Reversible hyperammonemic encephalopathy after gastrointestinal bleeding
An 81-year-old woman presented with massive melena. She required urgent hospitalization because of hyperprothrombinemia (international normalized ratio >9.9), induced by warfarin treatment following double valve replacement surgery she underwent 35 years prior, and had cirrhosis caused by chronic liver congestion.
The next day, she became comatose (serum ammonia level, 417 μg/dL) and was diagnosed with hepatic encephalopathy with acute hyperammonemia. Despite the decrease in serum levels (53 μg/dL) following 3-day lactulose and rifaximin treatment, her consciousness level remained low (Glasgow Coma Scale, 6). Electroencephalogram on day 8 showed triphasic waves, but no obvious epileptic discharges. Brain magnetic resonance imaging (MRI) on day 1 was unremarkable (Fig. 1A–C) and showed bilateral and symmetrical cortical swelling in the insular, cingulate, frontal, and occipital cortices on day 10 (Fig. 1D–F), and showed reduction in the extent of the lesion at 3 weeks post-hospitalization (Fig. 1G–I). Her consciousness level recovered slightly later than the MRI findings.
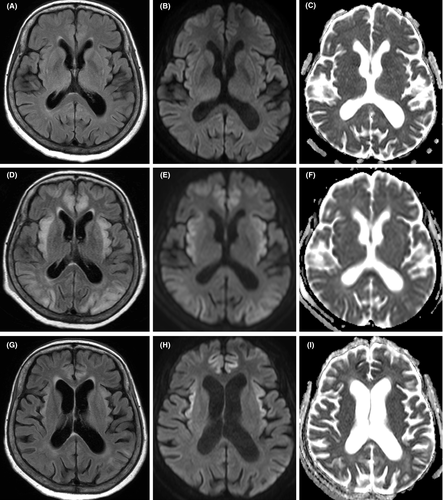
Ammonia detoxification in the brain occurs through glutamine formation through the glutamine synthesis pathway in astrocytes, leading to glutamine-induced astrocyte swelling and subsequent cerebral edema and even encephalopathy.1 Brain MRIs – which are essential in differential diagnoses – show symmetrical signal abnormalities in the insular and cingulate cortices.2-4 Close attention should be paid to secondary encephalopathy in patients with hyperammonemia.
Funding information
None.
Disclosure
Approval of the research protocol: N/A.
Registry and the registration no. of the study/trial: N/A.
Informed consent: Written informed consent was obtained from the patient.
Animal studies: N/A.
Conflict of interest: None.