A case report: Efficacy of thoracic MRA for ischemic stroke due to acute aortic dissection
Abstract
Background
Ischemic stroke requires prompt diagnosis and treatment but rarely results from acute aortic dissection. The administration of tissue-type plasminogen activator (t-PA) to such patients can lead to serious complications and potentially fatal outcomes. Here, we report a case in which thoracic magnetic resonance angiography (MRA) was useful for identifying cerebral infarction complicated by acute aortic dissection.
Case Presentation
A 60-year-old man presented with a sudden onset of left-sided hemiplegia, right-sided hemiparesis, and dysarthria. Noncontrast CT ruled out intracranial hemorrhage; however, aortic dissection was not detected. MRI showed reduced blood flow in the right middle cerebral artery, and t-PA administration was suspected to have caused ischemic stroke. However, thoracic MRA revealed dissection from the ascending aorta to the arch, which was diagnosed using contrast-enhanced CT.
Conclusion
Thoracic MRA is useful for diagnosing acute aortic dissection in patients with a stroke.
INTRODUCTION
Early diagnosis and timely administration of t-PA can improve neurological prognosis in patients with cerebral infarction.1 ADD is a severe condition in which the inner layer of the aorta tears, causing blood to infiltrate the aortic wall, potentially leading to complete dissection; it rarely causes stroke-like symptoms in patients. Administering tPA in patients with ADD can be fatal.2 The reported annual incidence of ADD ranges from 2.5 to 7.1 cases per 100,000 people.3 ADD accounts for approximately 0.3% of all strokes.4
Ruling out ADD is critical for stroke diagnosis. Noncontrast computed tomography (CT) of the head and chest, as well as head and neck magnetic resonance imaging/magnetic resonance angiography (MRI/MRA), are commonly used for the imaging evaluation of cerebral infarction. ADD diagnosis with noncontrast chest CT alone is challenging, and head and neck MRI/MRA may not detect ADD if the dissection cavity does not reach the internal carotid artery (ICA). Cerebral infarction in ADD may occur directly (via dissection extending to the brachiocephalic and left common carotid arteries5) or indirectly (via hypoperfusion due to hypotension from cardiac tamponade6), which can complicate the diagnosis. MRA was performed to evaluate access to endovascular treatment and to diagnose ADD involving the ascending aorta and aortic arch in patients with cerebral infarction. Here, we report a case of ADD diagnosed using thoracic MRA prior to t-PA. Appropriate measures were implemented for cerebral infarction in patients with ADD.
CASE PRESENTATION
The patient was a 60-year-old man with no significant medical history. On the day of symptom onset, the patient suddenly developed left hemiparesis and required emergency assistance. When the emergency crew arrived, the patient denied experiencing any chest or back pain. The patient was brought to the hospital with symptoms of left-sided paralysis and right convergent strabismus, suggesting acute stroke.
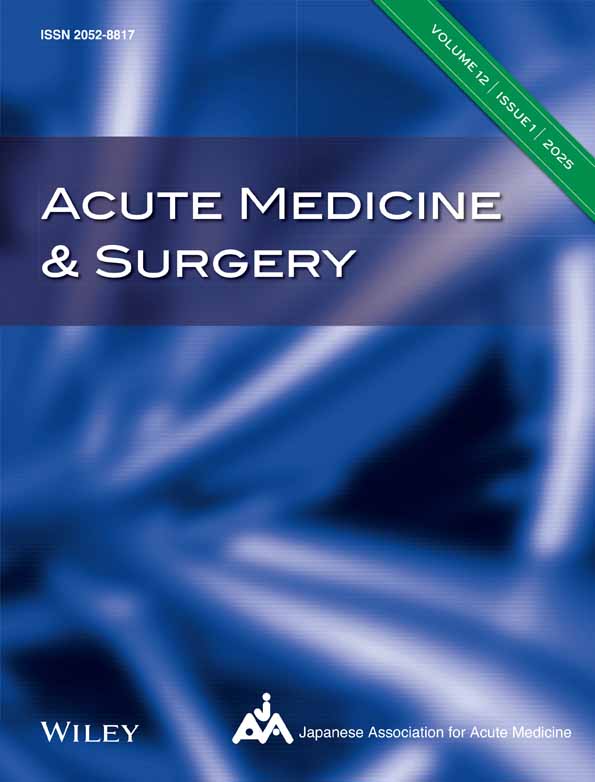
The patient's vital signs upon arrival were as follows: Glasgow Coma Scale (GCS), E3V4M6, SpO2: 95% (room air); respiratory rate, 16 breaths/min; blood pressure, 140/90 mmHg with no difference between the arms; pulse rate, 90 beats/min; and body temperature, 36.2°C. The National Institutes of Health Stroke Scale (NIHSS) score at the time of initial hospital care was 16/42. Ultrasonography revealed no issues in the carotid arteries or pericardium. A noncontrast CT scan was performed to evaluate an acute stroke. Head CT revealed no bleeding or organic issues, and chest CT revealed no signs of aortic dissection (Figure 1A–B). MRI showed no high-signal areas on diffusion-weighted images, and MRA revealed slightly decreased blood flow in the right middle cerebral artery (Figure 2A–C).
