Olprinone, phosphodiesterase III inhibitor, is useful for patients with severe acute heart failure due to takotsubo cardiomyopathy accompanied by subarachnoid hemorrhage
Abstract
Case
A 53-year-old woman with coma was diagnosed with subarachnoid hemorrhage and ruptured aneurysm at the right internal carotid–posterior communicating artery.
Outcome
The aneurysm was successfully clipped. Severe hypoxia and shock with abnormal left ventricular contraction were observed. We diagnosed severe acute heart failure with cardiogenic shock due to takotsubo cardiomyopathy complicated by subarachnoid hemorrhage. Neither catecholamine nor intra-aortic balloon pumping was selected to treat severe acute heart failure with cardiogenic shock because catecholamine generally worsens takotsubo cardiomyopathy and hematoma after surgery. Therefore, we gave olprinone and improved hypoxia and hemodynamics immediately without any arrhythmia.
Conclusion
Olprinone was effective for severe acute heart failure with cardiogenic shock due to takotsubo cardiomyopathy accompanied by subarachnoid hemorrhage. Catecholamine agents should be avoided if possible in patients with takotsubo cardiomyopathy. A phosphodiesterase III inhibitor may be useful for cardiogenic shock caused by takotsubo cardiomyopathy.
Introduction
A 53-year-old woman with recent severe headache was transferred to our emergency room because of sudden coma. Blood pressure (BP) was 65/40 mmHg and heart rate was 95 b.p.m. A cerebral computed tomography scan revealed subarachnoid hemorrhage (SAH) (Fig. 1). Angiogram showed a 6 mm ruptured aneurysm at the right internal carotid–posterior communicating artery (Fig. 1). Arterial blood gas analysis showed severe hypoxemia (pO2 = 70 torr; FiO2 = 1.0). Chest X-ray indicated normal-sized heart with severe pulmonary congestion (Fig. 2). Electrocardiogram revealed sinus tachycardia with ST elevation and inverted T wave in V4, V5, and V6 (Fig. 2). Echocardiogram showed akinesis of the apex, as indicated in Figure 2. We diagnosed acute heart failure with cardiogenic shock due to takotsubo cardiomyopathy following SAH (Hunt and Kosnik grade III). Because of severe hypoxia due to severe pulmonary congestion, tracheal intubation and mechanical ventilation with 100% oxygen were needed.
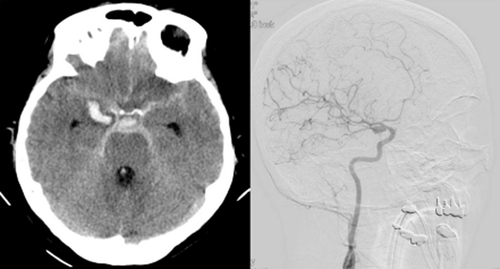
Cerebral computed tomography (left) and angiogram (right) of a 53-year-old woman with sudden coma.

Chest X-ray (left upper), echocardiogram (left bottom), and electrocardiogram (right) of a 53-year-old woman with sudden coma. Chest X-ray shows lung congestion. Echocardiograph shows apical ballooning of left ventricle in systole. Electrocardiogram shows typical giant negative T inversion at day 11, compatible with takotsubo cardiomyopathy.
In the intensive care unit, we detected the following hemodynamic and respiratory parameters: cardiac index (CI) = 1.9 L/min/m2; mean pulmonary arterial wedge pressure (mPAWP) = 22 mmHg; systemic vascular resistance index (SVRI) = 2203 dyne·s/m5/m2; SvO2 = 60%; pO2/FiO2 = 70 mmHg. Pressure study revealed severe heart failure with cardiogenic shock.
Case
For cardiogenic shock, we did not choose intraaortic balloon pumping (IABP) because anticoagulant therapy should be avoided. We also did not use catecholamines, because they should not generally be used in takotsubo cardiomyopathy. Therefore, olprinone, a phosphodiesterase III (PDE III) inhibitor, was selected for the treatment of cardiogenic shock.
Olprinone was infused i.v. at the dose of 0.2 μg/kg/min. One hour after the initiation of olprinone, hemodynamics were substantially improved without any side-effects. Four hours later, olprinone dramatically improved hemodynamics and oxygenation: BP = 102/64 mmHg; heart rate = 106 b.p.m.; CI = 2.6 L/min/m2; mPAWP = 18 mmHg; SVRI = 2143 dyne·s/m5/m2; SvO2 = 78%; pO2/FiO2 = 150 (Fig. 3).

