 | 1.4 | 0.8 | 2.4 | 1.5 | 0.7 | 2.8 |
| Educationa | ||||||||||||||
| < High school graduate | 4 | 0.6 | 0.2 | 1.9 | 0.6 | 0.4 | 0.9 | 11 | 0.7 | 0.3 | 1.5 | 0.7 | 0.2 | 1.4 |
| High school graduate | 9 | Ref | Ref | 21 | Ref | Ref | ||||||||
| > High school graduate | 22 | 1.1 | 0.5 | 2.4 | 1.1 | 0.9 | 1.4 | 50 | 1.1 | 0.6 | 1.8 | 1.1 | 0.6 | 2.1 |
| Annual household incomea | ||||||||||||||
| < $10,000 | 6 | 1.7 | 0.6 | 4.8 | 1.1 | 0.8 | 1.5 | 14 | 0.9 | 0.5 | 1.6 | 0.9 | 0.4 | 1.8 |
| $10,000-$50,000 | 16 | Ref | Ref | 29 | Ref | Ref | ||||||||
| > $50,000 | 8 | 2.8 | 1.2 | 6.4 | 1.6 | 1.2 | 2.1 | 35 | 1.1 | 0.7 | 1.9 | 1.2 | 0.6 | 2.1 |
| Smokinga, c | ||||||||||||||
| Yes | 28 | 1.0 | 0.5 | 2.4 | 1.2 | 0.9 | 1.5 | 62 | 1.3 | 0.8 | 2.2 | 1.4 | 0.7 | 2.3 |
| No | 7 | Ref | Ref | 20 | Ref | Ref | ||||||||
| Oral contraceptive usea, c | ||||||||||||||
| Yes | 1 | b | 0.9 | 0.5 | 1.3 | 8 | 1.3 | 0.6 | 2.7 | 1.3 | 0.3 | 2.5 | ||
| No | 34 | Ref | Ref | 73 | Ref | Ref | ||||||||
| Folic acid usea, c | ||||||||||||||
| Yes | 20 | 1.5 | 0.7 | 2.8 | 1.0 | 0.8 | 1.3 | 34 | 0.8 | 0.5 | 1.2 | 0.8 | 0.4 | 1.3 |
| No | 15 | Ref | Ref | 48 | Ref | Ref | ||||||||
- Comparison group for all analyses was mothers of singleton controls. Results in bold indicate statistical significance at p < 0.05; cOR, crude odds ratio; LCL, lower 95% confidence limit; UCL, upper 95% confidence limit; LUI, lower 95% uncertainty interval value; UUI, upper 95% uncertainty interval value; Ref, referent category.
- a Analysis restricted to mothers who reported unassisted conception.
- b OR not calculated for cell size <4.
- c Any reported use 1 month prior to pregnancy through 1 month after conception.
Discussion
Twin pregnancies occurred in approximately 2.7% of control mothers in the NBDPS, similar to the U.S. twin birth rate of 3% during the same time period (Martin et al., 2013). As expected, fertility treatment use was a significant predictor of twinning, both for mothers of controls and of cases with isolated orofacial clefts. Our results support previous reports of an association between fertility treatments and MZ twinning (Aston et al., 2008). Given the magnitude of the associations for ART and clomiphene citrate, it may appear that our results indicate a greater contribution of ART births to the overall twinning rate compared with non-ART treatments, in contrast to previous studies (Kulkarni et al., 2013). However, when comparing the proportion of twins attributable to IVF with non-IVF treatments, without adjusting for maternal age, our results (16.7% of twins and 14.5%, respectively) were similar to those of Kulkarni et al. (2013). We did not find any evidence to suggest a difference in the factors associated with twinning for unaffected controls and cases with orofacial clefts.
Historically, maternal age has been cited as a strong predictor of twinning (Bulmer, 1970; Bortolus et al., 1999). A recent report found the natural dizygotic twinning rate was relatively stable between 1969 and 2009 after controlling for maternal age (Derom et al., 2011). We found an association between maternal age and twinning for mothers reporting assisted conception but not among mothers reporting unassisted conception. One explanation for the discrepancy may be that we could not account for zygosity in our primary analyses, and previous studies have suggested that the association with maternal age may be limited to mothers of DZ twins (Bulmer, 1970). In our zygosity sub-analysis, we observed a trend of increased frequency of twinning with increasing maternal age for MZ and DZ twins, although the association was not statistically significant for MZ twin mothers. Our finding that the association between maternal age and twinning was attenuated after controlling for fertility treatment use, maternal race/ethnicity, education level, annual household income, study site, and year of EDD may suggest that this association is more complex than previously described.
Other factors associated with both fertility treatments and twinning such as education, prepregnancy weight, and use of a folic acid-containing multivitamin were associated with twinning when not controlling for fertility treatment use but were no longer associated after the models were stratified by fertility treatment use. The possibility of an association between folic acid and twinning has been particularly controversial (Werler et al., 1997; Li et al., 2003b). Our study found little difference in folic acid intake during the pregnancies of twin and singleton mothers reporting unassisted conception. In the ART stratum, almost all mothers reported taking folic acid. Although more twin mothers reported taking folic acid, this association was not statistically significant.
Among mothers who reported unassisted conception, a moderate increase in the frequency of twinning was observed for mothers who were non-Hispanic black, who reported two or more previous live births, and who smoked cigarettes between 1 month before conception through the first month of pregnancy, which is consistent with previous findings (Bulmer, 1970; Nylander, 1981; Hoekstra et al., 2010).
