A retrospective study of in-hospital cardiac arrest
Abstract
Aim
In-hospital cardiac arrest is an important issue in health care today. Data regarding in-hospital cardiac arrest in Japan is limited. In Australia and the USA, the Rapid Response System has been implemented in many institutions and data regarding in-hospital cardiac arrest are collected to evaluate the efficacy of the Rapid Response System. This is a multicenter retrospective survey of in-hospital cardiac arrest, providing data before implementing a Rapid Response System.
Methods
Ten institutions planning to introduce a Rapid Response System were recruited to collect in-hospital cardiac arrest data. The Institutional Review Board at each participating institution approved this study. Data for patients admitted at each institution from April 1, 2011 until March 31, 2012 were extracted using the three keywords “closed-chest compression”, “epinephrine”, and “defibrillation”. Patients under 18 years old, or who suffered cardiac arrest in the emergency room or the intensive care unit were excluded.
Results
A total of 228 patients in 10 institutions were identified. The average age was 73 ± 13 years. Males represented 64% of the patients (82/146). Overall survival after in-hospital cardiac arrest was 7% (16/228). Possibly preventable cardiac arrests represented 15% (33/228) of patients, with medical safety issues identified in 8% (19/228). Vital sign abnormalities before cardiac arrest were observed in 63% (138/216) of patients.
Conclusions
Approximately 60% of patients had abnormal vital signs before cardiac arrest. These patients may have an improved clinical outcome by implementing a Rapid Response System.
Introduction
Two decades have passed since the medical emergency team was first instituted in Australia.1 In the USA, the Institute of Medicine reported that at least 44,000 people, and perhaps as many as 98,000 people, die in hospitals each year as a result of medical errors that could be prevented.2
Rapid Response Systems (RRS) are patient-focused systems developed to prevent potentially avoidable deaths and serious adverse events such as cardiac arrests. The RRS identifies seriously ill and at-risk patients and those whose condition is deteriorating, allowing physicians to intervene appropriately in a timely manner. In Australia and the USA, the RRS has been implemented in many institutions and has contributed to improved clinical outcomes.3-6 In Japan, the Kyodokodo (medical safety nationwide joint action) has endorsed and promoted the RRS. Thus, recognition and implementation of RRS are gradually spreading.
In recent years, evidence regarding the details of out-of-hospital cardiac arrest has accumulated, enabling the establishment of evidence-based guidelines.7, 8 In European countries and the USA, multicenter in-hospital cardiac arrest (IHCA) registries have been developed and have reported results.9-13 However, there are limited data regarding IHCA in Japan. To date, only Yokoyama et al. have reported a prospective multicenter observational registry of IHCA at 12 facilities in Japan.14 This study included many facilities specializing in cardiovascular diseases, which may not reflect typical practice in Japan. We undertook a multicenter survey regarding IHCA to obtain baseline data prior to implementing a RRS. We examined the patient demographics of patients suffering IHCA, and evaluated associated in-hospital mortality. In addition, we reviewed the proportion of patients with IHCA who had abnormal vital signs preceding the IHCA.
Methods
Design and setting
A retrospective multicenter review of IHCA was carried out in 10 institutions. This study was approved by the Ethics Committee of St. Marianna University School of Medicine (Kanagawa, Japan) as the lead facility, and approved by the institutional review boards at each participating institution. Individual informed consent was waived by all participating institutions.
Data source
Diagnosis procedure combination data is a casemix patient classification system, similar to diagnosis-related groups in use in the USA. During a period of 1 year (from April 1, 2011 to March 31, 2012), all patients who suffered an IHCA, for whom cardiopulmonary resuscitation was performed, were evaluated retrospectively. Data were extracted based on three keywords in the diagnosis procedure combination records: “closed-chest compression”, “epinephrine”, or “defibrillation”. Patients under 18 years old, or those who had a cardiac arrest in the emergency room or intensive care unit (ICU) were excluded.
