Lead brownfields and birth defects in North Carolina 2003–2015: A cross-sectional case–control study
Abstract
Background
Brownfields consist of abandoned and disused sites, spanning many former purposes. Brownfields represent a heterogenous yet ubiquitous exposure for many Americans, which may contain hazardous wastes and represent urban blight. Neonates and pregnant individuals are often sensitive to subtle environmental exposures. We evaluate if residential exposure to lead (Pb) brownfields is associated with birth defects.
Methods
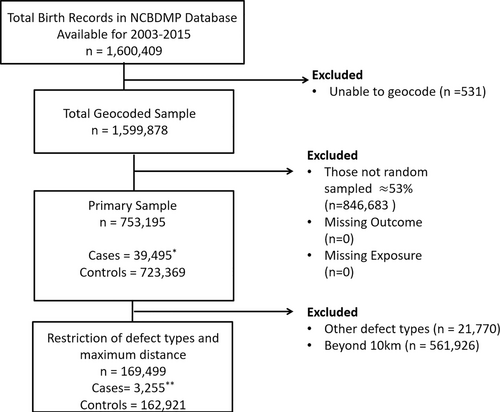
Using North Carolina birth records from 2003 to 2015, we sampled 169,499 births within 10 km of a Pb brownfield with 3255 cardiovascular, central nervous, or external defects identified. Exposure was classified by binary specification of residing within 3 km of a Pb brownfield. We utilized multivariable logistic regression models adjusted for demographic covariates available from birth records and 2010 Census to estimate odds ratios (OR) and 95% confidence intervals (CI). Effect measure modification was assessed by inclusion of interaction terms and stratification for the potential modifiers of race/ethnicity and diabetes status.
Results
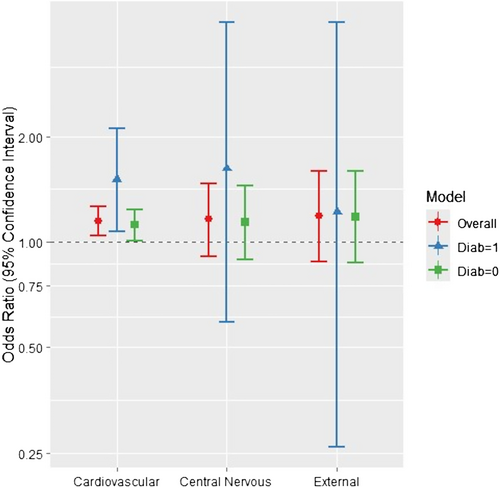
We observed positive associations between cardiovascular birth defects and residential proximity to Pb brownfields, OR (95%CI): 1.15 (1.04, 1.26), with suggestive positive associations for central nervous 1.16 (0.91, 1.47) and external defects 1.19 (0.88, 1.59). We did observe evidence of effect measure modification via likelihood ratio tests (LRT) for race/ethnicity for central nervous and external defect groups (LRT p values 0.08 and 0.02). We did observe modification by diabetes status for the cardiovascular group (LRT p value 0.08).
Conclusions
Our results from this analysis indicate that residential proximity to Pb brownfields is associated with cardiovascular birth defects with suggestive associations for central nervous and external defects. In-depth analyses of individual defects and other contaminants or brownfield site functions may reveal additional novel associations.
1 BACKGROUND
Birth defects remain the leading cause of infant mortality and are major contributors to infant morbidity and disability in the United States (Driscoll & Ely, 2020). Birth defects impose serious costs on health networks and communities in which they occur (Waitzman et al., 1994). Much of the etiology of birth defects remains unknown, yet often environmental in utero exposures are associated with increased risk of various defects (Hansen et al., 2009; L. Wang et al., 2019; Yoon et al., 2001). Further, birth defects have been linked to environmental exposures associated with hazardous materials like heavy metals, including lead (Pb) which is known to be a strong neurotoxin (Al-Hadithi et al., 2012; Sanders et al., 2014; Vinceti et al., 2001). Researchers have observed mixed associations with exposure to hazardous waste sites, such as Superfund sites and other large scale contaminated sites, with some studies reporting positive associations and others null associations (Budnick et al., 1984; Persico et al., 2020; Suarez et al., 2007). Brownfields are defined by the U.S. Environmental Protection Agency (EPA) as any “…real property, the expansion, redevelopment, or reuse of which may be complicated by the presence or potential presence of a hazardous substance, pollutant, or contaminant” with recent research linking residential exposure to brownfields with birth defects prevalence (EPA, 2023; Slawsky et al., 2022). Previous literature has also noted variations in the prevalence of birth defects by racial and ethnic grouping, which may be of interest in the historical context of redlining and the locations of some brownfields in minoritized neighborhoods (Canfield et al., 2006; Canfield et al., 2014).
