Impact of COVID-19 on resuscitation after hospital arrival for patients with out-of-hospital cardiac arrest: An interrupted time series analysis
Abstract
Background
In this study, we aimed to determine the effects of the coronavirus disease 2019 (COVID-19) pandemic on in-hospital cardiopulmonary resuscitation (CPR) in patients with out-of-hospital cardiac arrest (OHCA).
Methods and Results
Using the Japanese Diagnosis Procedure Combination inpatient database, we included patients with OHCA who were transported to hospitals between April 2018 and March 2021. Patients were categorized into groups, before and during the COVID-19 pandemic, according to the day of admission (before or after April 1, 2020, respectively). The primary outcome was in-hospital CPR duration after hospital arrival, and secondary outcomes included in-hospital death, intubation, and other resuscitation-related treatments. We examined the impact of the pandemic using interrupted time series (ITS) analyses. Among 144,867 patients with OHCA, 82,425 died in the outpatient department (53,286 before the pandemic and 29,139 during the pandemic) during the study period. The ITS analyses for patients who died in the outpatient department showed no significant level change in CPR duration after hospital arrival (0.41 min increase; 95% confidence interval [CI]: −0.54 to 1.4; p = 0.39), but the intubation rate was significantly lower (−5.9%; 95% CI: −8.4 to 3.4; p < 0.001). In-hospital death among all patients with OHCA showed a significant increase in trend (0.41% per month; 95% CI: 0.081–0.74; p = 0.016).
Conclusions
The COVID-19 pandemic had little impact on CPR duration after hospital arrival; however, there was a marked decrease in intubation for patients with OHCA after hospital arrival.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has affected more than 774 million patients and resulted in approximately 7 million deaths worldwide by February 4, 2024.1 It has affected overall public health and access to healthcare. Previous studies have reported an increase in the incidence of out-of-hospital cardiac arrest (OHCA) and in-hospital mortality of patients with OHCA during the COVID-19 pandemic due to prehospital factors, such as lower rates of bystander cardiopulmonary resuscitation (CPR) and early defibrillation.2-8 These reports have examined the impact of the COVID-19 pandemic on the prehospital OHCA care system; however, to the best of our knowledge, the changes in in-hospital OHCA care during the pandemic have not yet been clarified. As lower rates and early termination of CPR in hospitals increase mortality,9 the change in mortality may have been caused by the change in in-hospital OHCA care following hospital arrival during the COVID-19 period.
Therefore, we aimed to investigate changes in in-hospital resuscitation care and outcomes during the COVID-19 pandemic by utilizing a nationwide inpatient database in Japan and conducting interrupted time series (ITS) analyses. We hypothesized that, due to increased reluctance among hospital staff to perform CPR and aerosolizing procedures, such as intubation during the pandemic, the duration of CPR would be shorter, and fewer resuscitation-related procedures would be carried out. Additionally, we anticipated that these trends would be more pronounced in low-volume hospitals, where staff might have had less experience with infection prevention measures.
METHODS
Study design and data
This retrospective cohort study used a nationwide administrative inpatient database, the Japanese Diagnosis Procedure Combination (DPC) database, details of which have been reported elsewhere.10 The DPC database contains discharge abstracts and administrative claims data from more than 1600 acute care hospitals in Japan. All academic hospitals are obliged to contribute to the database; however, participation by community hospitals is voluntary. Hence, this database covers approximately 90% of all tertiary-care emergency hospitals in Japan.10 The DPC database contains the following data for all hospitalizations: age; sex; diagnoses recorded using the International Classification of Diseases, 10th Revision (ICD-10) codes; procedures recorded using Japanese medical procedure codes; and discharge status. Patients were followed up until discharge from the hospital. In a previous study that examined the validity of recorded diagnoses and procedures in a database, the specificity of the recorded diagnoses exceeded 96%, the sensitivity ranged from 50% to 80%, and the specificity and sensitivity of recorded procedures exceeded 90%.11
This study was approved by the Institutional Review Board of the University of Tokyo (approval number: 3501-5; May 19, 2021. Title: Clinical Epidemiological Studies using the DPC (Diagnosis Procedure Combination) data). It was conducted in accordance with the ethical standards of the responsible committee on human experimentation and the tenets of the 1975 Declaration of Helsinki. Given the unidentified nature of the data, the need for informed consent was waived. The authors first accessed the data for this research purpose on August 7, 2022. Data cannot be made publicly available for ethical reasons, as they involve patient information. However, the data can be made available to interested researchers upon request to the corresponding author, subject to obtaining ethical approval.
