Association between physician-staffed ambulances and patient prognoses after out-of-hospital cardiac arrests with respect to shockable and non-shockable rhythms: a retrospective observational study in a southern area of Shiga Prefecture Japan
Funding information
No funding information provided.
Abstract
Aim
Out-of-hospital cardiac arrests (OHCA) are a significant public health problem; to improve patients’ prognoses, various interventions, such as providing physician-staffed ambulances, have been implemented. We aimed to examine whether physician-staffed ambulances were associated with patients’ prognoses after OHCA with respect to first-monitored rhythms.
Methods
This retrospective observational study was undertaken between 1 September 2011 and 31 December 2015, using data based on Utstein-style guidelines. We extracted data on age, sex, first-monitored rhythm (shockable or non-shockable), presence of a witness, bystander cardiopulmonary resuscitation, time from call to arrival at the scene, out-of-hospital adrenaline administration, out-of-hospital intubation, return of spontaneous circulation before arrival at the hospital, and survival and neurological outcomes 30 days after OHCA, according to cerebral performance categories. We undertook logistic regression analyses to assess the association between physician-staffed ambulances and patients’ prognoses.
Results
A total of 882 OHCA patients were eligible for this study. Physician-staffed ambulances attended to 164 OHCA patients. Multivariable analysis found that in non-shockable rhythm patients, physician-staffed ambulances significantly improved good neurological outcome (odds ratio, 3.65; 95% confidence interval [CI], 1.28–10.50; P = 0.02), return of spontaneous circulation before arrival at the hospital (odds ratio, 2.68; 95% CI, 1.62–4.42; P < 0.001), and 30-day survival (odds ratio, 2.90; 95% CI, 1.30–6.45; P = 0.009). However, physician-staffed ambulances were not associated with patient prognoses in shockable rhythm patients.
Conclusion
Despite our study's limitations, physician-staffed ambulances might be associated with good neurological outcomes in non-shockable rhythm patients. Our observations could provide more appropriate prehospital treatment options for OHCA patients.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a major public health problem.1-3 Although various attempts have been made to alleviate this problem, previous systematic reviews and meta-analyses have reported that the survival rate of OHCA has been unaffected in almost 30 years.4-6 The importance of first-monitored rhythms has been associated with patients’ prognoses.4, 7 For instance, immediate defibrillation has been shown to improve prognoses in OHCA patients.1, 8 However, this procedure has only been adopted for shockable rhythms. In non-shockable rhythms, physical examination, diagnosis, and medication are necessary. Moreover, non-shockable rhythm OHCA patients have been reported to outnumber shockable rhythm patients.7 Therefore, if non-shockable rhythm patients’ prognoses were improved, total OHCA patients’ prognoses might also be improved.
According to previous studies, physician-staffed ambulances have improved the prognoses of OHCA patients.9, 10 The major advantage of physician-staffed ambulances is that a physician can exam and surmise the cause of OHCA earlier than emergency medical service (EMS) personnel. Furthermore, various medications, better team management, and more on-hand personnel could provide better resuscitation efforts for OHCA patients. However, advanced life support, which includes advanced airway management and adrenaline (epinephrine) administration frequently carried out by physicians, has been reported to have worsened the prognoses of OHCA patients.11, 12 Despite the clinical and public health importance of OHCAs, there has been a dearth of research investigating the relationship between physician-staffed ambulances and prognoses after OHCA with respect to first-monitored rhythm differences. Moreover, this type of ambulance service is only available in a limited number of countries.
Hence, we aim to examine retrospectively whether physician-staffed ambulances can be associated with prognoses of OHCA patients with respect to first-monitored rhythm differences in order to establish when these ambulances will be the most beneficial and, ultimately, to improve patient outcomes.
Methods
Study design
This observational study was based on retrospectively collected data in a southern area (population, ~335,000; area, ~200 km2) of Shiga Prefecture, Japan. Data of consecutive OHCA patients from 1 September 2011 to 31 December 2015 were included for the analysis. We excluded patients aged less than 18 years, those whose cardiac arrests were caused by trauma, and those for whom information was missing for the studied variables.
The institutional ethics committee of Saiseikai Shiga Hospital (Shiga, Japan) approved this study (No. 280), and the protocol conformed to the provisions of the Declaration of Helsinki. The requirement for written informed consent was waived.