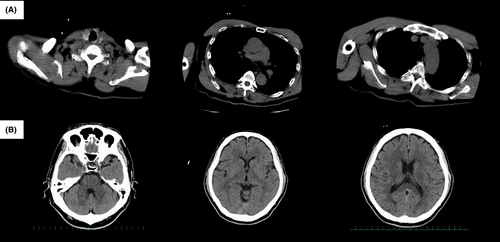
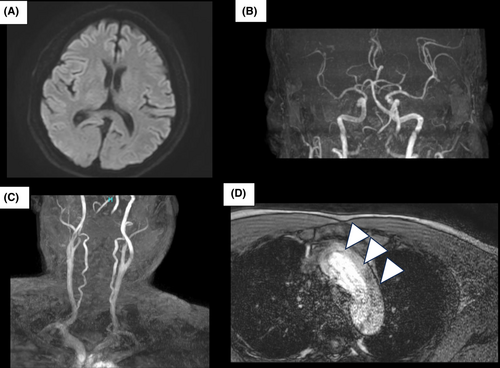
The patient had a presumed early-stage acute cerebral infarction that was undetectable on a head MRI. At the time of imaging and diagnosis—2 h after symptom onset and 30 min after hospital arrival—the administration of t-PA was considered. During a discussion with the neurosurgeon regarding thrombolytic therapy, blood tests revealed abnormal coagulation parameters, including fibrinogen levels of 72 mg/dL, FDP levels of 932.6 ng/mL, and D-dimer levels of 351.6 ng/mL. Consequently, the chest MRA was re-evaluated by the emergency physician and neurosurgeon, who identified a suspicious finding in the ascending aortic arch suggestive of a dissecting lumen (Figure 2D). To confirm the diagnosis, contrast-enhanced chest CT angiography was performed, which confirmed a Stanford type A aortic dissection extending from the ascending aorta to the common iliac arteries (Figure 3). At 3 h and 20 min after symptom onset, t-PA was withheld, and the patient was transferred to a specialized facility for surgical intervention. The patient underwent emergency surgery at the receiving facility, including replacement of the ascending aorta with an artificial graft. Postoperatively, his neurological symptoms gradually improved, with significant recovery of motor function. He was ambulatory with minimal assistance by the time of discharge and had a favorable functional outcome. He was discharged home on Day 16 of hospitalization with plans for outpatient follow-up and rehabilitation.
DISCUSSION
This case has two important implications. Although cerebral infarction usually requires prompt diagnosis and treatment, it can rarely be caused by ADD. Diagnosis is difficult when there is no chest pain or difference in blood pressure between the sides and there are few changes in the images of the internal carotid artery. Assessing ADD in cerebral infarction requires checking the head, neck, and chest MRA.
IV thrombolysis is vital for treating cerebral infarction1; however, it must be administered within 4.5 h and carries a risk of bleeding. Ischemic cerebrovascular disease complicated by ADD can lead to fatal hemorrhage. Therefore, it is imperative to rule out the presence of ADD.
Diagnosis of ADD is challenging when stroke is the initial presentation. The effects of ADD on stroke and imaging findings vary. Imaging tests alone have limitations in screening for ADD, owing to atypical clinical symptoms and low incidence.
Five mechanisms through which ADD can cause stroke have been proposed. (1) A mechanism in which the dissecting cavity extends into the common carotid or vertebral artery, obstructing blood flow to the brain. (2) The mechanism by which the dissecting cavity extends to the origin of the brachiocephalic, left common carotid, and left subclavian arteries obstructs blood flow. (3) Thromboembolism due to mural thrombi associated with dissection. (4) Hypoperfusion due to low blood pressure from cardiac tamponade. (5) Indirect ischemia due to compression of the true lumen by expansion of the false lumen.5, 6 In the present case, the dissecting lumen extended to the origin of the right brachiocephalic artery, corresponding to mechanism (2). Cervical MRI/MRA can readily diagnose cases involving mechanisms (1) and (2), where the dissection extends into the internal carotid and vertebral arteries. However, it should be noted that in this case, MRA did not clearly identify the dissection at the origin of the brachiocephalic artery, which made the diagnosis more challenging. Diagnosing cases involving secondary hypoperfusion, such as mechanisms (4) and (5), is presumed to be even more challenging because of the absence of apparent imaging changes in the head and neck region.
