Medication utilization for patients with chronic rhinosinusitis with nasal polyposis and asthma in 12 months pre- and post-dupilumab initiation
Presented as an oral presentation at the annual meeting of the American Rhinologic Society, September 2023, in Nashville, TN.
Abstract
Key points
- This study examines the impact of dupilumab on medication use for chronic rhinosinusitis with nasal polyposis (CRSwNP) and asthma patients.
- Patients on dupilumab had a reduction in oral/inhaled/topical steroids, antibiotics, and leukotriene receptor antagonists (LTRAs).
- The reduction in medication use had no impact on total polyp or SNOT-22 scores.
1 INTRODUCTION
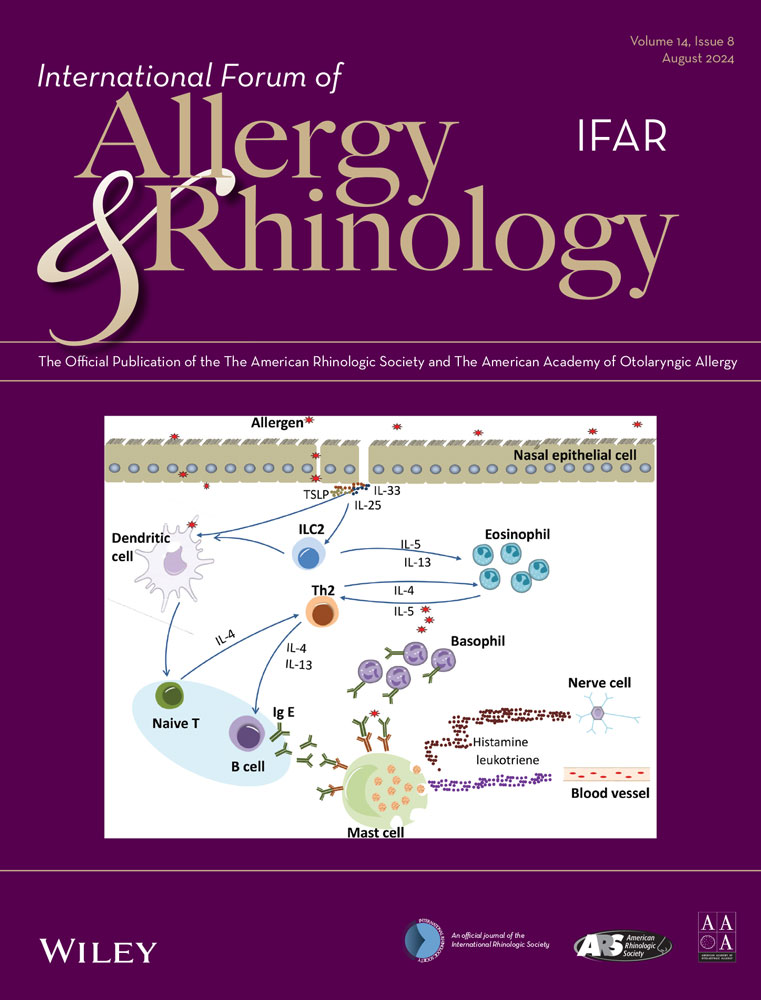
Asthma and chronic rhinosinusitis with nasal polyposis (CRSwNP) are chronic inflammatory diseases of the airway mediated through type 2 inflammation, and patients with both often present with more severe disease.1 Dupilumab treats both through targeting type 2 inflammation, preventing the activation of IL-4 and IL-13. Dupilumab has demonstrated a reduction in asthma and CRSwNP symptoms as well as objective measurements.1 This study examines the impact of dupilumab on topical, oral, and inhaled medications for CRSwNP and asthma patients before and after dupilumab initiation.
2 RESULTS
Thirty-nine patients with CRSwNP and asthma who were followed by otolaryngology and pulmonology 12 months pre- and post-dupilumab initiation were included. While all patients had CRSwNP, two patients started duplimuab for the primary indication of asthma. Demographics and baseline characteristics are summarized in Table 1. Thirty-six (92.31%) patients had a previous endoscopic sinus surgery (ESS) with an average of 1.89 ± 0.99 before enrollment (Table 1). Patients without ESS were started on dupilumab primarily for asthma. Prior to dupilumab, patients had an average polyp score of 4.15 (2.53) (min: 1 max: 8) and Sino-Nasal Outcome Test (SNOT)-22 of 57.34 (22.45) (min: 11, max: 73). There was a significant reduction in polyp and Sino-Nasal Outcome Test (SNOT-22) score after 12 months of dupilumab therapy (Table 1).