Emergency medical services system in Japan
Japan has approximately 800 fire stations with dispatch centers, and the EMS system is operated through local fire stations. Generally, three EMS staff members are assigned to an ambulance, and all EMS personnel are able to provide cardiopulmonary resuscitation (CPR) for basic life support and have been trained to use semiautomatic external defibrillators and airway devices. At least one emergency life-saving technician is assigned to each ambulance. Technicians are allowed to provide extensive resuscitation care, for example, they can give adrenaline through venous infusion lines and use advanced airway management, including intratracheal intubation under the guidance of a physician by telephone. The EMS personnel in Japan are not allowed legally to terminate resuscitation in the field. Therefore, most OHCA patients receiving CPR by EMS personnel are transported to hospitals, with the exception of fatality cases.
Physician-staffed ambulance system in the study area
Physician-staffed ambulances were available in the study area of Shiga Prefecture, where two hospitals provide physician-staffed ambulance services. The first hospital initiated a physician-staffed ambulance system in September 2011, and the second in April 2015; systems were both hospital-based. If ambulances were called for cases of OHCA, EMS ambulances were dispatched, and emergency call centers requested physician-staffed ambulances. Physician-staffed ambulances departed from the respective hospital. The staff of a physician-staffed ambulance consisted of four people, including an emergency physician, two medical staff members (primarily nurses), and a driver (usually a non-medical staff member). All physicians had worked in an emergency department for at least 3 years. They supplied advanced cardiac life support, intubation, and medications; however, on-scene percutaneous cardiopulmonary support devices were not used. Physician-staffed ambulances were available from 08:30 to 17:00 on weekdays in addition to EMS ambulances and dispatched for all OHCA. At other times, only EMS ambulances were dispatched for OHCA.
Data collection and quality control
All the data, which were based on the Utstein-style guidelines,13, 14 were collected retrospectively. The EMS personnel recorded the data of OHCA patients under the guidance of a physician. If the data form was incomplete, we supplied as much of the missing data as possible through EMS and medical records.
The data were categorized as follows: age, sex, first-monitored rhythm, witness presence, bystander CPR, time from call to arrival at the scene, out-of-hospital adrenaline administration, out-of-hospital intubation, return of spontaneous circulation (ROSC) before arrival at the hospital, survival and neurological outcomes 30 days after OHCA, and cerebral performance category (CPC).5 The first-monitored rhythm was defined as the rhythm first identified following arrival of the EMS ambulances or physician-staffed ambulances, whichever arrived first at the scene. We divided first-monitored rhythms into two groups: shockable (ventricular fibrillation or pulseless ventricular tachycardia) and non-shockable (pulseless electrical activity or asystole). Bystander CPR included chest compression and rescue breathing; however, its effectiveness was not taken into consideration. Time from call to arrival at the scene was defined as the time lapse between the time at which ambulances were called due to OHCA to the time that the first ambulance, whether it was EMS or physician-staffed, arrived at the scene.
A patient's neurologic outcome 30 days after OHCA was categorized by CPC as follows: 1, good cerebral performance; 2, moderate cerebral disability; 3, severe cerebral disability; 4, coma or vegetative state; 5, death.13, 14 We defined good neurological outcomes as CPCs of 1 or 2.1, 13, 14
Patient outcomes
Primary outcome was defined as the neurological outcome 30 days after OHCA in both shockable and non-shockable rhythm patients. Secondary outcome was defined as ROSC before arrival at the hospital and 30-day survival after OHCA in both shockable and non-shockable rhythm patients.
Statistical analysis
Summary statistics were used to compare the characteristics between physician-staffed and EMS ambulances. To determine the association between physician-staffed ambulances and prognoses after OHCA, univariable and multivariable logistic regression analysis was used. Odds ratios and their 95% confidence intervals were calculated. In the multivariable analysis, we adjusted for age, sex, witness presence, bystander CPR, time from call to arrival at the scene, and adrenaline and intubation. These factors were based on clinical validity.15 Furthermore, we undertook subgroup analyses to test interactions between subgroup variables and physician-staffed ambulances in relation to good neurological outcome.
All P-values were two-sided, and P-values of <0.05 were considered statistically significant. All statistical analyses were carried out by using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (version 3.3.1; The R Foundation for Statistical Computing, Vienna, Austria). More precisely, it is a modified version of R commander (version 2.2-5) designed to add statistical functions frequently used in biostatistics.16
Results
From 1 September 2011 to 31 December 2015, there were 980 OHCA patients. Of these, we excluded 17 patients <18 years of age, 74 patients whose arrests were caused by trauma, and two patients meeting both criteria. Furthermore, we excluded five patients without information regarding their first-monitored rhythm (three patients), CPC (one patient), and adrenaline administration (one patient). Therefore, 882 patients were included in this study (Fig. 1). There were 164 physician-staffed ambulances, nine (5.5%) of which arrived at the scene earlier than EMS ambulances.