Clinical course of a 53-year-old woman with sudden coma after admission to intensive care. Systolic blood pressure (sBP) increased from 65 to 102 mmHg (upper graph) because the cardiac index (CI) increased from 1.9 to 2.6 L/min/m2 (middle graph) without systemic vascular resistance index decrease (from 2203 to 2143 dyne·s/m5/m2) at 4 h after olprinone (Olp.) infusion. Pulse pressure increased (upper graph) and urine amount increased (bottom graph), which means cardiac performance improvement, resulting in a decrease in mean pulmonary capillary wedge pressure (mPAWP) from 22 to 18 mmHg (middle graph) and pO2/FiO2 (p/f) ratio improvement (from 70 to 150). Taken together, olprinone improved cardiogenic shock and severe heart failure within 4 h of infusion. BP, blood pressure; dBP, diastolic blood pressure; HR, heart rate.
Finally, the aneurysm was successfully clipped. Olprinone was discontinued after 3 days. Intratracheal tube was removed after 5 days. Left ventricular wall motion was normalized after 16 days. The patient was discharged after 26 days without any neurological dysfunction, and is now working as a maternity nurse.
Discussion
Takotsubo cardiomyopathy is characterized by acute left ventricular dysfunction with transient apical ballooning in absence of significant coronary artery disease.1 Typically, this condition is associated with sudden emotional or physical stress, accompanied by catecholamine surge, including SAH.2
Left ventricular abnormalities, including takotsubo cardiomyopathy, occurs in around 8% of cases of SAH in the ultra-early phase after onset.3 Some patients tend to be severe and the condition is often associated with pulmonary lung edema and hemodynamic instability, resulting in cardiogenic shock. In such cases, the management of cardiogenic shock is often very difficult. Catecholamine agents should be avoided whenever possible they have a causative role in the development of this cardiomyopathy.4 Intraaortic balloon pumping normally requires the use of anticoagulant agents, so IABP is difficult to use in patients with SAH.
Therefore, we chose olprinone, a specific PDE III inhibitor developed in Japan and extensively used in the treatment of acute heart failure. Olprinone has positive inotropic actions through the elevation of intracellular cAMP levels in cardiomyocytes.
There are many reports of heart failure due to takotsubo cardiomyopathy being treated with the calcium sensitizer levosimendan, a non-catecholamine inotrope that is not currently available in Japan, but there are few reports of treatment with a PDE III inhibitor. Padayachee reported that levosimendan was used successfully in takotsubo cardiomyopathy-related cardiogenic shock. They discussed that PDE III inhibitors may be problematic as they increase cAMP within cells, worsen myocardial stunning, and cause vasodilation resulting in hypotension.5 We are also concerned that olprinone may worsen hypotension because PDE III inhibitors have a vasodilatory effect. However, it has been reported that low-dose PDE III inhibitors exert a more potent positive inotropic effect and have a lesser effect on systemic vascular resistance than high-dose PDE III inhibitors.6 Consistent with previous report, in our case, low-dose olprinone increased cardiac output and only minimally decreased systemic vascular resistance. Therefore, worsening of hypotension did not occur after low-dose olprinone infusion. We observed hemodynamic stability, such as pulse pressure, SvO2, and increased urine amount, accompanied with a decrease in mPAWP. However, it is necessary to carefully observe changes in CI and SVRI after treatment with low-dose PDE III inhibitor to avoid drug-induced shock.
The exact mechanism of takotsubo cardiomyopathy is still unknown, but disturbance of the calcium regulatory system has been indicated. This effect might be caused by supraphysiological levels of catecholamines, which stimulate β-adrenoreceptors and alter the expressions of calcium-regulatory protein genes. Sarcolipin regulates sarcoplasmic/endoplasmic reticulum calcium ATPase 2 by lowering its affinity for Ca2+, and is frequently overexpressed in stress cardiomyopathy.7 Olprinone may have some effects on this calcium regulatory system.
Conclusion
In our case, olprinone dramatically and safely improved cardiogenic shock without IABP or catecholamine agents. Low-dose olprinone can be one of the most useful therapeutic agents in patients with cardiogenic shock due to takotsubo cardiomyopathy accompanied by SAH.
Conflict of Interest
None.