Data collection
The following data were collected for each case identified: age, gender, admitting service, event site, event time, code activation pattern, initial electrocardiogram wave pattern, defibrillation attempt times, monitor attached time, defibrillation time, primary disease for admission, etiology of cardiac arrest, and presence of vital sign abnormalities before the cardiac arrest. Criteria from a previous study were used to collect abnormal vital signs as a reference.15 Data collection and statistical analysis were carried out using StatFlex V6.0 (Artech Co., Ltd, Osaka, Japan).
Definition of each term was decided a priori
Futile care was defined as treatment when the purpose does not benefit patient care.16 A possibly preventable cardiac arrest was defined as a patient with a clear link between suboptimal practice and the event.17 A medical safety issue was defined as any unintended or unexpected incident that could harm a patient. Data were reviewed by an Emergency Medicine Board-Certified physician and a member of the medical safety committee at each facility. If the judgment was not in agreement, a third Emergency Medicine Board-Certified physician made the final decision in each facility.
Results
Details of study hospitals and patient cohort
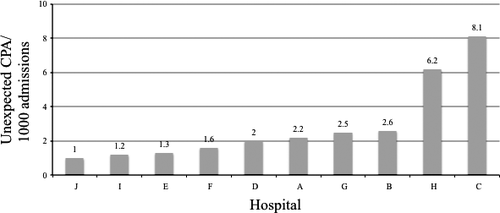
Data for a total of 228 patients were reviewed. The mean number of beds in the 10 participating institutions was 561 (range, 282–1,063). The number of unexpected cardiac arrests per 1,000 admissions at each facility is shown in Figure 1. The mean age of the patients was 72 ± 12 years and 64% (146/228) were men. The proportion of “code blue” activations during the cardiac arrests was 20% (45/228).
Details of cardiac arrests
Only 7% (16/228) of patients survived until discharge. Cardiac diseases were responsible for 21% of admissions (49/228) and non-cardiac diseases represented 79% (179/228) (Table 1). Witnessed cardiac arrest occurred in 58% (132/228) of patients, and 51% (116/228) had electrocardiogram monitoring at the time of cardiac arrest (Table 2. After cardiac arrest, 15% (36/228) of patients were considered to have a cardiac rhythm on the electrocardiogram that may respond to defibrillation (ventricular fibrillation/pulseless ventricular tachycardia), 32% (74/228) had pulseless electrical activity, and 22% (50/228) had asystole (Table 2).
| Etiology | Number | Percent (%) |
|---|---|---|
| Cardiac | n = 49 | 21 |
| Non-cardiac | n = 179 | 79 |
| Detailed etiology for non-cardiac | Total 179 | |
| Infectious | 51 | 22 |
| Oncology | 36 | 16 |
| Surgical | 23 | 10 |
| Gastrointestinal | 15 | 7 |
| Terminal | 10 | 4 |
| Neurological | 9 | 4 |
| Other | 35 | 15 |
| Situation | Percentage (number/total) |
|---|---|
| Witnessed | 58% (132/228) |
| Monitored | 51% (116/228) |
| Initial rhythm | |
| Ventricular fibrillation | 7% (17/228) |
| Ventricular tachycardia | 8% (19/228) |
| Pulseless electrical activity | 32% (74/228) |
| Asystole | 22% (50/228) |
| Other | 5% (11/228) |
| Unknown | 25% (57/228) |
| 100% | |
Presence of “do not attempt resuscitation” orders, “futile care”, “possibly preventable cardiac arrest”, and “medical safety issue”
Eleven percent (26/228) of patients had an active “do not attempt to resuscitate” order and 12% (27/228) of patients were regarded as receiving medically futile care. Cardiac arrests were considered as preventable in 15% (33/228) of patients, and 7% (19/228) of cardiac arrest causes were related to medical safety issues (Table 3).