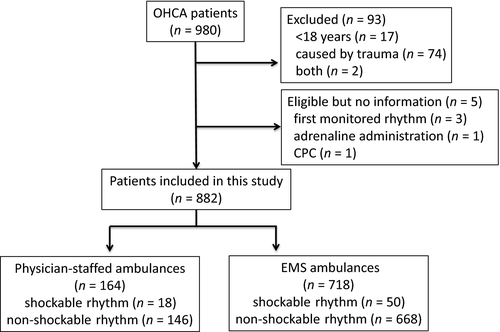
Table 1 shows the characteristics of the OHCA patients (both shockable and non-shockable rhythm patients) who were treated by physician-staffed or EMS ambulances. Physician-staffed ambulances gave adrenaline and undertook intubation more often than EMS ambulances, before arrival at the hospital. No statistically significant differences were observed in age, sex, shockable rhythm, witness presence, bystander CPR performance, or time from call to arrival at the scene. Among shockable rhythm patients, the number of times that adrenaline was given was higher and out-of-hospital amiodarone was given more frequently in the physician-staffed ambulance group; however, no statistical significance was detected concerning the number of shocks and the rate of percutaneous coronary intervention between the groups (Table S1). In addition, among shockable rhythm patients, all patients underwent attempted defibrillation. Among non-shockable rhythm patients, 38 patients (4.7%) underwent attempted defibrillation.
| Total (n = 882) | Shockable rhythm (n = 68) | Non-shockable rhythm (n = 814) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PhS | EMS | P-value | PhS | EMS | P-value | PhS | EMS | P-value | |
| n = 164 | n = 718 | n = 18 | n = 50 | n = 146 | n = 668 | ||||
| Age, years; median (IQR) | 81.0 (69.8–88.0) | 80.0 (69.0–87.0) | 0.500 | 72.5 (63.0–80.8) | 65.0 (48.0–80.0) | 0.080 | 82.0 (70.3–88.0) | 81.0 (70.0–87.0) | 0.480 |
| Sex (male), n (%) | 82 (50.0) | 397 (55.3) | 0.230 | 8 (44.4) | 45 (90.0) | <0.001 | 74 (50.7) | 352 (52.7) | 0.720 |
| Shockable rhythm, n (%) | 18 (11.0) | 50 (7.0) | 0.100 | – | – | – | – | – | – |
| Witness presence, n (%) | 64 (39.0) | 277 (38.5) | 0.930 | 13 (72.2) | 39 (78.0) | 0.750 | 51 (34.9) | 238 (35.6) | 0.920 |
| Bystander CPR, n (%) | 74 (45.1) | 331 (46.0) | 0.860 | 8 (44.4) | 21 (42.0) | 1.000 | 66 (45.2) | 310 (46.4) | 0.860 |
| Time from call to arrival at the scene, min; median (IQR) | 7.0 (6.0–9.0) | 8.0 (6.0–9.0) | 0.080 | 7.0 (5.3–9.8) | 7.5 (6.0–9.0) | 0.750 | 7.0 (6.0–9.0) | 8.0 (6.0–9.0) | 0.100 |
| Out-of-hospital adrenaline, n (%) | 86 (52.4) | 152 (21.2) | <0.001 | 14 (77.8) | 21 (42.0) | 0.010 | 72 (49.3) | 131 (19.6) | <0.001 |
| Out-of-hospital intubation, n (%) | 62 (37.8) | 99 (13.8) | <0.001 | 13 (72.2) | 3 (6.0) | <0.001 | 49 (33.6) | 96 (14.4) | <0.001 |
- CPR, cardiopulmonary resuscitation; IQR, interquartile range.
