Uterine rupture successfully treated with a damage-control strategy of hysterectomy and resuscitative endovascular balloon occlusion of the aorta-assisted cardiopulmonary resuscitation
Abstract
Background
Uterine rupture is a major cause of postpartum hemorrhage (PPH) that requires surgery. Resuscitative endovascular balloon occlusion of the aorta (REBOA) is also helpful for PPH. However, the effectiveness of REBOA in PPH with cardiac arrest is unknown.
Case Presentation
A 40-year-old woman developed hemorrhagic shock due to uterine rupture after an induced delivery. She developed cardiac arrest, but was rescued by cardiopulmonary resuscitation (CPR), REBOA, a hysterectomy, and pelvic gauze packing. The hemodynamics were too unstable to move to the operating room. Then we initiated the CPR assisted with REBOA and decided to activate massive transfusion and perform laparotomy in the emergency room. She was finally discharged home without neurological sequelae.
Conclusion
Our damage control strategy, including REBOA-assisted CPR, contributed to saving the life of a patient with a life-threatening PPH.
INTRODUCTION
Postpartum hemorrhage (PPH) can be fatal to both the mother and fetus, and is a major cause of maternal death worldwide.1 Patients with PPH often present with disseminated intravascular coagulopathy, which could necessitate a damage control strategy such as open abdominal management.2, 3
Uterine rupture is a major cause of PPH that requires surgery.4 Resuscitation, hemostasis, and correction of coagulopathy must be achieved quickly if a uterine rupture patient develops cardiac arrest.
Resuscitative endovascular balloon occlusion of the aorta (REBOA) uses an intra-aortic balloon catheter to control distal arterial bleeding and increase proximal blood pressure (BP) in cases of hemorrhagic shock due to a subdiaphragmatic injury. Resuscitative endovascular balloon occlusion of the aorta is also helpful in PPH.5 However, resuscitative thoracotomy (RT) may be preferable to REBOA in cases of traumatic cardiac arrest because of its speed and reliability.6 The effects of REBOA on neurological outcomes in cardiac arrest remain unknown.
We report a patient with postpartum uterine rupture who developed cardiac arrest. She was saved by applying a damage control strategy, including emergency hysterectomy during REBOA-assisted cardiopulmonary resuscitation (CPR).
CASE PRESENTATION
A 40-year-old woman delivered on the first day of her 39th week of pregnancy (gravida 5, para 1; vaginal delivery). Her medical history was noncontributory and she did not take any medications. Labor was induced with oxytocin and the Kristeller maneuver was used for delivery. Vaginal hemorrhage was 120 mL before the placenta was delivered and reached 1000 mL in the first hour. Her systolic BP dropped to 50 mmHg and did not respond to fundal massage, uterovaginal packing, and fluid administration. The physician at the outside hospital did not recognize the peritoneal hemorrhage. She was admitted to our hospital 150 min after delivery.
On admission, her BP was 76/46 mmHg, the heart rate was 133 b.p.m., the respiratory rate was 40 breaths/min, peripheral oxygen saturation was 97% (oxygen, 10 L/min), the consciousness level was E3V4M5 on the Glasgow Coma Scale (GCS), and body temperature was 35.1°C. Her abdomen was distended, but vaginal bleeding was minimal on pelvic examination. Abdominal ultrasonography revealed a massive peritoneal hemorrhage.
We intubated the patient immediately and gave her fluid and a massive transfusion. A 7F sheath was inserted through the left common femoral artery, and a REBOA catheter (Rescue Balloon ER; Tokai Medical Products) was placed and inflated above the diaphragm (Zone 1) (Figure 1). She suffered cardiac arrest and received CPR. The platelet count was below the detection threshold and the fibrinogen level was 40 mg/dL. We used active clotting factor VII to correct her coagulopathy. As the patient had repeated cardiac arrest and spontaneous circulation, the resuscitation team recognized that the hemodynamics were too unstable to move to the operation room. We initiated CPR assisted with REBOA and decided to activate massive transfusion and perform laparotomy in the emergency room after a multidisciplinary discussion. After the inflation of REBOA, we palpated a more definite pulse at the carotid artery and confirmed an increase in end-tidal carbon dioxide tension (EtCO2).
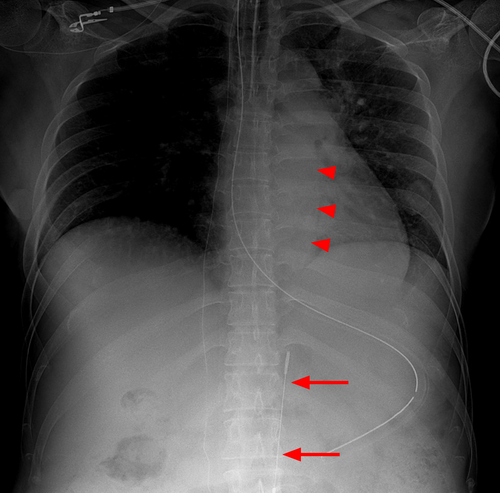
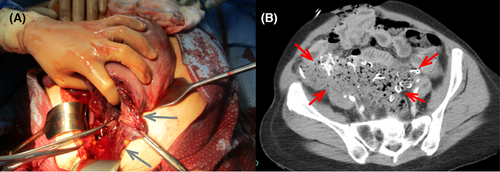
We observed a laceration of the uterus from the anterior wall to the right cervix (Figure 2A). A supravaginal hysterectomy was carried out for the uterine rupture with Zone 1 REBOA. Pelvic gauze packing was used due to sustained oozing (Figure 2B) and the patient was transferred to the intensive care unit for open abdomen management. After the hysterectomy, we deflated the REBOA gradually to explore further hemorrhage sites. Ideally, we wanted to deflate the REBOA following stable return of spontaneous circulation (ROSC). However, organ ischemia was a concern from prolonged aortic occlusion using REBOA located in Zone 1. Therefore, we deflated the REBOA before the stable ROSC. She received CPR for 44 min in total (Table 1, Figure S1). The pupillary findings changed during resuscitation; pupil diameters were bilaterally dilated to 7 mm but returned to 4 mm with prompt light reflex. The intraoperative blood loss was 6000 mL and 34 units of packed red blood cells, 42 units of fresh frozen plasma, and 40 units of platelets were transfused in the first 24 h.