Study population
We identified all patients with OHCA who were eventually cared for in hospitals between April 2018 and March 2021. In this study, patients with OHCA were defined as those with the ICD-10 code I46 (cardiac arrest) as their admission-precipitating diagnosis. Furthermore, all patients with OHCA were registered in the database as admitted to hospitals, even if they were declared dead in emergency rooms or outpatient departments. Consequently, only patients with OHCA who were not transferred to the hospital were excluded from the study. The inclusion criteria encompassed patients treated in hospitals that reported at least one OHCA case in each fiscal year from 2018 to 2020. The onset of the COVID-19 pandemic was defined as April 1, 2020, based on the COVID-19 expansion trend in Japan.
Variables
We identified the following variables from the database: age; sex; pre-transportation location; presence of dementia; cause of death (non-traumatic, traumatic, drug over dose, drowning, or asphyxia); tertiary hospital admission; intensive care unit (ICU) admission; high-dependency unit (HDU) admission; fiscal year of admission; diagnoses based on ICD-1012; procedures performed on the day of admission; and medications used on the day of admission, including epinephrine and antiarrhythmic drugs.
Outcomes
The primary outcome was the duration of in-hospital CPR after hospital arrival. This duration was calculated as the time, in minutes, from the initiation to the cessation of closed chest compressions in the hospital, including the emergency departments. CPR duration was calculated only for patients with recorded CPR performance, and patients without CPR duration record were excluded. It is used for health insurance reimbursement to hospitals (Japanese procedure code J046),13 and another study used this variable of CPR duration in the DPC database.13
The secondary outcomes were in-hospital death; neurologically favorable survival discharge; receiving intubation, cardioversion, adrenaline, antiarrhythmic agents (amiodarone, sotalol, nifekalant, bepridil, verapamil, digitalis, and Class Ia, Ib, and Ic antiarrhythmic agents), extracorporeal cardiopulmonary resuscitation (ECPR), coronary angiography (CAG) or targeted temperature management (TTM); ICU or HDU admission; length of hospital stay; and total costs. Neurologically favorable survival discharge was defined as survival with a Japan Coma Scale score of 0–2 at the time of discharge.14
Statistical analysis
Patient characteristics before and during the COVID-19 pandemic were compared using the Wilcoxon rank-sum test for continuous variables and the chi-square test for binary variables, as appropriate.
For subgroup analyses, we separated hospitals into two groups according to the volume of OHCA cases (high- and low-volume hospitals) and performed the ITS analysis in the same manner. High-volume centers were defined as ≥40 cases of OHCA per year.16, 17 We performed the ITS analysis on CPR duration, CPR receiving rate, intubation, cardioversion, adrenaline use, and antiarrhythmic agents use solely for patients who died in the outpatient department, including the emergency department, to mitigate the bias that an early return of spontaneous circulation (ROSC) may lead to early suspension of resuscitation efforts. CPR duration tends to be shorter for patients who achieve ROSC because hospital staff typically suspend CPR immediately upon confirming ROSC in patients with cardiac arrest. Some patients may achieve ROSC even before the administration of the first dose of epinephrine or antiarrhythmic drugs, often due to the effectiveness of the initial defibrillation. If the proportion of patients achieving ROSC differs between the groups, variations in CPR duration or drug usage may not accurately reflect changes in the treatment approach of hospital staff. Therefore, our analysis focused on patients who were not pronounced dead in the outpatient department. Additionally, we conducted exploratory subgroup analyses based on age groups (<65 and ≥65 years) and within the population that received shocks.
Data were complete for all variables other than total cost, and main analyses were conducted with complete cases. The same ITS analysis was conducted as a sensitivity analysis with multiple imputation using chained equations for CPR duration in the excluded patients lacking any CPR duration data. Ten imputed datasets were used, and estimates were pooled using Rubin's rules.18
All analyses were performed using STATA/SE software (Version 17.0; STATA Corp). All hypothesis tests were two-sided with a significance level of 0.05.