The mechanisms of action for brownfields impacting birth defects are still poorly understood. Brownfields can contain hazardous materials and even in the absence of detectable contamination may represent a substantial aesthetic nuisance and stressor in communities near brownfield sites. This analysis builds on prior study to examine associations between residential proximity to brownfield sites with Pb contamination and prevalence of birth defects (Slawsky et al., 2022). We hypothesize that proximity to Pb brownfields is associated with an increase in the prevalence of birth defects and those in close proximity, within 3 km or less, may see stronger associations. We emphasize Pb contamination as previous study has already established a link between brownfield proximity and birth defects and now material interest is placed in understanding the types of brownfields and associations with birth defects (Slawsky et al., 2022). For example, whether contaminated sites are more strongly associated than non-contaminated sites or whether the former function of the site (e.g., gas station vs. heavy industry factory) alter associations. We prioritize Pb contamination for its neurotoxic effects and Pb contamination being more commonly found at smaller size brownfields. We define Pb brownfields as sites with confirmed measurable amounts of Pb, but Pb may not be the predominate contaminant at a given site. Additionally, minoritized populations may be disproportionally impacted by brownfield proximity due to historical redlining and locating of hazardous sites in minoritized neighborhoods. To gain further understanding on mechanisms there is also interest in examining potential effect measure modification by diabetes status as previous literature has identified diabetes status as an important factor in some birth defects. Additionally, diabetes outcomes are closely related to neighborhood characteristics like healthcare access and food access (Hill-Briggs et al., 2021; Sanders et al., 2014; Tinker et al., 2020). Thus, our aims for this analysis are to estimate the association between proximity to Pb brownfields and central nervous, cardiovascular, or external birth defects. These defect types are thought to be most relevant for Pb exposure and demonstrated suggestive associations in a previous analysis with any residential brownfield exposure (Slawsky et al., 2022; Vinceti et al., 2001). We also aim to examine potential modification by race/ethnicity and diabetes status.
This analysis will shed further light on the relationship between brownfields and birth defect prevalence, provide insight into possible mechanisms of action from residential proximity to Pb contaminated sites, and identify potential at risk groups. Results from this analysis may indicate the need for more targeted efforts to remediate brownfields by class of contamination, or in minoritized populations which may be disproportionally impacted, to reduce the overall burden of birth defects in addition to highlighting potential at-risk groups like those with diabetes.
2 METHODS
2.1 Study population
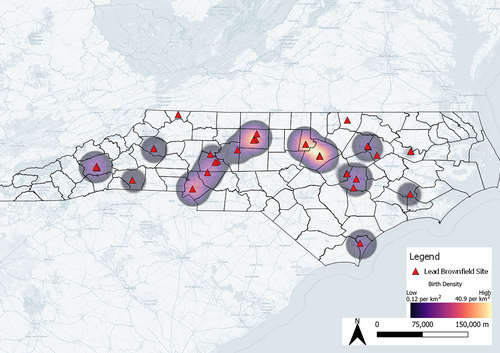
Data from North Carolina birth records and the North Carolina Birth Defects Monitoring Program (NCBDMP) were utilized to identify live-born singleton births from 2003 to 2015. NCBDMP is an active surveillance birth defects registry, which means they follow the birth cohort identified through vital statistics/birth registry data through the first year of life and document any birth defects that are diagnosed during that period (in addition to any birth defects that were diagnosed at delivery and included on the birth certificate). This is important for complete ascertainment as many birth defects are not immediately identified at birth itself but become apparent during the infant period. Trained NCBDMP staff systematically review and abstract hospital medical records, combined with information from hospital discharge records, vital records, and Medicaid claims, to identify infants born with a birth defect that are diagnosed within the first year of life. The NCDMP database has been utilized in prior studies and is considered representative for the state (Meyer & Siega-Riz, 2002; Nelson et al., 2016; Rappazzo et al., 2019). In August 2010, North Carolina adopted the 2003 revision of the U.S. Standard Birth Certificate, which resulted in modifications to the way many variables are collected and for the transition year some variables were not collected. Due to these changes, smoking and diabetes status were not available for analysis in 2010. Of the more than 1.6 million births available from 2003 to 2015, we restricted to a random sample of those with a residence at date of delivery within 10 km of a Pb brownfield (n = 169,499) as those beyond this limit are