Table 2 shows good neurological outcome prognoses. Physician-staffed ambulances were associated with good neurological outcome in total patients and non-shockable rhythm patients. In shockable rhythm patients, although we controlled for confounding factors, including the use of amiodarone and percutaneous coronary intervention, to undertake the multivariable logistic regression analysis for good neurological outcome, physician-staffed ambulances were not associated with good neurological outcome (Table S2).
| Total | Shockable rhythm | Non-shockable rhythm | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable analysis | Multivariable analysis | Univariable analysis | Multivariable analysis | Univariable analysis | Multivariable analysis | |||||||||||||
| OR | 95% CI | P-value | aOR | 95% CI | P-value | OR | 95% CI | P-value | aOR | 95% CI | P-value | OR | 95% CI | P-value | aOR | 95% CI | P-value | |
| PhS | 1.45 | 0.74–2.86 | 0.280 | 2.670 | 1.20–5.93 | 0.020 | 0.63 | 0.19–2.04 | 0.440 | 2.28 | 0.20–25.7 | 0.510 | 1.82 | 0.75–4.44 | 0.190 | 3.65 | 1.28–10.50 | 0.020 |
| Age | 0.96 | 0.94–0.97 | <0.001 | 0.94 | 0.90–0.98 | 0.008 | 0.98 | 0.95–1.00 | 0.080 | |||||||||
| Sex (M/F) | 1.23 | 0.62–2.41 | 0.550 | 0.41 | 0.07–2.44 | 0.330 | 1.09 | 0.45–2.62 | 0.850 | |||||||||
| Witness presence | 18.80 | 7.53–49.60 | <0.001 | 1.21 | 0.20–7.42 | 0.830 | 22.70 | 6.45–79.90 | <0.001 | |||||||||
| Bystander CPR | 0.90 | 0.46–1.77 | 0.800 | 1.40 | 0.39–5.00 | 0.600 | 0.53 | 0.20–1.44 | 0.210 | |||||||||
| Time from call to arrival at the scene | 0.81 | 0.70–0.95 | 0.009 | 0.87 | 0.65–1.17 | 0.360 | 0.74 | 0.59–0.93 | 0.010 | |||||||||
| Out-of-hospital adrenaline | 0.21 | 0.09–0.49 | <0.001 | 0.09 | 0.02–0.43 | 0.002 | 0.15 | 0.04–0.60 | 0.005 | |||||||||
| Out-of-hospital intubation | 0.76 | 0.28–2.04 | 0.580 | 0.57 | 0.06–5.93 | 0.640 | 0.48 | 0.10–2.26 | 0.360 | |||||||||
- aOR, adjusted odds ratio; CI, confidence interval; CPR, cardiopulmonary resuscitation; F, female; M, male; OR, odds ratio.
Table 3 shows ROSC before arrival at the hospital and 30-day survival prognoses. Physician-staffed ambulances were associated with ROSC before arrival at the hospital and 30-day survival in total patients and non-shockable rhythm patients.
| Multivariable analysis of ROSC | Total | Shockable rhythm | Non-shockable rhythm | ||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value | |
| Physician-staffed ambulances | 2.62 | 1.65–4.18 | <0.001 | 2.22 | 0.28–17.5 | 0.45 | 2.68 | 1.62–4.42 | <0.001 |
| Age | 0.98 | 0.97–1.00 | 0.010 | 0.97 | 0.94–1.01 | 0.11 | 0.99 | 0.98–1.01 | 0.23 |
| Sex (M/F) | 0.70 | 0.47–1.04 | 0.070 | 0.65 | 0.15–2.80 | 0.56 | 0.62 | 0.40–0.97 | 0.03 |
| Witness presence | 3.81 | 2.52–5.75 | <0.001 | 1.9 | 0.43–8.36 | 0.40 | 3.34 | 2.13–5.24 | <0.001 |
| Bystander CPR | 1.06 | 0.71–1.56 | 0.780 | 1.12 | 0.37–3.42 | 0.84 | 1.00 | 0.65–1.55 | 0.98 |
| Time from call to arrival at the scene | 0.96 | 0.88–1.04 | 0.320 | 1.00 | 0.79–1.26 | 0.98 | 0.95 | 0.86–1.04 | 0.25 |
| Out-of-hospital adrenaline | 1.75 | 1.14–2.67 | 0.010 | 0.20 | 0.06–0.72 | 0.01 | 2.46 | 1.54–3.93 | <0.001 |
| Out-of-hospital intubation | 0.56 | 0.32–0.97 | 0.040 | 1.51 | 0.21–10.80 | 0.69 | 0.43 | 0.23–0.81 | 0.009 |