RESULTS
We determined 144,867 patients with OHCA in 814 hospitals. The patients were divided into two groups: 96,168 before the COVID-19 pandemic and 48,699 during the COVID-19 pandemic (Table 1). The mean age was modestly but significantly higher during the COVID-19 pandemic than that before the pandemic (73.2 before vs. 73.6 during the COVID-19 pandemic, p < 0.001). The number of patients with OHCA admitted to tertiary hospitals decreased significantly during the pandemic (62.8% before vs. 61.9% during; p < 0.001).
| Total | Before COVID-19 | During COVID-19 | p-Value | |
|---|---|---|---|---|
| N = 144,867 | N = 96,168 | N = 48,699 | ||
| Age, mean (SD) | 73.3 (17.9) | 73.2 (18.0) | 73.6 (17.7) | <0.001 |
| Male, n (%) | 85,964 (59.3%) | 56,955 (59.2%) | 29,009 (59.6%) | 0.21 |
| Tertiary Hospital, n (%) | 90,566 (62.5%) | 60,431 (62.8%) | 30,135 (61.9%) | <0.001 |
| Transported from, n (%) | ||||
| Home | 127,350 (87.9%) | 84,341 (87.7%) | 43,009 (88.3%) | <0.001 |
| Hospital | 3085 (2.1%) | 2213 (2.3%) | 872 (1.8%) | |
| Nursing Home | 14,432 (10.0%) | 9614 (10.0%) | 4818 (9.9%) | |
| Dementia | 20,109 (13.9%) | 13,582 (14.1%) | 6527 (13.4%) | <0.001 |
| Cause of OHCA, n (%) | ||||
| Non-traumatic | 136,757 (94.4%) | 90,772 (94.4%) | 45,985 (94.4%) | 0.66 |
| Traumatic | 2660 (1.8%) | 1793 (1.9%) | 867 (1.8%) | |
| Drug Overdose | 250 (0.2%) | 164 (0.2%) | 86 (0.2%) | |
| Drowning | 1582 (1.1%) | 1059 (1.1%) | 523 (1.1%) | |
| Asphyxia | 3608 (2.5%) | 2375 (2.5%) | 1233 (2.5%) |
- Abbreviations: COVID-19, coronavirus disease 2019; OHCA, out-of-hospital cardiac arrest; SD, standard deviation.
The number of patients who were registered as having undergone CPR was 104,805. The average CPR duration was 25.6 min before the pandemic and 24.7 min during the pandemic. There were 85,679 (89.1%) and 44,476 (91.3%) deaths before and during the pandemic, respectively, and 54,478 (56.6%) and 25,243 (51.8%) intubations before and during the pandemic, respectively. Additionally, there were 4616 missing values for total cost. However, there were no missing data for other outcomes.
ITS analysis revealed that the level change of CPR duration was a 0.48 min decrease (95% confidence interval [CI]: −1.37 to 0.41; p = 0.28), which was not significantly different (Table 2 and Figure 1A). In contrast, the intubation rate had a significantly decreased level change (−3.4%; 95% CI: −4.8 to 2.0; p < 0.001; Figure 1B), and the level change of antiarrhythmic agents use significantly increased (1.6%; 95% CI: 0.93–2.3; p < 0.001). The level change of other outcomes, including in-hospital mortality, neurologically favorable survival discharge, ECPR, ICU admission, HDU admission, and length of hospital stay, was not statistically significant (Table 2, Figure 1C, and Figure S1).