assumed to have little to no residential contact with the site. Cases for this analysis included all identified births with at least one cardiovascular, central nervous, or external birth defect (n = 3255). Controls for this analysis were considered on the basis they did not have a recorded birth defect, low birth weight (<2500 g), or preterm birth (<37 weeks gestational age) per standard guidelines with a final control sample of 162,921 births (CDC, 2021). Addresses recorded at delivery were considered the principal residence and were geolocated using address, city, state and ZIP in ArcGIS (ESRI, 2011). Data on gestational parent age (i.e., age of birthing parent at time of birth), race/ethnicity, prenatal care, diabetes and smoking status, were obtained from birth records. We augmented our data with American Community Survey (ACS) 5-year (2013) data to capture important area-level education data at the census block group level with the percent achieving a bachelor's degree or more and Census 2010 area level urbanicity as the percent of the block group designated as urban (Figure 1).
2.2 Exposure
We acquired data on brownfields by combining data from the North Carolina Department of Environmental Quality (NC-DEQ), and EPA's Clean Ups in my Community (CIMC) databases (EPA, 2020; NCDEQ, 2020). NC-DEQ maintains a database of all brownfields in the state. This database includes completed (i.e., remediated and restored sites) and ongoing brownfields. To ensure complete coverage, we also included the CIMC database which maintains similar data but includes all the EPA funded brownfield and hazardous waste cleanups for the entire U.S. Both databases are utilized to cross-validate and to ensure against any missing brownfield sites from being uploaded at different times. We spatially joined these two data sources to create a complete dataset of all the brownfields identified as of January 2020 in North Carolina. We then restricted to only those brownfield sites in North Carolina which had assessments with detectable levels of Pb (n = 58). Although some sites were considered remediated by January of 2020, we include them if they were still ongoing during the 2003 to 2015 timeframe. Confirmation of Pb contamination is determined during a phase one site assessment, with historical document review, a site visit, and sample collection which can be from a variety of media depending on the nature of the brownfield site (e.g., soil sample for a park or water samples at a lake) and often multiple media are sampled (EPA, 2024). Our sample included various site types with detectable Pb contamination ranging in function from abandoned gas stations to urban parks with legacy pollution from retired incinerators, but our data did not contain numeric Pb level measurements. Our primary exposure of binary distance (≤3 km vs. >3 km) to nearest Pb brownfield was calculated using a distance matrix measuring from the centroid of the residential address from the birth record to the centroid of the nearest Pb brownfield with a Hub-and-Spoke analysis and then implemented our maximum allowable distance of 10 km. 3 km (i.e., 1.86 miles) was selected as a good approximation of a neighborhood zone or area considered commonly traveled from a person's residence and has been utilized in prior studies for aspects of the built environment and cardiovascular health (Poelman et al., 2018). All spatial analyses were conducted in QGIS 3.14 (Qgis, 2019).
2.3 Outcomes
We focused the analyses on external birth defects and birth defects affecting the cardiovascular and central nervous systems identified by the NCBDMP as these defects are thought to be most impacted by Pb exposure and showed associations with any brownfield exposure in previous analyses (Slawsky et al., 2022; Vinceti et al., 2001). Central nervous system defects (i.e., neural tube defects) include anencephaly, hydrocephalus, and spina bifida. Cardiovascular system defects represent the largest group in terms of cases and include atrial septal defect, aortic valve stenosis, atrioventricular septal defect, coarctation of aorta, hypoplastic left heart syndrome, pulmonary valve atresia, transposition of the greater vessels, tetralogy of Fallot, tricuspid valve atresia, and ventricular septal defect. External defects include anophthalmia/microphthalmia, anotia/microtia, congenital cataract, lower limb reduction, and upper limb reduction. We also included models for specific groups (i.e., cardiovascular, central nervous, and external), while effect measure estimates for individual defects (e.g., atrial septal defect) are presented in supplemental materials. Individual models were performed only for those birth defects with five or more cases in stratified analyses, as defects with fewer cases do not provide interpretable estimates.
