Challenges for interprofessional simulation-based sedation training courses: Mini review
Abstract
Sedation for invasive procedures is given for various clinical purposes to patients of all ages worldwide. However, sedation is a continuum to general anesthesia and contains severe inherent risks leading to mortality. Providing a simulation-based sedation training course (SEDTC) to various medical staff could be an effective strategy to improve patient and medical safety associated with sedation. The SEDTC generally includes basic airway management such as upper airway obstruction release or rapid response action toward excessive sedation, utilizing problem-based learning or simulators. However, participation alone in the SEDTC can only achieve Level 1 (reaction) or 2 (learning) in the Kirkpatrick model. A patient safety improvement of Level 3 (transfer) or 4 (result) of the Kirkpatrick model can be achieved when all members related to sedation undergo experiential learning and reach a consensus. Accordingly, in-hospital interprofessional SEDTC focusing on a resilience approach is essential to achieve effective sedation patient safety in Level 3 or 4 of the Kirkpatrick model.
SEDATION FOR INVASIVE PROCEDURES AND CONCERNS REGARDING PATIENT SAFETY IMPROVEMENT
The main purpose of sedation for invasive procedures is the application of sedative or analgesic drugs to diminish anxiety and attenuate pain to provide an appropriate degree of amnesia or decreased awareness. Another important purpose of sedation for invasive procedures is to minimize patient motion, to allow doctors to perform necessary diagnostic or therapeutic procedures.1
Sedation for invasive procedures is different from monitored anesthesia care, which must be provided by anesthesiologists. In contrast, sedation for invasive procedures can be provided not only by anesthesiologists but also by nonanesthesiologists.2, 3
Sedation for invasive procedures is given for various clinical purposes to patients of all ages worldwide.4 However, sedation is a continuum to general anesthesia and contains severe inherent risks leading to mortality, and it is not always possible to predict how an individual patient will respond.5, 6
One report on closed claims showed that the most common adverse effect or injury during procedural sedation is respiratory depression due to over-sedation.7
PROCEDURAL SEDATION GUIDELINES FOR NONANESTHESIOLOGISTS
While doctors try to target depth of sedation, the actual level of sedation can unexpectedly fluctuate and sometime collapse, because the metabolism or response to drugs differs individual by individual. In 1996, the Practice Guidelines for Sedation and Analgesia by Non-Anesthesiologists (ASA-SED) was reported by the American Society of Anesthesiologists. The ASA-SED were updated in 2002 and 2018.9, 10 This guideline strongly recommends that patient monitoring should be performed continuously by medical staff who are not directly involved in the procedure.8 The ASA-SED provides recommendations and warnings for nonanesthesiologists to provide safe sedation and analgesia. Moreover, they define and emphasize that sedation is a continued general anesthesia. Thus, high-quality and safe sedation necessitates preoperative patient examination especially on airways, sufficient fasting time set-up, appropriate monitoring including verbal response to patient, adequate emergency equipment, compliance with drug administration principles, and validation of discharge criteria. In addition, all medical staff related to procedural sedation should always be aware that the level of sedation changes according to the circumstances.
SIMULATION-BASED SEDATION TRAINING APPLICATION FOR PATIENT SAFETY IMPROVEMENT
Nontechnical skill is usually regarded as an essential component of patient or medical safety management, including sedation.11 Deficiencies in nontechnical skills can increase the error risk, leading to adverse events or outcomes.12 One effective method for patient or medical safety improvement is simulation-based education (SBE). Simulation-based education has been shown to be a valuable and effective instructional tool for both technical and nontechnical skills, as well as behavior-based crisis management skills.12 For example, SBE can contribute to rapid response system education on excessive sedation as this educational method could be used to acquire excessive sedation-related technical or nontechnical skills.13
The primary risk associated with excessive sedation is respiratory suppression or airway obstruction, which frequently leads to hypoxia. The first step in the rapid response when responding to excessive sedation is to notice hypoventilation leading to hypoxia through patient observation or technical monitoring. The next action for medical staff in the clinical situation is to activate the rapid response system (call for help), give high-flow oxygen to sedated patients, and perform airway management to release the upper airway obstruction utilizing manual airway maneuvers or sometimes assist using bag-valve-mask ventilation.14 Furthermore, antagonist administration may treat respiratory suppression if some opioids or benzodiazepines are administered. Thus, nontechnical skill development is warranted.
