Traumatic intrapericardial diaphragmatic hernia
Graphical Abstract
Traumatic intrapericardial diaphragmatic hernias are very rare; they occur when the central tendon of the diaphragm ruptures, allowing abdominal viscera to herniate into the pericardial sac, causing life-threatening cardiac tamponade. Computed tomography imaging with multiplanar reconstruction is useful in evaluating such cases.
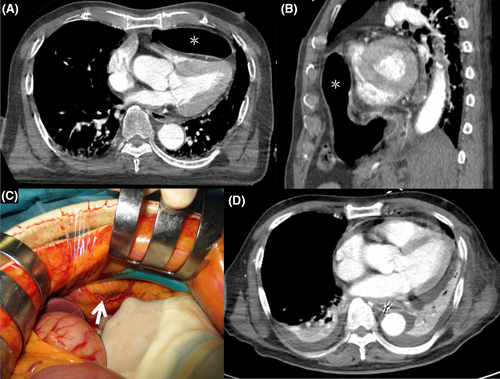
An 89-year-old man presented to the emergency department following a motorcycle accident; his vitals indicated shock and respiratory distress. Echocardiography showed deformation and compression of the cardiac chambers; however, the images were unclear. A contrast-enhanced computed tomography (CT) performed 15 min after patient transfer revealed multiple injuries, including gastric herniation through an anterior diaphragmatic defect into the pericardial sac (Figure 1A,B), with compression of the right ventricle (asterisk), left renal artery injury, retroperitoneal hemorrhage, and pelvic fracture. Hypotension persisted despite fluid resuscitation. Blood transfusions and intravenous norepinephrine were initiated, and the patient's hemodynamics stabilized at the start of surgery. An emergency laparotomy performed 3 h after CT image acquisition revealed a 5 cm diaphragmatic defect (white arrow) (Figure 1C). The hernia had improved spontaneously and was not identified at the time of surgery. Intraoperative findings showed no injury to the stomach or heart, except in the area of the pericardial injury, which had become a hernia defect. The defect was repaired with interrupted 2-0 prolene sutures in the diaphragm and pericardium. No drain was placed in the pericardial sac. Left nephrectomy and external fixation of the pelvis were then carried out. A total of 5360 mL of blood was transfused, and the patient was admitted to the intensive care unit after 9 h of surgery. Three days after admission, CT revealed no hernia recurrence (Figure 1D). Intensive care was continued; however, the patient died on day 16 from multiple-organ failure due to sepsis.
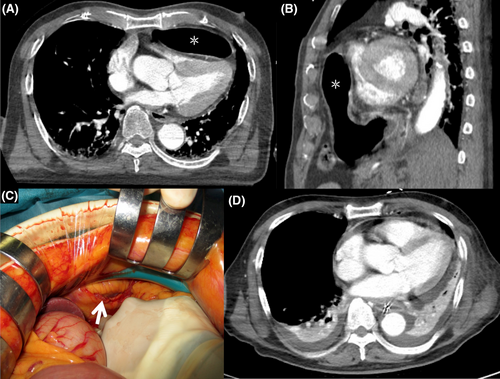
Traumatic diaphragmatic hernia accounts for 3%–7% of all abdominal and thoracic trauma and rupture of the diaphragm. They occur in the left posterolateral aspect due to the protective ability of the liver to absorb energy on the right.1, 2 However, traumatic intrapericardial diaphragmatic hernias are very rare; they occur when the central tendon of the diaphragm ruptures, allowing abdominal viscera to herniate into the pericardial sac, causing life-threatening cardiac tamponade.1 Although cardiac tamponade is clinically diagnosed, imaging studies are crucial in its assessment. Chest radiographs of patients with cardiac tamponade could demonstrate an enlarged cardiac silhouette, suggesting pericardial effusion. However, chest radiographs might not be useful for early diagnosis, as pericardial effusion <200 mL is not visible on radiographs.3 Cases of traumatic acute cardiac tamponade with a normal-sized heart on chest radiographs have further been reported.3 Echocardiographic findings, such as pericardial effusion and cardiac chamber compression, can be diagnostic of cardiac tamponade. However, transthoracic echocardiography can be difficult to carry out, with inadequate views obtained in 13%–38% of trauma patients.4 In traumatic diaphragmatic hernias, hernias of various organs have been reported, including the transverse colon, stomach, and greater omentum1; it is difficult to assess these findings by chest radiography or echocardiography accurately. Therefore, if the primary survey shows that the physical and echocardiographic findings are suspicious for cardiac tamponade, but the structures of the intrapericardial space are unclear, and pericardiocentesis is not possible, a surgical pericardial window should be performed. Alternatively, if the institution is equipped to handle sudden changes or unstable situations, a CT scan should be performed promptly. Computed tomography with multiplanar reconstruction can accurately diagnose the cause of cardiac tamponade and identify rare but potentially fatal injuries,5 while assessing other trauma findings, as in this case. In this case, the long operative time could have contributed to the patient's death. Based on the concept of damage control surgery, a shorter operative time and adequate intensive care are critical in the management of severe trauma patients.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
Authors declare no conflict of interests for this article.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: The requirement for patient consent was waived due to the anonymous nature of the information.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.