| Percentage | ||
|---|---|---|
| Possible preventable cardiac arrests | 15% (33/228) | |
| Incidents or accidents | 8% (19/228) | |
| Preceding symptom | 21% (7/33) | |
| Inappropriate monitoring | 24% (8/33) | |
| Medical safety issue | Error: treatment | 27% (9/33) |
| Error: preventive measures | 12% (4/33) | |
| Error in judgment | 12% (4/33) | |
| Total | 100% (n = 33) | |
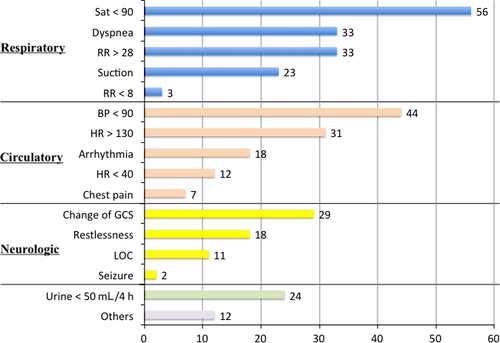
Presence of antecedent vital sign abnormalities
Vital sign abnormalities were identified in the 24 h preceding the cardiac arrest in 61% (140/228) of patients (Fig. 2). The most common abnormalities were associated with respiratory function, such as persistent SpO2 <90%, dyspnea, or tachypnea (respiratory rate >28). The second most common abnormalities were associated with circulation including systolic blood pressure <90 mmHg or tachycardia (heart rate >130). In the 6 h preceding cardiac arrest, the most frequent abnormalities observed were associated with altered respiratory function (Table 4).
| Time period (IQR hours) | T ≤ 6 (%) | 6 < T ≤ 12 (%) | 12 < T ≤ 18 (%) | 18 < T ≤ 24 (%) | Hours (%) |
|---|---|---|---|---|---|
| Respiratory (1–15) | 18 | 10 | 4 | 14 | 45 |
| Circulatory (1–16) | 11 | 5 | 3 | 12 | 31 |
| Neurologic (1–13) | 5 | 2 | 2 | 6 | 14 |
| Renal (11–24) | 2 | 1 | 1 | 3 | 8 |
| Others (6–10) | 1 | 1 | 0 | 0 | 3 |
| 37 | 19 | 9 | 35 | 100 |
- CA, cardiac arrest; IQR, interquartile range.
- Respiratory: saturation <90%, dyspnea, respiratory rate >28/min, <8/min.
- Circulatory: systolic blood pressure <90 mmHg, heart rate >130/min, <40/min, chest pain.
- Neurologic: change of glasgow coma scale, loss of consciousness, seizure.
- Renal: urine <50 ml/4 hr.
Discussion
The incidence of IHCA (Fig. 1) at each facility ranged from 1.0 to 8.1 per 1,000 admissions. This study found a similar incidence (from 3.8 to 13.1 per 1,000 admissions) of IHCA compared to reports from England and the USA.17, 18 Given the lack of consistency in reporting the incidence of IHCA, outcomes should be reviewed and compared with caution.19 At present, eight of the 10 hospitals in this study have introduced RRS.
The patient population in this study included patients who had IHCA in a general ward. Approximately 60% of patients had abnormal vital signs before suffering a cardiac arrest. There have been similar reports reported from England and the USA. Schein et al.20 found that 84% of the patients had documented clinical deterioration, and Franklin et al.21 reported a comparable number of 66%. However, previous studies have reported incompletely recorded vital signs.22, 23 The respiratory rate was often omitted from data collection, and has been termed the “neglected vital sign”.24 Vital signs may not have been documented for a number of reasons, and requires further study. The retrospective nature of this study may influence these results as well. This is the first retrospective report of a multicenter study of IHCA, including non-cardiovascular facilities, in Japan.
