How to facilitate a rapid response system in Japan: a promotion course based on TeamSTEPPS
Funding Information
This work was supported by Japan Society for the Promotion of Science KAKENHI Grant Number 15K08865. The funding source had no role in the design, practice, or analysis of this study.
Abstract
Aim
In Japan, the number of facilities introducing a rapid response system (RRS) has been increasing. However, many institutions have had unsuccessful implementations. In order to implement RRS smoothly, a plan that meets the needs of each hospital is needed.
Methods
Rapid response system teams from each hospital, including a physician and staff in charge of medical safety, from the RRS online registry were invited to attend a workshop. The workshop aimed to develop and implement RRS. The course curriculum was based on the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) developed in the USA. Participating facilities were required to formulate an RRS introduction plan referring to Kotter’s 8-step change model to overcome barriers in the implementation of RRS. The change in medical emergency team activations comparing the intervention and control group hospitals was compared.
Results
Sixteen institutions were eligible for this study. After participating in the workshop, there was a tendency toward more frequent activation of medical emergency teams in the intervention group (P = 0.075). According to a self-evaluation from each facility, there is great difficulty in overcoming the 5th step of Kotter’s model (empower people to act the vision).
Conclusion
This step-by-step evaluation clearly identified a problem with implementation and provided measures for resolution corresponding to each facility. There was a major barrier to overcome the 5th step of Kotter’s model in leading change, which represents the attitude toward implementing RRS in institutions.
Introduction
The rapid response system (RRS) was developed to enable early detection of adverse events in hospitalized patients, leading to early intervention. The Japanese Coalition for Patient Safety launched the RRS in the 6th action plan in 2008.1 This action plan has expanded the recognition of RRS. The in-hospital emergency committee was organized in the Japan Society for Emergency Medicine in 2010 and promoted RRS education.2 The Japanese RRS online registry began as a joint project by the Joint Committee of the Japan Society for Emergency Medicine and the Japanese Society of Intensive Care Medicine, and a multicenter case registry of RRS has been developed.3 A medical accident investigation system was started in Japan in 2015, making it necessary to grasp the whole picture of “unexpected deaths” related to medical care and analyze the causes of death at each facility. In the revision of the health-care fee structure in Japan in 2018, the evaluation criteria for emergency and critical care centers were revised.4 Among these changed, a system for in-hospital emergencies was added as a new criterion, which has increased the motivation for implementing RRS in facilities in Japan.
Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS)5, 6 is an evidence-based systematic approach to integrate teamwork into practice developed by the US Department of Defense and the Agency for Healthcare Research and Quality. TeamSTEPPS is recognized in fields such as obstetric emergency care and medical safety through the TeamSTEPPS Japan Alliance7, 8 in Japan. TeamSTEPPS introduces Kotter’s 8-step change model as a strategy to foster an organization’s patient safety culture.
Recently, several facilities in Japan have reported that the rate of adverse events decreased after the introduction of RRS.9-11 Although good results have been reported by implementing RRS in North America, Europe and Australia, we do not know whether these methods can be applied in Japan with its different medical culture. Each facility has implemented RRS based on trial and error. In this study, we evaluated the effectiveness of the RRS promotion course based on TeamSTEPPS to overcome barriers to RRS implementation and identified specific barriers.
Methods
We recruited facilities in Japan from the RRS online registry (41 facilities), which was introduced in 2015. Of the facilities registered in the RRS online registry, 14 that participated in this RRS promotion course were defined as the intervention group and 27 that did not participate in the course were defined as the control group. The goal at each facility was to promote the implementation of RRS. The course was designed to focus not on an individual but on the hospital unit as a team. Physicians, nurses, hospital executives, and medical safety managers were recruited to participate in the course. In consideration of venue restrictions and balance with other hospitals, the number of participants per hospital was set to 4–5 persons and we received prior consent to use the data obtained in this course as research from participating hospitals. Participants were instructed to read “Our Iceberg is Melting”12 before the course to understand the 8 steps (Table 1) in Kotter’s model of change. A 1-day RRS promotion course was held on 4 October 2015, and repeated on 16 January 2016 (Fig. 1, Table 2). In this course, each hospital delegation created RRS action plans based on the culture and environment at their facility using Kotter’s model (Table 3). After attending the course, the group from each hospital made efforts to execute their RRS action plans. We monitored the number of medical emergency team (MET) activations at each facility through the RRS online registry. The RRS online registry form was electronically accessed by registered institutions and the whole database is securely managed by the University Hospital Medical Information Network – Clinical Trial Research (UMIN-CTR) at the University of Tokyo (Tokyo, Japan). This study was registered in UMIN-CTR (UMIN000012045) and approved by the Institutional Review Board committee in this institution. To evaluate the effectiveness of the RRS promotion course, the number of MET activations at each hospital in the intervention group was analyzed and compared with the control group.