| Multivariable analysis of 30-day survival | aOR | 95% CI | P-value | aOR | 95% CI | P-value | aOR | 95% CI | P-value |
|---|---|---|---|---|---|---|---|---|---|
| Physician-staffed ambulances | 2.57 | 1.32–5.03 | 0.006 | 2.75 | 0.31–24.2 | 0.36 | 2.90 | 1.30–6.45 | 0.009 |
| Age | 0.96 | 0.95–0.98 | <0.001 | 0.95 | 0.91–0.99 | 0.01 | 0.97 | 0.95–0.99 | 0.009 |
| Sex (M/F) | 1.00 | 0.57–1.76 | 1.000 | 0.74 | 0.15–3.68 | 0.71 | 0.83 | 0.42–1.63 | 0.590 |
| Witness presence | 14.9 | 7.20–30.80 | <0.001 | 1.12 | 0.23–5.35 | 0.89 | 16.80 | 7.52–47.2 | <0.001 |
| Bystander CPR | 1.01 | 0.57–1.77 | 0.980 | 0.91 | 0.28–2.96 | 0.88 | 0.94 | 0.46–1.90 | 0.850 |
| Time from call to arrival at the scene | 0.84 | 0.74–0.96 | 0.009 | 0.95 | 0.73–1.23 | 0.71 | 0.79 | 0.67–0.93 | 0.005 |
| Out-of-hospital adrenaline | 0.39 | 0.20–0.74 | 0.004 | 0.18 | 0.05–0.66 | 0.01 | 0.38 | 0.17–0.89 | 0.020 |
| Out-of-hospital intubation | 0.67 | 0.30–1.53 | 0.350 | 0.63 | 0.08–5.03 | 0.66 | 0.45 | 0.15–1.40 | 0.170 |
- aOR, adjusted odds ratio; CI, confidence interval; CPR, cardiopulmonary resuscitation; F, female; M, male.
Figure 2 shows the subgroup analysis between subgroup variables and physician-staffed ambulances for good neurological outcome in shockable rhythm patients. There was no interaction among subgroup variables. Because good neurological outcome was not observed in the physician-staffed ambulance group that experienced unwitnessed OHCA, the odds ratio and P-value for interaction for the unwitnessed group could not be calculated.
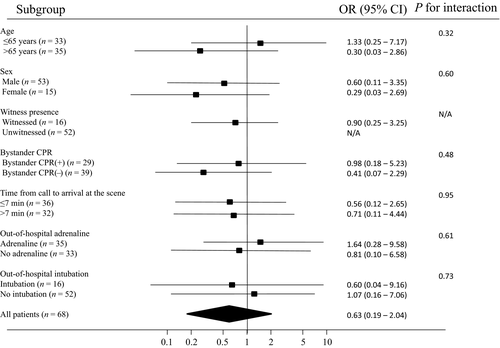
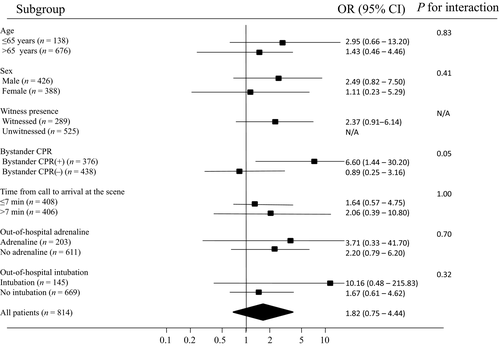
Figure 3 shows the subgroup analysis between subgroup variables and physician-staffed ambulances for good neurological outcome in non-shockable rhythm patients. Bystander CPR had a statistically significant association with good neurological outcome. Because good neurological outcome was not observed in the physician-staffed ambulance group that experienced unwitnessed OHCA, the odds ratio and P-value for interaction for the unwitnessed group could not be calculated.
Discussion
In this retrospective study of 882 OHCA patients, we made several important observations. Physician-staffed ambulances were not associated with good neurological prognoses, ROSC, or 30-day survival in OHCA patients whose initial rhythm was shockable. In contrast, these ambulances significantly improved the rate of good neurological outcomes, ROSC, and 30-day survival in OHCA patients who initially had non-shockable rhythms. In addition, in non-shockable rhythm bystander CPR patients, physician-staffed ambulances were associated with good neurological outcomes.
Several reasons were possible for the fact that physician-staffed ambulances were not associated with the prognoses of shockable patients in this study. First, it is well known that immediate defibrillation is the most precise factor for predicting favorable prognoses for OHCA patients. Second, although there is an advantage in having a physician's knowledge of anti-arrhythmia medications, the effects of such drugs on OHCA patients were not established. Third, on-scene percutaneous cardiopulmonary support devices were not used, which might have given a powerful advantage to physician-staffed ambulances.