2.4 Covariates
Potential confounders were selected a priori through a combination of expert knowledge and literature review. We included: gestational parent age at delivery (in years), self-classified race/ethnicity (White, Black, Hispanic, Asian American/Pacific Islander, American Indian, Other), prenatal care (month prenatal care began), gestational parent smoking (current smoker yes/no), diabetes status (includes both gestational and pre-gestational yes/no), area level education (% of census block group with a bachelor's degree or more), and urbanicity (% of census block designated as urban). Demographic and behavioral covariates were obtained from birth records. Age, race/ethnicity, smoking habits, and diabetes status have all been documented in prior literature as important factors in various birth defects (Canfield et al., 2014; Drake et al., 2016; Gill et al., 2012; Reefhuis & Honein, 2004; Tinker et al., 2020). Prenatal care is used both to adjust for prenatal care itself but also as a proxy socioeconomic status variable (Dubay et al., 2001). Race/ethnicity is not included as a biological variable but as a proxy indicator for differential experiences of stressors related to race/ethnicity. Census covariates were collected from Census 2010 and ACS 2013, via recorded address with education noted in prior literature (Farley et al., 2002; Langlois et al., 2010). Due to changes in birth record forms smoking and diabetes are missing for 2010.
2.5 Statistical analyses
Odds ratios (OR) and 95% confidence intervals (95% CI) for brownfield exposure and birth defects were estimated using multivariable logistic regression models. All models were adjusted for gestational parent age, month prenatal care began, race/ethnicity group, ACS 2013 block group education (% with bachelor's degree or more) and Census 2010 urbanicity, gestational parent smoking status during pregnancy (yes/no), and gestational parent diabetes during pregnancy (includes both gestational and pre-gestational and is coded as yes/no). We also conducted sensitivity analyses stratifying by race/ethnicity and diabetes status to assess the potential for effect measure modification on the multiplicative scale; all models were adjusted for listed potential confounders except the stratifying variables. Likelihood ratio test p-values were calculated comparing nested models with and without an interaction term for the potential modifier and evaluated at the alpha = 0.10 level. Missingness was low and treated as random with complete case analysis performed. To test our results for robustness in changes to the diabetes item on North Carolina birth records before and after 2010 and missing for all 2010 records we conducted a series of sensitivity analyses: removing 2010 records, subsetting to before and after 2010, and models without diabetes adjustment. We also examined different distance thresholds for defining exposure with both a 1500 and 6000 m threshold. All analyses were conducted using R Version 4.2.1 (Team, R. C, 2021).
3 RESULTS
From the more than 1.6 million births in North Carolina from 2003 to 2015, our analytic sample consisted of 169,499 births that had a recorded address at date of delivery within 10 km of a Pb brownfield. This sample contained 3255 births with at least one cardiovascular, central nervous, or external defect and 162,921 control births (i.e., no defect, low birth weight, or preterm birth). Cases and controls tended to be very similar with both having an average gestational parent age of 27, average prenatal care beginning within 3 months of gestation, and similar racial/ethnic distributions. There were differences in the levels of smoking (9.8% vs. 8.8%) and diabetes (6.1% vs. 3.5%) with cases having the higher percentages (Table 1). Missingness was low among all variables with no variable having more than 10% missingness. Births tended to have the highest density around major urban centers with Pb brownfields also being located primarily in urban centers (Figure 2).