| Time after admission (min) | Resuscitation and hemostasis | Vital signs |
|---|---|---|
| 0 | Arrival at hospital | BP 76/46 mmHg, HR 133 b.p.m. |
| 1 | Abdominal ultrasound | |
| 4 | Fluid resuscitation was started | |
| 8 | Intubation | |
| 17 | Transfusion was started | BP 89/51 mmHg, HR 106 b.p.m. |
| 31 | REBOA | BP increased from 104/61 mmHg to 210/100 mmHg following REBOA inflation, HR 94 b.p.m. |
| 32 | CPR was started | Cardiac arrest (PEA) HR 44 b.p.m. |
| 58 | Laparotomy was started | BP 157/75 mmHg |
| 77 | Hysterectomy was done | Cardiac arrest (PEA) |
| 78 | Pelvic gauze packing was started | BP 136/58 mmHg |
| 100 | Balloon of the REBOA catheter was deflated | BP 155/118 mmHg |
| 107 | Laparotomy was done | BP 86/34 mmHg |
| Open abdominal management | ||
| 117 | Sustained ROSC | BP 122/84 mmHg HR 100 b.p.m. |
| 168 | Transfer to ICU | BP 102/36 mmHg HR 104 b.p.m. |
- Abbreviations: BP, blood pressure; CPR, cardiopulmonary resuscitation; HR, heart rate; ICU, intensive care unit; PEA, pulseless electrical activity; REBOA, resuscitative endovascular balloon occlusion of the aorta; ROSC, return of spontaneous circulation.
We repacked the abdomen because of the patient's unstable hemodynamics and progressive anemia. Computed tomography angiography revealed extravasation in the right rectus abdominis muscle, so we embolized the right inferior epigastric artery with gelatin sponges (Figure S2). The gauze was removed the next day and the abdomen was closed.
Her GCS recovered to E4VTM6 on day 1 despite the prolonged CPR. Mechanical ventilation was required for 8 days to treat postoperative pneumonia. The d-dimer level increased to 14.9 μg/mL on day 6, so continuous intravenous heparin was administered. Computed tomography angiography and ultrasound revealed a thrombus in the right iliac and ovarian veins and inferior vena cava. Heparin was replaced with a direct oral anticoagulant and the thrombus gradually disappeared. On hospital day 39, she was discharged home without neurological sequelae.
DISCUSSION
The patient developed hemorrhagic shock due to uterine rupture, followed by cardiac arrest. In parallel with CPR, an emergency hysterectomy was initiated, with REBOA used to control the subdiaphragmatic hemorrhage.
Manual compression and angioembolization are ineffective for hemostasis cases of uterine rupture, which require surgery. Uterine rupture is rare without a previous cesarean section or uterine surgery. The use of uterine contractions and pressure on the uterine fundus are risk factors for uterine rupture.4, 7 Uterine rupture might not cause vaginal bleeding or abdominal pain;4 although a prompt diagnosis and hysterectomy are essential for saving the lives of patients with uterine rupture, the diagnosis of intra-abdominal bleeding is often delayed.
Resuscitative endovascular balloon occlusion of the aorta is useful in patients presenting with hemorrhagic shock due to torso trauma, and is less invasive than RT.6 Although having a risk of limb ischemia,8 REBOA is also feasible and effective for controlling life-threatening PPH.5 The advantages of REBOA compared to RT for the treatment of shock PPH are as follows: (1) arterial access can be secured before cardiac arrest, (2) the aortic occlusion level is adjustable from Zone 1 for impending cardiac arrest to Zone 3 for anatomically reasonable occlusion in PPH, (3) the occlusion intensity can be titrated from complete to partial REBOA, and (4) aortic occlusion without a newly added large chest wound and less risk of hypothermia. Although REBOA assisted CPR for PPH is a challenging strategy, REBOA maintained the proximal arterial pressure during CPR and helped control the arterial bleeding without manual aortic compression until hysterectomy was carried out in our patient.
Unlike blunt polytrauma patients with supradiaphragmatic injuries, the bleeding source in PPH is in the pelvic cavity, where REBOA can control exsanguination. As a less invasive measure, REBOA contributed to the return and maintenance of spontaneous circulation in our PPH patient, even after cardiac arrest. Resuscitative endovascular balloon occlusion of the aorta is expected to maintain the proximal arterial pressure during CPR. We confirmed a more definite carotid pulse and increased EtCO2. It was also supposed to help control arterial bleeding without manual aortic compression until a hysterectomy was carried out on our patient. Thus, the potential benefit of REBOA in cardiac arrest patients was reported in previously published works.9
CONCLUSION
We reported a hysterectomy with REBOA-assisted CPR in a uterine rupture patient. She was rescued using a damage control strategy that included REBOA, emergency hysterectomy, gauze packing, open abdominal management, massive transfusion, and angioembolization.
ACKNOWLEDGMENTS
We would like to thank Textcheck for the English language editing.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: Informed consent was obtained from the patient.
Registry and registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
Author elects to not share data.