In non-shockable rhythm patients, physician-staffed ambulances were positively associated with good neurological outcomes, ROSC, and 30-day survival. One previous study reported a relationship between physician-staffed ambulances and ROSC and 30-day survival,10 which mirrors the results of our study. However, that study did not investigate the relationship between physician-staffed ambulances and prognoses after OHCA with respect to first-monitored rhythm differences. Furthermore, physician-staffed ambulances were associated with good neurological outcomes in non-shockable rhythm patients. One reason for this could be that the early adrenaline administration and endotracheal intubation might contribute to an elevated rate of good neurological outcomes, ROSC, and 30-day survival in non-shockable rhythm patients. Although some studies have reported that these procedures were less effective in providing good neurological prognoses,11, 12 two recent studies have shown that early performance of these procedures was useful in non-shockable rhythm patients.17, 18 In physician-staffed ambulances, the use of adrenaline and endotracheal intubation might be initiated earlier than in EMS ambulances.
In the subgroup analysis, bystander CPR had a statistically significant association between physician-staffed ambulances and good neurological outcome in non-shockable rhythm patients. In this study, bystander CPR effectiveness was not taken into consideration; however, it might be possible that, if physician-staffed ambulances could select non-shockable rhythm and bystander CPR patients, these ambulances could be more effective.
Although it could be advantageous that physicians can examine and surmise the cause of OHCA earlier in non-shockable rhythm patients, our study was unable to show that physicians’ assistance in these cases was necessary. Early use of adrenaline and endotracheal intubation could be useful; therefore, if EMS ambulances could undertake these procedures early, there might be no difference in outcomes between the ambulance types. Therefore, it could be difficult to show that physicians’ knowledge and experience were necessarily beneficial. However, further well-designed prospective investigations are needed to make this determination.
Our study showed that physician-staffed ambulances might be associated with good neurological outcomes in non-shockable rhythm patients. It might be possible that, if physician-staffed ambulances could select non-shockable rhythm and bystander CPR patients, these ambulances could be more effective. However, in shockable rhythm patients, these ambulances might not be associated with patients’ prognoses.
To the best of our knowledge, this is the first report showing the impact of physician-staffed ambulances on OHCA patients classified by their first-monitored rhythm. Therefore, our results could identify the cases for which physician-staffed ambulances would be the most useful.
Limitations
Our study had several potential limitations. First, it was a retrospective observational study undertaken in a specific area, thereby limiting data selection. Second, in this study, physician-staffed ambulances were only dispatched in the daytime, on weekdays. It has been reported that the time of OHCA (weekdays, holidays, daytime, and night-time) was associated with patients’ prognoses,19, 20 a factor which was not accounted for in this study. Third, a lack of data might have influenced the results of this study. For example, mechanical chest compression,21 complicating disease processes, differing locations where the OHCA occurred, differing abilities of EMS personnel, and in-hospital procedures performed (e.g., treatment for hypothermia and use of percutaneous cardiopulmonary support devices) were not collected. In addition, we were unable to discern whether or not bystander CPR was effective. Fourth, while physician-staffed ambulances transported OHCA patients to the nearest hospital, there was transportation bias. Ambulance personnel selected the destination hospital depending on the condition of OHCA patients, as there was a difference in treatment that could be carried out at each hospital. Finally, because our study was confined to a restricted area in Japan, outcomes cannot be generalized to other countries with different physician-staffed ambulances and EMS systems.
Conclusions
Despite our study's limitations, our results suggest that, in shockable rhythm patients, physician-staffed ambulances might not be associated with their prognoses. However, in patients with non-shockable rhythm, these ambulances might be associated with good neurological outcomes. Our observations could influence future staffing requirements in ambulances and, in turn, provide more appropriate prehospital treatment options for OHCA patients.
Acknowledgements
The authors appreciate the contributions of Shino Hiraizumi, M.D., Masahiro Nozawa, M.D., and Tadashi Echigo, M.D. from the Saiseikai Shiga Hospital, Takayuki Kato, M.D. from the Shiga University of Medical Science, Shinsaku Takeda, M.D. from the Shiga General Hospital and Hiroshi Tsuruta, M.D., Ph.D. from the Kusatsu General Hospital who collected clinical data. We would like to thank Professor Takashi Omori, Ph.D. from the University of Kobe for useful statistical advice. In addition, we would like to thank the members of the Konan Fire Department for their participation in the study.
Disclosure
Approval of the research protocol: The institutional ethics committee of Saiseikai Shiga Hospital (Shiga, Japan) approved this study (No. 280).
Informed consent: N/A.
Registry and registration no. of the study/trial: N/A.
Animal studies: N/A.
Conflict of interest: None declared.