| Covariate | Case | Control |
|---|---|---|
| Mean ± SD or n (%) | ||
| n | 3255 | 162,921 |
| Distance to lead (Pb) brownfield in meters | 5430 ± (2756) | 5580 ± (2712) |
| Gestational parent age | 27.9 ± (6.5) | 27.3 ± (6.0) |
| Missing | 0 (0) | 4 (<0.01) |
| Race/ethnicity (%) | ||
| White Non-Hispanic | 1367 (42.0) | 71,218 (43.7) |
| Black Non-Hispanic | 1155 (35.5) | 52,991 (32.5) |
| Hispanic | 624 (19.2) | 31,576 (19.4) |
| Asian American/Pacific Islander | 92 (2.8) | 6309 (3.9) |
| American Indian | 8 (0.2) | 479 (0.3) |
| Other/unknown | 9 (0.3) | 348 (0.2) |
| Smoking (% current)a | ||
| Yes | 320 (9.8) | 14,298 (8.8) |
| No | 2661 (81.8) | 135,744 (83.3) |
| Missing | 274 (8.4) | 12,879 (7.9) |
| Prenatal care (month prenatal care began) | 2.8 ± (1.7) | 2.9 ± (1.6) |
| Missing | 295 (9.1) | 13,920 (8.5) |
| Education (%)b | 30.1 ± (21.2) | 30.8 ± (21.6) |
| Urbanicityb | 87.7 ± (25.9) | 87.7 ± (26.2) |
| Diabetesa | ||
| Yes | 201 (6.1) | 5771 (3.5) |
| No | 2785 (85.6) | 144,625 (88.8) |
| Missing | 269 (8.3) | 12,525 (7.7) |
- a Missing counts include births in 2010 which are missing due to administrative changes in birth certificate data collection methods.
- b From ACS 2013 data (block group level) mean percent with a bachelor's degree or more and Census 2010 mean percent designated as urban with (SD).
When evaluating the association between residential Pb brownfield exposure and cardiovascular birth defects, we observed a positive association (OR 1.15; 95% CI 1.04, 1.26) (Table 2). This result indicates that the odds of cardiovascular birth defect for those residing within 3 km of a Pb brownfield is 1.15 times as high as those living further from a Pb brownfield holding gestational parent age, race/ethnicity, prenatal care, smoking status, diabetic status, and education constant. The 95% CI of (1.04, 1.26) indicates that this study's data are relatively compatible, at an alpha level of 0.05, with a population OR between 1.04 and 1.26 for the adjusted estimate. We also observed suggestive positive associations between residential Pb brownfield exposure, central nervous, and external defects (OR 1.16; 95% CI 0.91, 1.47 and OR 1.19; 95% 0.88, 1.59, respectively).
| Birth Defects Groupa | OR | 95% CI | LRT p valueb |
|---|---|---|---|
| Cardiovascular | 1.15 | 1.04, 1.26 | – |
| Central nervous | 1.16 | 0.91, 1.47 | – |
| External | 1.19 | 0.88, 1.59 | – |
| Cardiovascular stratified by diabetes statusc | 0.08 | ||
| Diabetes absent | 1.12 | 1.01, 1.24 | – |
| Diabetes present | 1.51 | 1.07, 2.11 | – |
| Central nervous stratified by diabetes statusc | 0.39 | ||
| Diabetes absent | 1.14 | 0.89, 1.45 | – |
| Diabetes present | 1.62 | 0.59, 4.23 | – |
| External stratified by diabetes statusc | 0.95 | ||
| Diabetes absent | 1.18 | 0.87, 1.59 | – |
| Diabetes present | 1.22 | 0.26, 4.23 | – |
| Cardiovascular stratified by race/ethnicityd | 0.75 | ||
| White | 1.08 | 0.91, 1.26 | – |
| Black | 1.17 | 1.01, 1.36 | – |
| Hispanic | 1.16 | 0.91, 1.45 | – |
| Asian American/Pacific Islander | 0.87 | 0.33, 1.91 | – |
| American Indiane | 0.60 | 0.30, 3.97 | – |
| Other/unknowne | 0.63 | 0.07, 3.50 | – |
| Central nervous stratified by race/ethnicityd | 0.08 | ||
| White | 0.78 | 0.47, 1.22 | – |
| Black | 1.41 | 0.98, 2.00 | – |
| Hispanic | 1.17 | 0.66, 1.96 | – |
| Asian American/Pacific Islander | 1.00 | 0.68, 1.28 | – |
| American Indiane | – | – | – |
| Other/unknowne | – | – | – |
| External stratified by race/ethnicityd | 0.02 | ||
| White | 1.01 | 0.56, 1.69 | – |
| Black | 0.97 | 0.59, 1.53 | – |
| Hispanic | 1.44 | 0.77, 2.55 | – |
| Asian American/Pacific Islandere | – | – | – |
| American Indiane | – | – | – |
| Other/unknowne | – | – | – |
- a All models are adjusted for age, race/ethnicity, prenatal care, diabetes status, smoking status, and area level education unless stratified by that variable.