As analgesic and sedative doses and matching differ by each invasive procedure or institution, SBE on sedation safety for invasive procedures should include not only situational awareness but also effective communication to team members, including rescuers, regarding administered drugs.
- Constructing a patient or medical safety system that includes basic monitoring to recognize emergency respiratory suppression and activation of the rapid response system.
- Establishing the rapid access to airway rescue devices for release of airway obstruction or respiratory suppression.
- Establishing the rapid response system to respiratory suppression by excessive sedation.
- Installing the “excessive sedation” specific rescue box in each department. The rescue box should contain conventional resuscitation drugs, airway rescue devices (orotracheal or nasotracheal airway, supraglottic device, and so on), and antagonists (flumazenil or naloxone).
- Establishing postsedation monitoring obligations and determine the standards for discharge.15, 16
Off-the-job training utilizing SBE training applications can enhance the patient or medical safety to diminish sedation-related complications.17
CURRENT LIMITATIONS OF SEDTC IN JAPAN
There are various reports of SEDTCs for procedural sedation safety focusing on the rapid response system to excessive sedation and its prevention.18, 19 These training courses are mainly developed by critical care doctors, such as anesthesiologists or emergency doctors, which suggests that critical care doctors who are familiar with respiratory or circulation crisis management play an essential role in safety sedation risk management systems.20 From the viewpoint of patients or medical safety, participants of SEDTC are expected to acquire competency on: (1) appropriate sedation preparation, (2) emergency rapid response to drug-induced hypoxia, and (3) effective team communication skills.21, 22
One problem associated with the present SEDTC in Japan is the adaptability to each sedation situation. As procedural sedation is performed in various medical environments, such as emergency departments or endoscopy rooms, it is sometimes difficult for the participants to apply the competency to their own medical environments. To overcome this problem, in-hospital SEDTC can be one possible solution. Another nonnegligible problem associated with current SEDTC is the lack of team resilience. Individual medical staff such as doctor or nurse participation in public SEDTC courses cannot cultivate team resilience. For the improvement of safety management of sedation, not only interprofessional knowledge sharing on sedation or rescue techniques but also reconstruct the system of sedation. For example, all medical staff related to procedural sedation are expected to acquire sufficient sedation principles and safety management understanding. Thus, further interprofessional approaches, including resilience, are warranted for SEDTC in Japan.
NEED FOR INCORPORATING RESILIENCE COMPETENCIES IN SEDTC
Rapid response training has been developed to be an evidence-based method to ensure patient and medical safety to enhance clinical outcomes.23 Although rapid response team performance is not uniform in each department, rapid response training in SEDTC should emphasize sedation-related emergency and treatments. For including emergency response team competency in SEDTC, we should focus attention on the resilience of individual team members.24, 25
A recent report showed that staff resilience plays an essential role in the development of overall patient safety.26 As resilience of medical staffs can facilitate improvements in interprofessional teamwork, applications, safety climate development plays a central role in effective rapid response team function.27, 28 While individual teamworking skills and competencies, SBE can be an effective method to develop resilience in various medical teams. Resilience training requires instruction that is developed for organizational and individual procedures or department characteristics that are unique to the emergency response team context. These characteristics can be applied to SEDTC because the training mainly focuses on the rapid response system to excessive sedation. A wide variety of settings, including magnetic resonance imaging rooms, emergency departments, endoscopy rooms, and operating rooms represent unique situations that require customized team training solutions incorporating individualized resilience components.
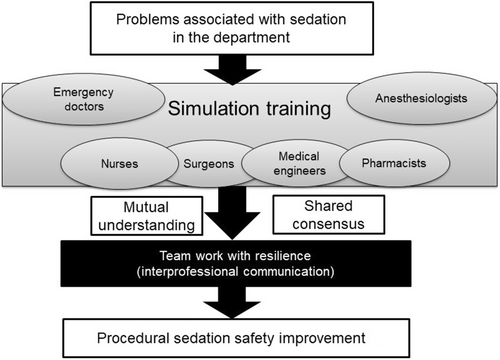
One expected competency associated with sedation for invasive procedures can be derived from SBE that incorporates airway rescue techniques and nontechnical skills such as communication or situational awareness. Another important sedation team competence is team resilience that supports effective approaches to medical emergencies associated with sedation-related complications. Rapid response teams to excessive sedation are required to be adaptable and individuals must be resilient. Accordingly, SBE can provide the requisite training in team adaptability and individual team member resilience during responses to medical emergencies associated with sedation (Figure 1). As team member resilience should be developed in each sedation department, in-hospital type SEDTC application is warranted. I believe that in-hospital SEDTC that includes resilience as an explicit teamwork training objective can enhance mutual understanding or shared consensus, leading to overall team performance associated with procedural sedation.