The associations we observed for mothers reporting fertility treatments likely reflect the cost of fertility treatments or choices regarding treatment options, such as implanting multiple embryos, rather than causal factors. The association between income and twinning may be due to treatments such as IVF being cost-prohibitive to lower income families and many insurers do not provide coverage for these treatments (American Society for Reproductive Medicine, ). Cost has been previously cited as a factor related to the socioeconomic and ethnic disparities among women using fertility treatments (Smith et al., 2011). Similarly, the large proportion of twin births in MA are likely due to state mandates that insurers provide coverage for fertility treatments, including IVF (Martin et al., 2011). For women receiving IVF, choices regarding the number of embryos implanted are an important consideration, although not one that we were able to analyze.
Our study has several limitations. First, our study was limited by the relatively small sample size after stratifying by fertility treatment use and estimated zygosity. We were unable to conduct multivariable analyses for mothers reporting fertility treatment use. We relied on self-reported data from a retrospective maternal interview, so we cannot rule out exposure misclassification due to inaccurate recall. The average age at interview was 9 months for controls (singletons: 9.3 months; twins: 10.1 months) and 11 months for cases (singletons, 10.7 months; twins, 11.3 months). The study participation rate was slightly higher among mothers of twins than mothers of singletons for both controls (singletons, 65.4%; twins, 68.7%) and cases (singletons, 68.2%; twins, 71.6%). We were not able to verify the accuracy of the responses for reported periconceptional exposures or reported use of fertility treatments. For mothers who reported fertility treatment use, we were unable to determine the number of embryos implanted, a strong predictor of twinning (Templeton and Morris, 1998). Another limitation is that a comparison of the plurality reported by the mothers in the interview with information recorded on the infant's birth certificate or mother's hospital record revealed some discrepancies, with mothers reporting higher rates of twin gestation. Although previous studies have found a high degree of concordance between plurality from maternal report and on birth certificates, some variability exists and may be due to clerical errors or early fetal demise of a co-twin (Querec, 1980; Schoendorf et al., 1993). Ascertainment of early fetal demise has likely increased because these previous studies due to increased use of early ultrasonography. A sensitivity analysis restricted to control infants without plurality discrepancies produced results similar to those from the primary analysis.
We were also unable to directly determine zygosity. This limitation is important because many factors have only been associated with DZ twinning (Bulmer, 1970; Hoekstra et al., 2010). Zygosity is particularly difficult to obtain as the gold-standard for determining zygosity is genetic analysis (Chen et al., 1999). However, our simulation modeling approach may be useful as it allowed us to estimate risk factor associations for MZ and DZ twins with accompanying uncertainty intervals. Although we attempted to assess factors associated with zygosity of twins, there are other features of twinning, such as chorionicity, that we were not able to assess using these data.
Strengths of this study include use of a demographically diverse, population-based sample from 10 different states across the United States. We were able to control for a variety of factors associated with twinning. This analysis assesses potential risk factors for twinning among a modern sample of mothers that reported fertility treatment use in addition to mothers that reported unassisted conception of twins.
Fertility treatment use was a strong predictor of twinning, as expected, but the factors associated with twinning among women receiving fertility treatments are likely due, in part, to the type of treatment, number of embryos implanted, and the availability of insurance coverage. We observed an increase in twinning with increasing maternal age, but factors such as maternal race/ethnicity and socioeconomic status may contribute and should be examined further. Given the increased risk of adverse outcomes associated with a twin pregnancy, understanding the factors associated with twinning, be it unassisted or assisted, is of public health importance.
Acknowledgments
The authors thank the Centers for Birth Defects Research and Prevention in AR, CA, GA, IA, MA, NJ, NY, NC, TX, and UT for their data; and the families who participated in the NBDPS. Disclosure statement: The authors report no conflict of interest.
Appendix

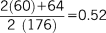
 is the proportion of male twins, a is the number of male-male twin pairs (60 in our sample), b is the number of male-female twin pairs (64 in our sample), and n is the total number of twin pairs in the sample (176 in our sample). The proportion of male twins in our analysis was therefore calculated as:
is the proportion of male twins, a is the number of male-male twin pairs (60 in our sample), b is the number of male-female twin pairs (64 in our sample), and n is the total number of twin pairs in the sample (176 in our sample). The proportion of male twins in our analysis was therefore calculated as:
 ) in our total sample of like-sex and unlike-sex twins (Hardin et al., 2009):
) in our total sample of like-sex and unlike-sex twins (Hardin et al., 2009):

 is the proportion of female twins (
is the proportion of female twins (
 ). The proportion of DZ twins in our sample was therefore estimated as:
). The proportion of DZ twins in our sample was therefore estimated as:
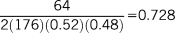
We estimated the total number of DZ twin pairs in our sample to be 128 (72.8% of 176 twin pairs). The 64 unlike-sex twins were assumed to be DZ and 64 of the like-sex twin pairs estimated to be DZ (n = 128–64). There were 112 total like-sex twins, and therefore we estimated that the remaining 43% (n = 48) of like-sex pairs were MZ.
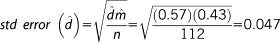
 is the probability of monozygosity, given a twin pair is like-sex. If the value from the uniform distribution was less than the value from the normal distribution, the twin pair was designated as MZ; otherwise the twin pair was designated as DZ. All unlike-sex twins were assigned as DZ.
is the probability of monozygosity, given a twin pair is like-sex. If the value from the uniform distribution was less than the value from the normal distribution, the twin pair was designated as MZ; otherwise the twin pair was designated as DZ. All unlike-sex twins were assigned as DZ.We estimated unadjusted ORs using logistic regression models for each exposure of interest, with singletons as the referent group, stratified by estimated zygosity. For exposures other than fertility treatment use, the analysis was restricted to mothers who reported unassisted conception. OR estimates for all 1,000 datasets were compiled, and our summary OR estimates were obtained by calculating the median, with the 2.5 and 97.5 percentiles comprising the lower and upper bounds of our uncertainly intervals, respectively.