- b Likelihood ratio test p value comparing nested models with and without an interaction term for the potential modifier.
- c Includes both gestational and non-gestational diabetes;
- d Self-classified from birth record.
- e These strata have fewer than 500 observations and may not produce reliable estimates or instances of no observations and no estimates.
We did observe evidence of effect measure modification by race/ethnicity for central nervous and external defects, (LRT p value = 0.08 and 0.02, respectively). Stratified estimates indicated the potential for modification (higher magnitude ORs for Black and Hispanic gestational parents compared to White gestational parents but imprecision due to small samples may contribute to inconclusive evidence). We also observed evidence of effect measure modification for diabetes status with cardiovascular defects only (LRT p value = 0.08) with gestational parents with diabetes having increased odds of any birth defect and considerable differences in stratum-specific estimates when looking among specific groups and some individual defects (e.g., atrial septal defect and hydrocephalus; Table 2, Figures 3, S1.1 and S1.2). Sensitivity analyses to examine the robustness of results to possible misclassification of the diabetes covariate exhibited no changes in estimates when excluding adjustment for diabetes in defect group models or when excluding 2010 data. Changes to the odds ratios did occur when subsetting the data to the years 2003–2009 and 2011–2015 for cardiovascular and external defect groups (Table S1.3). Our adjusted results differed slightly from crude (unadjusted) models with only minor changes to point estimates and confidence intervals (Table S1.4) Altering our exposure threshold did reveal a slight exposure-response relationship with some stronger associations for a closer proximity, especially central nervous defects and the 1500-m threshold. Results also seemed attenuated by expanding further out to the 6000-m threshold, but model specification showed reasonable fit for the binary fit at 3000 m (Table 3 and Figure S1).
| OR | 95% CI | |
|---|---|---|
| 1500-m threshold | ||
| Cardiovascular | 1.16 | 1.01, 1.33 |
| Central Nervous | 1.29 | 0.92, 1.76 |
| External | 1.14 | 0.73, 1.70 |
| 3000-m thresholda | ||
| Cardiovascular | 1.15 | 1.04, 1.26 |
| Central Nervous | 1.16 | 0.91, 1.47 |
| External | 1.19 | 0.88, 1.59 |
| 6000-m threshold | ||
| Cardiovascular | 1.04 | 0.96, 1.13 |
| Central Nervous | 1.12 | 0.91, 1.37 |
| External | 1.08 | 0.84, 1.39 |
- a 3000 m is the principal threshold for all other presented results.
4 DISCUSSION
The primary aim of this analysis was to build upon prior study and investigate associations between residential proximity to lead (Pb) brownfields and birth defects. Using the data available from the NC Birth Defects Monitoring Program, CIMC, and NC-DEQ, we were able to assess residential exposure to Pb brownfields across many different birth defect phenotypes. We observed positive associations for cardiovascular defects and suggestive positive associations for central nervous and external defect groups, which had fewer cases and wider confidence intervals. Results from analyses for effect measure modification indicated probable modification by diabetes and evidence for modification by race/ethnicity for some defect groups. Diabetes and race/ethnicity are noted in prior literature as important covariates for birth defects (Correa et al., 2008; Laine et al., 2015; Ohlson, 2020; Sanders et al., 2014).