In particular, in cases of ADD presenting with neurological symptoms, approximately one-third of the patients do not complain of chest pain,6 and diagnosis is difficult because imaging tests for the purpose of evaluating stroke are prioritized in the initial treatment. In addition, although the difference in systolic blood pressure is associated with ADD, its sensitivity is only approximately 60%,7 and it is not always seen; therefore, it was not seen in this case either, and dissection could not be suspected.
In addition to imaging, there is an Aortic Dissection Risk Score (ADD-RS). The score is assigned to three categories: physical examination findings, pain symptoms, and patient background. The total score ranges from 0 to 3 points. It is effective for screening ADD when combined with D-dimer, with a sensitivity of 93.1%–99.8% and a specificity of 21.8%–67.1%.8 In this case, there was no chest pain or difference in blood pressure between the left and right sides, and no notable findings were found in the patient's medical history. Therefore, the average ADD-RS score was 1. Because the D-dimer level was abnormal, it was considered useful in the posterior region. However, it is difficult to interview patients with impaired consciousness, and it should be recognized that there are limitations to using this score alone to rule out ADD.
In this case, chest MRA was useful for evaluating ADD. At our hospital, we performed a noncontrast chest CT as a screening test for ADD when evaluating stroke. However, if typical findings such as a high-intensity crescent, linear high-density, or medial calcification are not visible on noncontrast CT, approximately 6.7% of ADD cases will remain undiagnosed.9 Although transthoracic echocardiography is an excellent auxiliary diagnostic modality for aortic dissection, it is insufficient for diagnostic exclusion when pericardial effusion or false lumen formation in the ascending aorta is not confirmed.
MRI for aortic dissection is reported to have high diagnostic accuracy, with a positive likelihood ratio (PLR) of 14.1 for transesophageal echocardiography and 13.9 and 25.3 for MRI.10 However, because of the longer acquisition time (approximately 20 min for thoracic MRA vs. 8 min for contrast-enhanced CTA), MRI is often considered less suitable for emergency diagnosis, despite its high diagnostic accuracy.
Since the widespread adoption of mechanical thrombectomy in 2018, thoracic MRA has become increasingly common in acute stroke protocols. It is routinely performed in conjunction with head and neck MRA to assess vascular anatomy and confirm access routes for endovascular treatment. In addition to its role in procedural planning, thoracic MRA can also incidentally detect acute aortic dissection, as seen in the present case, underscoring its diagnostic value in patients with stroke. In such cases, in which the dissection does not extend to the head and neck, it is difficult to make a diagnosis based on head and neck MRA alone. However, a definitive diagnosis can be made by simultaneously performing MRA of the aortic arch. While thoracic MRA suggests a possible dissection, contrast-enhanced CTA is crucial for mapping the full extent of the dissection and assessing the involvement of major arterial branches, which cannot be fully evaluated on noncontrast MRA due to limitations in spatial resolution and susceptibility to motion artifacts. It is essential not to miss the diagnosis of ADD, and we propose that it is valuable to perform chest MRA or contrast-enhanced CTA prior to intravenous tPA administration in order to rule out acute aortic dissection.
CONCLUSION
The early diagnosis and treatment of acute cerebral infarction are crucially linked to patient prognosis. Therefore, it is essential to rule out the presence of ADD. However, because stroke-like symptoms in ADD can arise from various mechanisms, they may be overlooked if only head and neck MRA, noncontrast CT, and echocardiography are used to assess patients.
Incorporating chest MRA into the evaluation of stroke enables not only the planning of endovascular treatment strategies but also the assessment of ADD, allowing timely and appropriate management of the patient. Chest MRA is a valuable tool for diagnosing ADD in patients with symptoms of ischemic stroke.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
ETHICS STATEMENT
Approval of the research protocol: N/A.
Informed consent: The patient provided written informed consent for the publication of this case report and all accompanying images.
Registry and the registration no. of the study/trial: N/A.
Animal studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
Data sharing is not applicable to this article as no new data were created or analyzed in this study.