| 1st step | Communicate urgency |
| 2nd step | Build a guiding team |
| 3rd step | Create a vision |
| 4th step | Communicate for buy-in |
| 5th step | Remove obstacles |
| 6th step | Create short-term wins to provide momentum |
| 7th step | Maintain momentum |
| 8th step | Incorporate CHANGE INTO ORGANIZATIONAL CULTURE |

| Title | Educational format | Time (min) | |
|---|---|---|---|
| am | 1. Concept of RRS | Lecture and discussion | 60 |
| 2. Barriers to the implementation of RRS | Workshop | 120 | |
| pm | 3. TeamSTEPPS | Lecture and workshop | 90 |
| 4. Developing an action plan (8 steps) | Presentation and feedback | 120 |
| Step | Proposed plan for each step (reference example) | Interval | Metric |
|---|---|---|---|
| 1 |
In-hospital cardiac arrest case review? Questionnaire survey |
1 year | Number of unexpected deaths |
| 2 | Form a guiding team by leading members | 1 month | Number of MET activations |
| 3 | RRS seminar, poster making | 2 months | |
| 4 |
Briefing session Explanatory meeting at each ward |
3 months | Survey |
| 5 |
Special lecture by a noted speaker Do Not Attempt Resuscitation notices and clarification |
5 months | Survey |
| 6 |
Medical emergency team case study meeting Create a hospital newspaper |
6 months | Held regularly |
| 7 |
Set up a RRS steering committee Critical Care Outreach Team |
1 year | |
| 8 |
Initiative through the hospital Promulgate the philosophy of TeamSTEPPS |
Two follow-up surveys were undertaken: Survey 1 was conducted approximately 1 year after the course, and Survey 2 approximately 2 years later (Fig. 1). Survey 1 examined the degree of achievement for each step in Kotter’s model. In Survey 2, we created 20 original questions based on Kotter’s 8-step model (Table S1) and asked to assess the status of implementation. Participating facilities were divided into successful implementation and unsuccessful implementation groups. The successful implementation group is defined as a MET activation rate more than once per week.
Statistical analysis
Categorical variables, including gender, were compared with the χ2-test. Continuous variables were compared using Student’s t-test. Statistical analysis was carried out using StatFlex version 6 (Artech, Osaka). A P-value <0.05 was considered statistically significant.
Results
Twenty-five facilities (four university hospitals and 21 community hospitals) participated in the RRS promotion course. Seven facilities did not implement RRS during the survey period and two facilities did not respond to the survey. Data for these facilities were excluded from the analysis. Sixteen facilities (including two facilities not participating in the RRS online registry) were eligible for analysis.
Survey 1: Action plan achievement survey
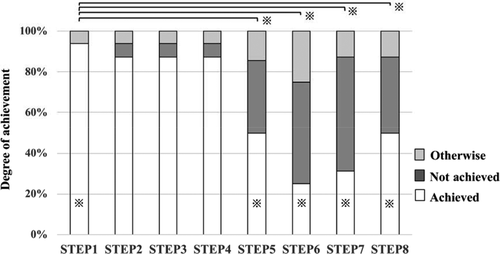
Survey 1 was conducted approximately 1 year after the course to evaluate the progress for implementation of RRS at participating facilities. Figure 2 shows the degree of achievement of the action plan at each step (16 facilities, Fig. 2). Compared to achieving steps 1 through 4, the degree of achievement of steps 5 through 8 was significantly lower (P < 0.05).