Our results indicate that residential proximity to Pb brownfields may be linked to birth defects, which is in line with a previous analysis looking at any brownfield exposure (Slawsky et al., 2022). These results are also consistent with a previous analysis looking at brownfields just within Charlotte, North Carolina and other birth outcomes (Wang, 2011). We are not aware of any other studies assessing Pb brownfields and birth defects, but several contaminants, including Pb, have been previously linked to various birth defects (Rappazzo et al., 2019; Sanders et al., 2014; Vinceti et al., 2001). Pb brownfields may represent a source for exposure and so residential proximity to Pb brownfields may interrupt, or otherwise harm, fetal development. The most plausible route for exposure would be from leached Pb into the soils and waters surrounding the brownfield site. Prior studies provide evidence of well water contamination in North Carolina from Pb and other heavy metals (Eaves et al., 2022; Sanders et al., 2014). It is also possible that Pb dust could have infiltrated soils from remediated sites with recent study highlighting elevated Pb soil levels surrounding locations of former waste incinerators (Bihari, 2022). It is therefore plausible that Pb exposure could occur for gestational parents through soil, water, and air, and so through dermal absorption, ingestion, or inhalation routes and may be dependent on the former function of the brownfield site. It is also possible that brownfields may be proxy measures for neighborhood and environmental quality even in the absence of direct contamination and impact birth outcomes through psychosocial stress (Carmichael et al., 2007; Landrigan et al., 2010). The findings of this analysis limited to Pb brownfields are somewhat stronger (i.e., higher magnitude indicated in the odds ratio) than those from the previous analysis looking at any brownfield and support the need to investigate other contaminant-specific brownfields (e.g., cadmium, mercury, and volatile organic compounds) (Slawsky et al., 2022).
Using a widespread cross-sectional approach allowed us to capture rare phenotypes from a large birth records dataset that included thousands of cases across North Carolina in a population representative for the state. Analysis of potential effect measure modifiers identified potential groups most acutely impacted such as those with diabetes and minoritized races. These individuals may be more susceptible, vulnerable, or disproportionately exposed to the impacts of nearby brownfields and further investigation of these groups would be informative. The maximum distance restriction of 10 km was used to ensure study participants had probable exposure to and regular contact with a Pb brownfield and meant our analytic sample was essentially of residences located in urban and suburban settings and had very few residences in rural settings. Pb brownfields also tended to concentrate near major urban centers. Sensitivity results altering the exposure threshold showed evidence of a modest exposure-response relationship. In further sensitivity analysis our results appear robust to changes in the diabetes variable for North Carolina birth records. Models for defect groups without adjustment for diabetes and with 2010 data removed did not result in changed estimates. Subsetting the data to smaller datasets before and after 2010 did alter estimates for cardiovascular and external defect groups, but it is not clear that these changes are due entirely to the diabetes variable or due to other aspects that vary between these sections of time.
Our study has some limitations. By using residential proximity, we are assuming that the individual had some exposure to the nearby brownfields, but this cannot be confirmed without more information on individual time-activity patterns; lacking this information may increase the risk of exposure misclassification. We were limited to the residential address at date of birth and did not have information on residential mobility that may have occurred during pregnancy. The critical exposure window for birth defects is early in the gestational period; if parents moved away from or closer to a Pb brownfield later in gestation, exposure misclassification could occur and introduce bias into our results. We anticipate this bias would be non-differential because it is unlikely that birth defect status would be known or would influence changing residences either toward or away from a Pb brownfield. We would expect potential sources of exposure misclassification to be non-differential with respect to case status and so likely bias estimates toward the null. We are also limited by not having a quantifiable amount of Pb contamination and so cannot confirm that Pb is the primary contaminant at a given brownfield only that a site had measurable amounts of Pb. This opens a potential for exposure measurement error and confounding by co-contaminants. We still expect exposure measurement and unmeasured confounding to be non-differential to case status. An additional concern is the binary classification of exposure creating a false dichotomy at the 3 km point. Sensitivity analyses examining different cut points did indicate a potential exposure-response relationship with slightly stronger associations for those 1500 m or closer and weaker associations when the threshold was placed at 6000 m (Table 3). Analysis of model specification also did support adequate fit for binary specification of exposure (Figure S1). Measurement error for the outcomes is likely to be minimal, although misdiagnosis is possible. Selection bias should not be a concern because NCBDMP actively screens all birth records, but errors or missing records could occur. Being a cross-sectional design, temporality would ordinarily be a concern. However, because brownfields are often legacy contaminant sites they have been present in the community for decades or even centuries and are likely present throughout the entire gestational length of births from this 2003–2015 timeframe. Additionally, efforts to successfully remediate these sites are recent, and grants have been awarded at an increasing pace to identify and begin remediation on a growing number of sites (Berman et al., 2022). Therefore, it is possible that our list of sites from 2020 may be an underestimate of actual brownfield sites.