The physiological abnormalities preceding cardiac arrest (Fig. 2) affected the fundamental functions of airway, breathing, and circulation.25 Percutaneous arterial oxygen saturation was less than 90%, which was the most common antecedent factor, and hypotension was the second most common factor. These results identify a group of at-risk individuals who may represent preventable cardiac arrests, despite suffering IHCA.26 Some facilities have recently introduced the Early Warning Score system or the National Warning Score system, and used these systems to identify patients who are physiologically deteriorating.27, 28 In the present study, in the 6 h preceding cardiac arrest, the most frequent physiologic abnormalities were associated with respiratory function. These results are similar to those previously reported.20
In this study, only 7% of patients survived until hospital discharge, which is quite low. Yokoyama et al. 14 reported a 30-day survival rate of 28% and Girotra et al. 12 reported survival until hospital discharge in 17% of patients. Those studies included patients who had IHCA in the ICU, which makes it difficult to compare with results of the present study. Another possible explanation of the higher rate of in-hospital mortality in this study might be related to the indications for admission. In this study, cardiac disease was present in 21% of patients, whereas Yokoyama's study included 55% of patients with cardiac disease.14 At the time of initial electrocardiogram after IHCA, rhythms that may respond to defibrillation (ventricular fibrillation/pulseless ventricular tachycardia) were present in 15% of patients in this study; 41% of patients in Yokoyama's study had these cardiac rhythms.14 The higher rate of hospital mortality may be associated with a low proportion of cardiac rhythms that generally respond to electric shock. The aging of Japan's population is advancing. Even if a patient has a cardiac rhythm that responds to electric shock, they might not survive because of advanced age. These factors may influence the overall rate of hospital mortality.
The management of IHCA is affected by specific aspects of the medical care system in each country. Before trying to predict the effectiveness of introducing an RRS in a particular country, data is essential to be able to compare clinical outcomes before and after RRS implementation. This study was carried out to provide such data in Japan. This study also illustrates specific features of the Japanese medical culture. The code team was activated for only 20% of patients. In Japan, nursing staff contact the attending physician or accessible physician when a patient suffers a cardiac arrest, and it is generally expected that this physician will coordinate the resuscitation effort. Even in patients with “do not attempt resuscitation” status, cardiopulmonary resuscitation was occasionally carried out. Life-sustaining support for critically ill patients, regardless of the futility of care, was given until recently in Japan.29, 30 A patient with “do not attempt resuscitation” status may be given full support despite cardiopulmonary arrest, which occurred in 11% of the patients in this study. This shows that cardiopulmonary resuscitation was carried out even in patients with a “do not attempt resuscitation” order, and that the order may have been overridden because of legal concerns, or concerns about relationships with the family.
Limitations
This study has some limitations. The specific level and quality of care is variable among the facilities that participated in this study. We could not classify the “response style” between institutions. It is not possible to provide survival analyses for each of the initial rhythm types and the details of treatment in medically futile cases. The “do not attempt resuscitation” policy and ICU admission criteria were not the same in all facilities. As this is a retrospective review, some relevant data, especially vital sign information, may not have been recorded or were not available in patient records. Other limitations may include missing capture of data due to study design, and a lack of assessment of interobserver agreement for measures related to subjective assessment, such as “futile care”, “possibly preventable death” and “medical safety issue”.
Conclusions
In this study, approximately 60% of patients had abnormal vital signs before cardiac arrest. These patients may have had improved clinical outcomes with intervention by an RRS. The RRS data with IHCA data should be prospectively collected for in-hospital medical safety and risk management.
Conflicts of interest
None.
Acknowledgements
This study was supported by MEXT KAKENHI (Grant Number 24592755).
Appendix
The members of the In-Hospital Cardiac Arrest Study Group were: Takeshi Ikeda (Aizawa Hospital, Nagano), Yuka Takamatsu (St. Marianna University Hospital), Yasuhisa Hasegawa (Aichi Cancer Center Hospital), Satoshi Suzuki (Aomori Kensei Hospital), Tetsya Komuro (Saitama Medical Center), Natsuki Kawamura (JA Hiroshima General Hospital), and Narumi Yamada (NHO Nagasaki Medical Center).