Survey 2: Long-term follow-up survey
Two years after the RRS promotion course, we undertook Survey 2 (16 facilities). In this survey regarding the 8-step change model, we asked questions related to the 5th step, “Do you recommend staff to attend an external lecture?” and “Do you provide tuition remission and travel expenses to attend an external workshop?” These two questions were answered positively by significantly more facilities in the successful RRS group than the unsuccessful group (Table 4, P = 0.027 and P = 0.037, respectively).
| Step | Option |
Success group n = 10 |
Failure group n = 6 |
P-value | |||
|---|---|---|---|---|---|---|---|
| 1 | Did you conduct ongoing investigations of unexpected deaths (number of cases)? | Yes | 9 | 90% | 6 | 100% | 0.420 |
| Did you conduct surveys about in-hospital emergency targeted nurses and doctors in the hospital? | Yes | 6 | 60% | 5 | 83% | 0.330 | |
| 2 | Were there any regular trainings for members involved in RRS in your institution? | Yes | 4 | 40% | 1 | 17% | 0.099 |
| 3 | Did you set a goal? (specific example → number of medical emergency team activations, measurement of respiratory rate, etc.) | Yes | 10 | 100% | 4 | 67% | 0.051 |
| Did you have the opportunity to explain the outcomes of RRS to the executives? | Yes | 7 | 70% | 6 | 100% | 0.140 | |
| Did you have enough staff to perform RRS (three or more nurses)? | Yes | 6 | 60% | 3 | 50% | 0.700 | |
| Did you have enough staff to perform RRS (three or more doctors)? | Yes | 6 | 60% | 3 | 50% | 0.180 | |
| 4 | Did you make pocket manuals, name tags, posters etc. in order to inform the activation criteria? | Yes | 10 | 100% | 6 | 100% | 0.700 |
| Did you hold a briefing session about RRS for general physicians? | Yes | 9 | 90% | 5 | 83% | 0.700 | |
| Did you notify and explain the Do Not Attempt Resuscitation in the whole hospital? | Yes | 3 | 30% | 3 | 50% | 1.000 | |
| 5 | Did you hold a special lecture by a noted speaker? | Yes | 4 | 40% | 3 | 50% | 0.700 |
| Did you recommend staff to attend an external lecture? | Yes | 6 | 60% | 1 | 17% | 0.027 | |
| Did you provide tuition remission and travel expenses to join an external workshop? | Yes | 5 | 50% | 0 | 0% | 0.037 | |
| 6 | Did you create in-house newspapers to inform the outcome of RRS? | Yes | 6 | 60% | 5 | 83% | 0.330 |
| Did you work closely with the medical safety management sector? | Positive | 7 | 70% | 6 | 100% | 0.140 | |
| Did you hold regular case study (review) meetings? | Positive | 4 | 40% | 3 | 50% | 0.380 | |
| 7 | Were you introducing a Critical Care Outreach Team? | Yes | 5 | 50% | 1 | 17% | 0.180 |
| 8 | Did you investigate feedback from the medical setting on the evaluation of RRS? | Yes | 4 | 40% | 3 | 50% | 0.700 |
| Was RRS recognized as an important function of your hospital? | Positive | 8 | 80% | 4 | 67% | 0.550 | |
| Was your RRS designed so that it does not rely on individuals? | Positive | 7 | 70% | 5 | 83% | 0.550 | |
- RRS, rapid response system.
Medical emergency team activations
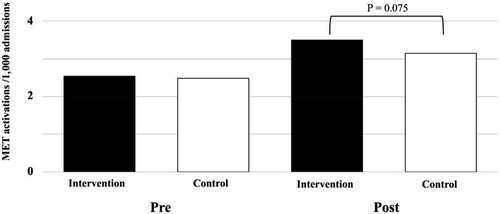
During the year before the RRS promotion course, the number of MET activations was not different comparing the intervention group and the control group (P = 0.744). After the intervention, there was a tendency for more MET activations in the intervention group compared to the control group (P = 0.075, Figs 1 and 3).
Discussion
The RRS is accredited by the Japan Council for Quality Health Care.1 However, to the best of our knowledge, there are few reports to show that RRS is functioning effectively in Japan. In this study, to overcome barriers associated with RRS implementation, we adopted the 8-step program of TeamSTEPPS to facilitate implementation and investigated whether it has an impact on the implementation of RRS. This is the first report in Japan, which shows that the 5th step is especially important to create an environment that encourages RRS activations by removing existing barriers.