POSSIBILITY OF INTERPROFESSIONAL IN-HOSPITAL OFF THE JOB TRAINING FOR IMPROVING PROCEDURAL SEDATION SAFETY
The Kirkpatrick model has been applied over the decades as the major framework for evaluating education or training outcomes. Various evidence regarding the efficacy of various methods in professional health-care training has been accumulated on the utility of the Kirkpatrick model.28 Increased medical staff competency in the patient or medical safety domain has been demonstrated following conventional SBE courses.
However, the outcomes measured after conventional SBE courses have been largely limited to Kirkpatrick Level 1 (reaction) and 2 (learning) measures. While knowledge, skills, and attitudes regarding patient or medical safety should be “seeded” within organizations by key team members who participate in patient safety training incorporating SBE, the majority of individuals in the hospital who did not undertake SEDTC are not aware of patient safety related to sedation. Thus, individual training, while necessary, is insufficient to elicit remarkable changes in outcomes by the entire professional health-care workforce. In other words, participation in the SEDTC as an individual can only achieve Level 1 or 2 in the Kirkpatrick model. To develop significant improvement leading to patient or medical safety system outcomes, entire dissemination and adoption of attitudes and skills throughout the entire workforce is essential.
Patient safety improvement reaching Levels 3 or 4 of the Kirkpatrick model can be achieved when all members relating to sedation undergo experiential learning and reach a consensus associated with team resilience. Similarly, achieving Kirkpatrick Level 4 (Figure 2) through the patient or medical safety educational program requires interprofessional consensus and subsequent actions. The in-hospital interprofessional scenario-based SBE utilizing problem-based learning and discussion or simulators for sedation safety for invasive procedures can support smooth consensus building, leading to team resilience.
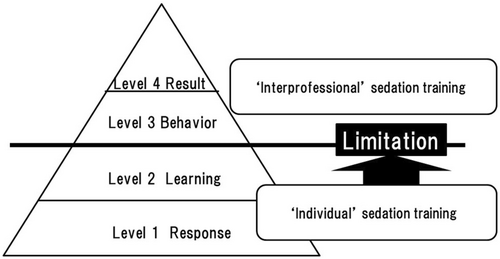
Development of skilled facilitators for patient safety SBE within individual hospitals is urgently required to realize and measure effective outcomes of in-hospital patient safety programs. In other words, to achieve Level 3 or 4 of the Kirkpatrick model in each clinical sedation environment, in-hospital interprofessional SEDTC is needed (Figure 2). The updated 2018 ASA-SED recommends that patient or medical safety improvement action associated with procedure sedation should be performed by all teams in the hospital. This idea is consistent with the idea that in-hospital interprofessional SBE can facilitate resilience and patient or patient safety improvements associated with procedural sedation.
Certainly, there are several barriers for introducing in-hospital SEDTC. First, it is sometimes difficult to keep training times and adjust interprofessional schedules for SBE. The support and understanding of the stakeholders are essential. Second, training scenario should be developed that are appropriate to the sedation environment. The SBE specialist and medical safety trainer should collaborate to establish the training scenario. Finally, it is sometime difficult for various medical staff to cultivate the motivation for improving sedation safety. Continuous sedation medical safety emphasis is warranted.
The learning purpose should be decided based on common interprofessional problems associated with sedation. Utilizing in-hospital simulation, department medical staff can discuss the problem and arrange to obtain technical and nontechnical skills on prevention or rapid response when dealing with excessive sedation. Critical care doctors such as anesthesiologists or emergency physicians play a vital role in facilitating these in-hospital SEDTCs. Critical care doctors should also participate in the course to demonstrate appropriate rapid response techniques and protocols. Continuous in-hospital SEDTC can develop attitudes in various medical professionals associated with SEDTC little by little but steadily.
After completing the in-hospital SEDTC, a mutual understanding and shared consensus among staff can help to develop team resilience toward procedural sedation in the department. Continuous effort and study on the effects of such in-hospital patient safety system improvement is warranted in the future.
CONCLUSION
Several SEDTC programs have been developed by critical care doctors for patients and patient safety improvement. To overcome the limitations of present SEDTCs, in-hospital interprofessional off-the-job training focusing on resilience is required for practical safety improvement in each procedural sedation environment.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: N/A.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
There is no data.