| Change in level | Change in trend (/month) | |||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-Value | Coefficient | 95% CI | p-Value | |
| CPR duration (min) | −0.48 | (−1.37 to 0.41) | 0.28 | 0.089 | (0.017 to 0.16) | 0.017 |
| Intubation (%) | −3.4 | (−4.8 to −2.0) | <0.001 | −0.0022 | (−0.17 to 0.16) | 0.98 |
| Cardioversion (%) | 0.62 | (−0.070 to 1.3) | 0.077 | −0.033 | (−0.11 to 0.044) | 0.39 |
| Epinephrine use (%) | −0.94 | (−2.3 to 0.44) | 0.18 | 0.18 | (0.050 to 0.31) | 0.008 |
| Antiarrhythmic agents use (%) | 1.6 | (0.93 to 2.3) | <0.001 | 0.23 | (0.17 to 0.29) | <0.001 |
| In-hospital mortality (%) | −0.55 | (−2.7 to 1.6) | 0.6 | 0.41 | (0.081 to 0.74) | 0.016 |
| Neurologically favorable survival discharge (%) | 0.86 | (−0.80 to 2.5) | 0.30 | −0.32 | (−0.55 to 0.087) | 0.009 |
| ECPR (%) | 0.094 | (−0.71 to 0.90) | 0.81 | −0.054 | (−0.15 to 0.040) | 0.25 |
| CAG (%) | 0.067 | (−0.68 to 0.81) | 0.86 | −0.1 | (−0.19 to 0.013) | 0.026 |
| TTM (%) | 0.45 | (−0.65 to 1.6) | 0.41 | −0.16 | (−0.30 to 0.026) | 0.022 |
| ICU admission (%) | 0.016 | (−2.3 to 2.4) | 0.99 | −0.16 | (−0.49 to 0.18) | 0.35 |
| HDU admission (%) | 0.24 | (−1.1 to 1.6) | 0.73 | 0.029 | (−0.13 to 0.19) | 0.71 |
| Length of stay (days) | −0.052 | (−1.1 to 0.97) | 0.92 | −0.25 | (−0.41 to 0.099) | 0.002 |
| Total cost (thousand JPY) | 52 | (−79 to 183) | 0.42 | −24 | (−43 to 5.4) | 0.013 |
- Note: N = 104,805 for CPR duration, N = 144,867 for other outcomes.
- Abbreviations: CAG, coronary angiography; CI, confidence interval; CPR, cardiopulmonary resuscitation; ECPR, extracorporeal cardiopulmonary resuscitation; HDU, high-dependency unit; ICU, intensive care unit; JPY, Japanese Yen; OHCA, out-of-hospital cardiac arrest; TTM, targeted temperature management.
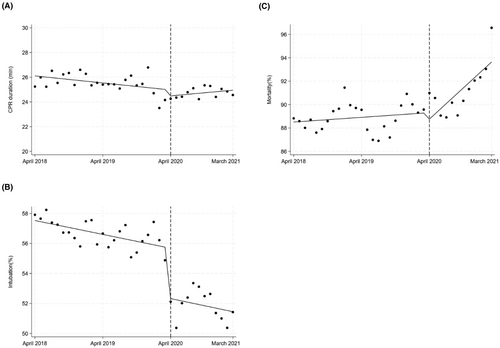
In terms of trend changes, CPR duration (0.089 min per month; 95% CI: 0.017–0.16; p = 0.017), epinephrine use (0.18% per month; 95% CI: 0.050–0.31; p = 0.008), antiarrhythmic agent use (0.23% per month; 95% CI: 0.17–0.29; p < 0.001), and in-hospital mortality (0.41% per month; 95% CI: 0.081–0.74; p = 0.016) significantly increased, while neurologically favorable survival discharge (−0.32% per month; 95% CI −0.55 to 0.087; p = 0.009), CAG (−0.10% per month; 95% CI −0.19 to 0.013; p = 0.026), TTM (−0.16% per month; 95% CI −0.30 to 0.026; p = 0.022), length of hospital stay (−0.25 days per month; 95% CI −0.41 to 0.099; p = 0.002), and total cost (−24,000 thousand Japanese Yen per month; 95% CI: −43,000 to 5.4000; p = 0.013) significantly decreased (Table 2).