There are several reports about the difficulties of RRS implementation.13-15 In the present study, despite recruitment of hospital units rather than individuals to participate in the promotion course, 7 of 21 facilities did not implement RRS over the 2 years following the course. This highlights one of the difficulties associated with implementing an RRS. Shortage of manpower to organize METs, lack of support by administrative staff, inadequate educational system, and no support by physicians, were mentioned as barriers in Japan.13 Even in the survey for participants in this study, the shortage of manpower to promote RRS was stated as the main obstacle (data not shown). However, manpower problems were unique to each hospital and could not be solved in a short period of time. In Japan most patients expect one primary physician to take care of them during their hospitalization and do not want to be seen by other providers, such as RRS team members. This makes it difficult to introduce an RRS or critical care outreach team as a hospital-wide service. As understanding the need for RRS and approval of the RRS by hospital executives is indispensable to implement RRS, this RRS promotion course encouraged hospital executives to participate as much as possible. Even in Europe and the USA, the necessity of an introduction process, continuing support, regular evaluation, and revision are emphasized to overcome the difficulties associated with an RRS.14, 16
Kotter analyzed factors associated with failed transformation in companies and presented 8 steps17 needed to promote changes. These steps comprehensively include change in awareness, building a team, vision/strategy planning, execution, and the change process. There are reports of using these steps in many medical disciplines from Europe and the USA.18-20 As understanding Kotter’s 8 steps is essential for our promotion course, self-study of Kotter’s model prior to the course was a prerequisite so that participants could fully understand the steps. Each facility created an RRS introduction strategy with reference to TeamSTEPPS as the core element of the RRS promotion course21 (Table 3). The 1st to 4th steps served as preparation stages for the RRS implementation process (Fig. 2). The process was more easily achieved up to this stage. For subsequent stages (5th to 8th steps), the difficulty in overcoming obstacles increased while executing each step by trial and error. It seemed that the timing of this investigation had an effect on progress through the steps.
As indices for measuring the effect of RRS, the number of in-hospital cardiac arrests per admitted patients, the number of MET activations, and the number of unexpected intensive care unit transfers are generally used. According to reports from Europe and the USA, a significant decrease in unexpected deaths and in-hospital cardiac arrests did not occur until 4–6 years after the introduction of RRS.22-24 The MERIT study did not show a significant effect, which was attributed to a short observation period.25 Bellomo et al. stated that between 25.8 and 56.4 calls to METs per 1,000 admissions is required to become a “mature” RRS.26 In this study, as an easy-to-follow index, we used the number of MET activations. Assessing the number of activations was facilitated for hospitals participating in the RRS online registry as that data are in the registry.3 Facilities that participated in the RRS promotion course had a tendency to increase the number of MET activations during the same period in comparison with the control group, which suggests that the RRS promotion course played an important role in increasing the number of activations (Fig. 3).
This is the first study to show the effectiveness of introducing RRS using the TeamSTEPPS method. TeamSTEPPS and Kotter’s 8-step program provided hints to consider the strategies needed at each facility. This RRS promotion course has the potential to facilitate implementation and evaluation of RRS at hospitals throughout Japan. The 16 participating institutions were divided into two groups based on the number of MET activations. The survey results related to the 8-step program were compared between the groups. As a result, two 5th step-related questions, “Do you recommend staff to attend external lectures?” and “Do you provide tuition remission and travel expenses for staff to participate in an external workshop?” had significantly more positive answers in the successful group (Table 4). The 5th step has questions related to “Enable action by removing barriers: Removing barriers, such as inefficient processes and hierarchies, provides the freedom to work in sectionalism and results in generating real impact.” This 5th step is consistent with the report that attitudes towards METs were significantly associated with the degree of MET system utilization in the MERIT study.27 Creating an environment conducive to practice RRS is one of the factors associated with successful RRS implementation.
There are some limitations in this study. First, due to the nature of this study, it was impossible to randomly assign intervention groups, which are usually done in randomized controlled trials and no attempt had been made to equalize both groups. Therefore, several confounding factors might have influenced the results of this study. Second, facilities participating in the RRS online registry are composed of mixed hospitals with various stages of RRS implementation. These results might not apply to all hospitals and then further research is necessary. Finally, in this study, the number of MET activations is considerably lower than in reports from North America, Europe and Australia.
Conclusion
Despite some limitations, this study has identified the 5th step as the major barrier to introducing RRS using Kotter’s 8-step change model to promote RRS. Developing a strategy to overcome this 5th step is important to effectively promote RRS. The creation and evaluation of RRS implementation plans using Kotter’s model “Leading Change” is helpful to identify problems and develop remedial measures appropriate for each facility.
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science KAKENHI (Grant No. 15K08865)
Disclosure
Approval of the research protocol: The protocol was approved by the Ethics Committee of NHO Ureshino Medical Center (13-06).
Informed consent: The requirement for informed consent of patients was waived.
Registry and registration no. of the study/trial: This study was registered in UMIN-CTR (UMIN000012045).
Animal studies: N/A.
Conflict of interest: None.