Antigenic targets and pathogenicity of anti–aortic endothelial cell antibodies in Takayasu arteritis
Abstract
Objective
Anti–endothelial cell antibodies are considered to have an important role in the pathogenesis of Takayasu arteritis (TA). Previously, these antibodies were detected using human umbilical vein endothelial cells, which do not completely represent the antigenicity/functions of aortic endothelial cells, the specific targets in TA. To delineate the precise role of antigenic targets, we investigated such targets as well as the pathogenic mechanism of antibodies directed against aortic endothelial cells (AAECAs) in TA.
Methods
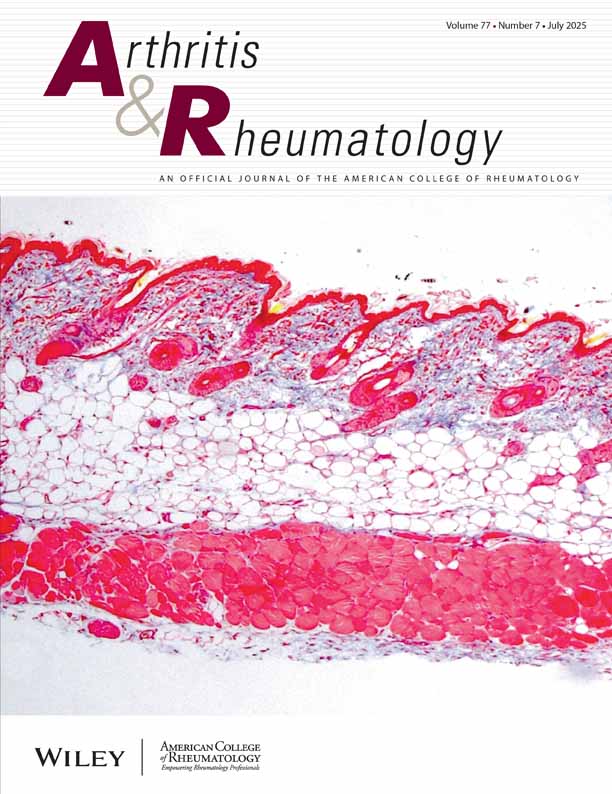
AAECAs were detected using a cellular enzyme-linked immunosorbent assay (ELISA), and their antigenic targets were detected by immunoblotting. AAECA-mediated induction of endothelial adhesion molecule expression and cytokine production was studied by ELISA, and apoptosis was studied using the TUNEL method.
Results
AAECAs were detected in 86% of patients with TA and in 9% of controls. Sera obtained from AAECA-positive patients with TA recognized a total of 9 antigens ranging in size from 18 kd to 200 kd, of which the 60–65-kd triplet was recognized most often. The aortic endothelial cell reactivity of Hsp60-absorbed sera was reduced by ∼50% as compared with that of unabsorbed sera (mean ± SD 0.488 ± 0.08 versus 0.838 ± 0.116). Sera from AAECA-positive patients with TA, compared with sera from AAECA-negative patients with TA and that from controls, induced increased expression of E-selectin (mean ± SD 0.833 ± 0.063 versus 0.217 ± 0.081 and 0.221 ± 0.101 optical density [OD] units, respectively) and vascular cell adhesion molecule 1 (0.620 ± 0.144 versus 0.165 ± 0.005 and 0.177 ± 0.055 OD units, respectively) and increased production of interleukin-4 (IL-4) (6.8 ± 2.4 versus 1.2 ± 1.6 and 1.3 ± 2.5 pg/ml, respectively), IL-6 (24.3 ± 2.4 versus 4.5 ± 6.7 and 5.9 ± 5.1 pg/ml, respectively), and IL-8 (36.8 ± 10.3 versus 10.1 ± 6.7 and 7.8 ± 2.1 pg/ml, respectively). Sera from AAECA-positive patients with TA induced 29 ± 6% (median ± SEM) apoptosis of aortic endothelial cells.
Conclusion
Our data show that the AAECAs that are present in patients with TA are directed mainly against 60–65-kd antigen(s) and may cause vascular dysfunction by inducing expression of endothelial adhesion molecules, cytokine production, and apoptosis.