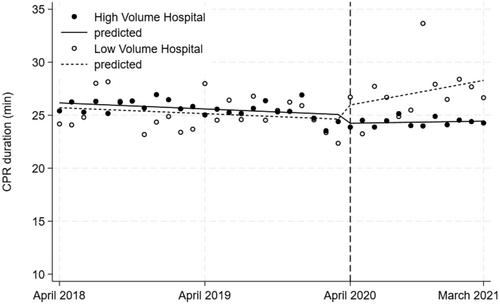
We conducted a subgroup analysis of the high- and low-volume hospitals. The characteristics of each group are shown in Table S1. In that subgroup analysis, there were no significant changes in CPR duration levels in either group, as shown in Figure 2 and Table 3. For patients who died in the outpatient department, the level of intubation significantly decreased by 5.9% (95% CI: −8.4 to 3.4%; p < 0.001), while the level of antiarrhythmic agent use significantly increased by 0.59% (95% CI: 0.26–0.93%; p = 0.001). The trend change in antiarrhythmic agent use also significantly increased by 0.11% per month (95% CI: 0.073–0.14%; p < 0.001). These results are shown in Table S2 and Figure S2.
| Change in level | Change in trend (/month) | |||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-Value | Coefficient | 95% CI | p-Value | |
| High-volume hospitals (min) | −0.78 | (−1.7 to 0.16) | 0.10 | 0.065 | (−0.0085 to 0.14) | 0.081 |
| Low-volume hospitals (min) | 1.4 | (−1.2 to 3.9) | 0.28 | 0.26 | (−0.034 to 0.55) | 0.081 |
- Abbreviations: CI, confidence interval; CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest.
For patients who were not declared dead in the outpatient department, the CPR duration level significantly decreased by 2.1 min (95% CI: −4.2 to 0.13; p = 0.038), while antiarrhythmic agent use significantly increased by 2.8% (95% CI: 1.7–4.0%; p < 0.001). The trend change showed significant increases in CPR duration (0.20 min per month; 95% CI: 0.036–0.36; p = 0.018), epinephrine use (0.55% per month; 95% CI: 0.17–0.93; p = 0.005), antiarrhythmic agent use (0.38% per month; 95% CI: 0.28–0.48; p < 0.001), in-hospital mortality (0.81% per month; 95% CI: 0.14–1.5; p = 0.019), and HDU admission (0.27% per month; 95% CI: 0.015–0.52; p = 0.038). Conversely, there were significant decreases in CAG usage (−0.19% per month; 95% CI: −0.35 to 0.035; p = 0.018), TTM usage (−0.33% per month; 95% CI: −0.59 to 0.065; p = 0.016), length of hospital stay (−0.58 days per month; 95% CI: −0.91 to 0.24; p = 0.002), and total cost (−51,000 Japanese Yen per month; 95% CI: −88,000 to 14,000; p = 0.008). Those results are shown in Table S2 and Figure S3.
Other results of subgroup analyses are detailed in Table S3. Patients younger than 65 years showed no significant changes in level or trend between the pre-pandemic and pandemic periods. A sensitivity analysis with multiple imputation for CPR duration showed results similar to those of the main analyses (Level change: −0.32 min; 95% CI −1.0 to 0.41; p = 0.38; Trend change: 0.13 min per month; 95% CI 0.071–0.19; p < 0.001).
DISCUSSION
This nationwide observational study focused on the impact of the COVID-19 pandemic on CPR duration on patients with OHCA after hospital arrival and revealed that there was no significant change in CPR duration before and during the COVID-19 pandemic. Previous studies on the impact of the COVID-19 pandemic on patients with OHCA have reported a decrease in prehospital resuscitation procedures.4, 6, 7 The present study revealed that the duration of CPR after hospital arrival did not decrease during the pandemic. The difference in CPR time between pre- and in-hospital CPR may be explained by differences in CPR providers. CPR conducted in the hospital was performed mostly by medical staff, whereas prehospital CPR was performed partly by laypersons. Laypersons may hesitate to conduct CPR because of the possible risk of COVID-19; however, hospital staff may be ready for precautions against COVID-19.