There are limitations to the birth records data themselves as administrative changes to questionnaire items, for example diabetes, changed around 2010 and there are concerns that those variables may not be reliable or comparable. Our sensitivity analyses partially ameliorate these concerns with little to no change in estimates with or without diabetes adjustment or restriction of data. Sub-setting the data before and after 2010 did differ, but it is not clear that the diabetes variable is driving this change or if reductions in sample size or other time-related factors (e.g., air pollution trends, medication availability, etc.) played a role. Critically none of the estimates disagree directionally with all models, still indicating a positive association via point estimates (Table S1.3) Future studies may want to examine brownfields assessed for specific former functions (e.g., former gas station) to better understand possible mechanisms and link more closely to neighborhood composition. Prior literature provides evidence that well water users are exposed to increased levels of Pb and that some North Carolina wells have detectable levels of Pb and other heavy metals (Eaves et al., 2022; Gibson et al., 2020). It is possible that lead from brownfields could leach into groundwater, providing indirect exposures of lead to North Carolinians. However, this would require site/well specific testing to confirm, which is beyond the scope of this article. We lacked spatially resolved water source data and so could not assess the impacts of water source type. Misestimation (over or under) may occur due to missing important covariate adjustment like water source type, and risk of residual and uncontrolled confounding remains. We also lacked data to assess actual blood and brownfield site Pb levels and so participants from this analysis may not have had any Pb exposure or could possibly be exposed occupationally to Pb or via some other means, opening the potential for non-differential exposure misclassification that could bias our results toward the null in expectation. It should also be noted that brownfields themselves may be proxies for other causative factors. Residential proximity to a brownfield may be indicative of lower socioeconomic status or additional environmental justice concerns that may impact birth defects. Further research will be useful to parse out the specific impacts of brownfields on birth defects adjusting for covariables tailored to specific birth defect phenotypes or groups where sample sizes allow. These steps may continue to elucidate the impact brownfields have on birth defects.
5 CONCLUSIONS
This analysis of residential lead (Pb) brownfield exposure and the prevalence of cardiovascular, central nervous, and external defects found that proximity to a Pb brownfield may increase the risk for various birth defects, especially cardiovascular defects. Pb brownfields may pose a further risk to certain groups like those with diabetes and minoritized races. Further research is needed to better understand the role of former site function, the relationships brownfields have with neighborhood quality, redlining, and environmental justice concerns linked to brownfields and legacy contamination.
ACKNOWLEDGMENT
The authors would like to acknowledge Corinna Keeler and Stephanie DeFlorio-Barker for their review and comments, Debora Andrews for quality assurance review, and Nina Forestieri for original data collection and collaboration.
FUNDING INFORMATION
This research was supported, in part, by an appointment to the Research Participation Program for the US Environmental Protection Agency, Office of Research and Development, administered by the Oak Ridge Associated Universities through an interagency agreement between the US Department of Energy and Environmental Protection Agency. This study was performed as part of normal duties by EPA employees and contractors. Further support was provided by the National Institute for Occupational Safety and Health training grant (NIOSH T42OH008673). The funders had no role in the study design, data collection, analysis, interpretation, or manuscript writing.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interest.
DISCLAIMER
The views expressed in this article are those of the author(s) and do not necessarily represent the views or policies of the U.S. Environmental Protection Agency. Mention of trade names or commercial products does not constitute endorsement or recommendation for use.
Open Research
DATA AVAILABILITY STATEMENT
Some data that support the findings of this study are available for public download. Data from the NC Birth Records are not publicly available; contact Nina Forestieri for inquiries https://schs.dph.ncdhhs.gov/units/bdmp/contacts.htm https://deq.nc.gov/about/divisions/waste-management/brownfields-program; https://www.epa.gov/cleanups/cleanups-my-community; https://schs.dph.ncdhhs.gov/units/bdmp/; https://www.census.gov/programs-surveys/decennial-census/decade.2010.html https://www.census.gov/programs-surveys/acs/technical-documentation/table-and-geography-changes/2017/5-year.html Code files used for this analysis are available upon request.