Hospital staff performed the same amount of CPR (i.e., duration) on patients with OHCA during the pandemic, despite the risk of exposure to SARS-COV-2.19 The older age of patients with OHCA during the pandemic had little impact, possibly because the difference in patient age was relatively small. The present study also showed that the CPR duration was preserved even in low-volume hospitals. A shortage of personal protection equipment during the COVID-19 pandemic occurred in relatively small hospitals compared with that in tertiary hospitals.20 The baseline characteristics of patients with OHCA in low-volume hospitals during the COVID-19 pandemic were comparable to those of the overall patient population, and the duration of CPR was maintained, suggesting that adequate medical resources were available even in non-tertiary hospitals in Japan for critical conditions, such as CPR. The ITS analysis detected a statistically significant increase in the trend change of CPR duration. ITS analyses evaluate the difference in intercept at the time of event occurrence (level change) and change in angle after the event (trend change) using generalized linear model with separated samples before and after the event. This methodology can reveal whether a significant difference is observed in either the level change or the trend change independently. For example, a previous study on Zolpidem use in Korea demonstrated a considerable change in the intercept alone, suggesting an immediate impact of media broadcasting on the use of Zolpidem.21
The marked decrease in level change and the subsequent increase in trend change in CPR duration for patients who were not declared dead in the outpatient department (Figure S2A) may suggest the following scenario: At the onset of the pandemic, patients with OHCA may not have received CPR for a sufficient duration, leading to a higher mortality rate in the outpatient department. The gradual return of CPR duration to baseline levels over time may indicate that healthcare providers adapted to the challenges posed by the COVID-19 pandemic, particularly regarding infection control measures. However, it is noteworthy that the proportion of intubated patients decreased during the pandemic, consistent with findings from previous studies.2, 3 This may indicate the hospital staff's attitudes toward avoiding intubation as an aerosolizing procedure. However, the discrepancy between unchanged CPR duration and decreased intubation rates suggests that hospital staff may not have recognized chest compressions as an aerosolizing procedure, in contrast to findings from previous studies.19 The level change in intubation among patients younger than 65 years was insignificant. This result suggests that hospital staff continued to perform aerosol-producing resuscitation procedures for younger patients, likely because the possibility of rescuing these patients was higher than that of older patients.
The observed decrease in intubation rates may be attributable to reduced prehospital intubation by EMS, as reported in a study from New York City.22 In Japan, most EMS intubations are not recorded in the DPC database due to reimbursement rules. According to reports from the Fire and Disaster Management Agency in Japan, the ratio of intubations to CPR by EMS was 6.8% in 2018, 6.7% in 2019, and 7.5% in 2020.23-25 These variations do not fully account for the observed changes in intubation levels, suggesting that changes in EMS intubation rates had minimal impact on the overall level change observed in this study.
The statistically insignificant changes in ECPR, adrenaline use, CAG, TTM, ICU admission, and HDU admission indicate that the pandemic had a minimal impact on these essential procedures for patients with OHCA at the beginning of the pandemic. However, as CAG and TTM are generally performed on patients with a better prognosis, the remarkable trend changes showing increased mortality and decreased CAG and TTM suggest a gradual decline in the proportion of successfully resuscitated patients with OHCA over time. This decline may reflect worsening patient conditions, such as an increased proportion of unwitnessed OHCA cases and reduced bystander CPR, as other procedures and treatments remained largely unchanged. Although decreased intubation rates may have contributed to increased mortality, further analysis with more detailed data is needed to confirm this hypothesis.
The level change and trend change in antiarrhythmic drug use increased considerably. A descending trend in the use of antiarrhythmic agents was observed starting in 2018, reaching a plateau in 2019. In 2020, the monthly use of antiarrhythmic agents remained stable, suggesting that the trend change observed in antiarrhythmic drug use occurred in 2019 and was likely unrelated to the COVID-19 pandemic. The generalized linear model used in the interrupted time series analysis demonstrated statistically significant changes in both intercept and trend when the data were divided before and after April 2020. To further validate this, an additional analysis comparing data from before and after April 2019 showed a better fit to the observations. Additionally, some antiarrhythmic drugs examined in this study were not recommended for patients with cardiac arrest according to recent guidelines. The reduction in the use of these drugs may be related to the observed stabilization of antiarrhythmic drug use after 2019.
Overall, this study suggests that the onset of the COVID-19 pandemic had minimal impact on in-hospital care for patients with OHCA, except for intubation, indicating that the procedures were applicable to the patient. However, the decrease in intubation rates may have contributed to increased mortality. Future considerations for managing OHCA during pandemics, especially those caused by unknown pathogens, should include evaluating factors related to intubation, CAG, and TTM to help mitigate mortality.
LIMITATIONS
The present study has several limitations. First, due to data access constraints, the dataset only includes information up until March 2021, covering just 1 year of the pandemic period. Larger and more severe waves of the COVID-19 pandemic occurred in Japan after this period, which were not captured in this study. Additionally, the period defined as post-COVID-19 in Japan began after May 2023, following a change in the legal status of the pandemic. To comprehensively assess long-term impacts, data extending to at least May 2024 would be necessary for a robust ITS analysis. Unfortunately, such data will only become available around 2025 or later. This study provides insights into changes in treatment attitudes of hospital staff during the pandemic but does not encompass the effects of subsequent waves.
Second, the use of ICD-10 codes to identify patients with OHCA may have resulted in misclassification. We defined patients with OHCA using the ICD-10 code I46 (cardiac arrest) as the diagnosis precipitating admission. This approach may include patients who experienced cardiac arrest shortly after hospital arrival for unclear reasons.
Third, the proportion of patients with OHCA who were not registered as having undergone CPR was relatively high. Most patients without any CPR duration data were presumed to have achieved ROSC before hospital arrival, as these patients tended to be younger (70.4 vs. 74.4 years) and had lower mortality (73.3% vs. 96.2%). This may have led to an outcome bias. However, the results of the analysis with multiple imputation were similar to those of the main analysis. This suggests that the impact on CPR duration due to the relatively high proportion of patients without CPR registration is limited.
Fourth, the administrative database did not include details typically recorded in the Utstein style, such as information on the prehospital setting—e.g., presence of a witness, bystander CPR, no-flow time from collapse to initiation of CPR, automated external defibrillator use, event location, initial rhythm, quality of CPR, interruptions in chest compression, ROSC, and interventions by paramedics (e.g., adrenaline administration, intubation, and duration of CPR by paramedics). The absence of these variables limits the depth of analysis regarding prehospital care and its impact on outcomes.26
Fifth, the database also did not contain the information of ‘Do Not Attempt Resuscitation (DNAR)’ orders, and adjustment of with or without DNAR cannot be conducted. CPR duration might be shorter for advanced-age patients with DNAR declaration. However, in Japan, the number of people who declared DNAR is very small, sitting at approximately 10%, according to previous studies.27, 28 The proportion of patients with DNAR of written format is smaller.29 Although it was assumed that the number of these older patients with and without reported DNAR did not seem to change before and during the COVID-19 pandemic, further evaluation is necessary to clarify the impact of DNAR and super aging on CPR duration.
CONCLUSION
This nationwide observational study found that the COVID-19 pandemic had minimal impact on in-hospital care for patients with OHCA in terms of CPR duration. While most essential procedures for patients with OHCA were maintained at the onset of the pandemic, there was a remarkable decrease in the proportion of patients who were intubated, and the trend in mortality notably increased during this period. Further research is needed to clarify the factors contributing to the decreased intubation rates and address potential strategies for reducing mortality in future pandemics caused by unknown pathogens.
ACKNOWLEDGMENTS
We would like to thank Editage (www.editage.com) for their writing support on the manuscript.
FUNDING INFORMATION
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (grant numbers: 21AA2007 and 20AA2005), and the Ministry of Education, Culture, Sports, Science and Technology, Japan (grant number: 20H03907). The funding sources were not involved in the study.
CONFLICT OF INTEREST STATEMENT
HY reports receiving grants from the Ministry of Health, Labour and Welfare, Japan, and the Ministry of Education, Culture, Sports, Science and Technology, Japan during the conduct of the study. No other disclosures were reported.
ETHICS STATEMENT
Approval of the research protocol: The protocol for this research project has been approved by the Institutional Review Board of the University of Tokyo (approval number: 3501-5; May 19, 2021. Title: Clinical Epidemiological Studies using the DPC (Diagnosis Procedure Combination) data), and it conforms to the provisions of the Declaration of Helsinki.
Informed consent: N/A. Given the unidentified nature of the data, the need for informed consent was waived.
Registry and the Registration No. of the study: N/A.
Animal Studies: N/A.
Open Research
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.