| CRSwNP and asthma cohort, mean (min, max) (SD), n = 39 | |
|---|---|
| Age | 52.21 (15.52) |
| Sex | |
| Male | 14 (35.90%) |
| Female | 25 (64.10%) |
| Race | |
| White | 19 (48.70%) |
| Black | 16 (41.0%) |
| Asian | 1 (2.60%) |
| Other | 3 (7.70%) |
| Body Mass Index (BMI) | 30.83 (5.61) |
| Smoking status | |
| Current | 0 (0.00%) |
| Former | 16 (41.03%) |
| Never | 23 (58.97%) |
| Insurance | |
| Private | 15 (38.50%) |
| Medicare | 17 (43.60%) |
| Medicaid | 7 (17.90%) |
| Asperin-Excarbated Respiratory Disease (AERD) | 10 (25.64%) |
| Number of prior surgeries, mean (SD) | 1.89 (0.99) |
| Baseline total polyp score, (SD) | 4.15 (1, 8) (2.53) |
| Baseline SNOT-22, (SD) | 57.34 (11, 73) (22.45) |
| 12 Month total polyp score, (SD) | 0.91 (0, 7) (1.99) |
| 12 Month SNOT-22, (SD) | 24.24 (0, 60) (22.45) |
- Note: Both 12-month total polyp and SNOT-22 scores were significantly reduced compared to baseline measurements at p < 0.001.
Medication consumption 12-month pre- to the 12-month post-biologic initiation using both electronic medical records and clinical notes were compared. After dupilumab initiation, patients had significantly decreased oral steroid prescriptions for both asthma (1.92–0.36) and CRSwNP indications (2.46–1.05) as well as antibiotic prescriptions (3.08–0.85). The cohort also had a decrease in the number of patients on high-dose inhaled corticosteroids (ICS) (17 vs. 12) leukotriene receptor antagonists (LTRA) (27 vs. 16), and nasal steroid spray for CRSwNP and asthma treatment and/or exacerbations. CRSwNP exacerbations were defined as an acute worsening of symptoms with worsening nasal congestion and signs of infection on endoscopy with or without a positive culture. There was no significant difference in topical antibiotic use and nasal steroid rinses (Table 2).
| Cohort baseline |
Cohort 12-month follow up |
Pearson chi square | df | Phi/Cramer's V | p-value | |
|---|---|---|---|---|---|---|
| Nasal steroid sprays | 22 | 8 | 3.956 | 1 | 0.319/0.319 | 0.047 |
| Nasal steroid rinses | 22 | 12 | 0.290 | 1 | −0.086/0.086 | 0.59 |
| LTRA | 27 | 16 | 7.66 | 1 | 0.443/0.443 | 0.006 |
| Topical antibiotics | 4 | 3 | 0.371 | 1 | −0.098/0.098 | 0.542 |
| Inhaled corticosteroids | ||||||
| Low | 7 | 7 | ||||
| Medium | 9 | 8 | 25.15 | 6 | 0.873/0.617 | <0.001 |
| High | 17 | 12 |
| 95% Confidence interval of the difference | ||||||
|---|---|---|---|---|---|---|
| Cohort baseline mean (SD) | Cohort 12-month follow up mean (SD) | Lower | Upper | Cohen's d effect size | Two-sided p-value | |
| CRS steroid prescriptions | 1.92 (2.13) | 0.36 (0.63) | 0.90 | 2.22 | 0.77 | <0.001 |
|
CRS Mg of steroids |
511.67 (623.70) | 91.03 (155.75) | 217.54 | 623.75 | 0.67 | <0.001 |
| Antibiotic prescriptions | 3.08 (2.45) | 0.85 (1.29) | 1.56 | 2.90 | 1.09 | <0.001 |
| Asthma steroid prescriptions | 2.46 (3.03) | 1.05 (1.85) | 0.71 | 2.11 | 0.66 | <0.001 |
|
Asthma Mg of steroids |
800.95 (1284.74) | 393.59 (932.52) | 84.25 | 730.47 | 0.41 | 0.02 |
3 DISCUSSION
CRSwNP and asthma patients represent a distinct population. Patients with both demonstrate predominance of type 2 inflammation and worse nasal and pulmonary symptoms.1 This study demonstrates the efficacy of dupilumab for reducing CRSwNP and asthma medication consumption through decreased oral steroid, nasal steroid sprays, ICS, antibiotic, and LTRA medication use, while maintaining an improvement in total polyp and SNOT-22 scores.
This cohort demonstrated a significant reduction of high-dose ICS as well as oral steroid consumption for CRSwNP and asthma patients. While there is no clear algorithm for deescalating steroid medication, our results demonstrate that clinical judgment is adequate as patients required fewer steroid courses in the follow-up period. Furthermore, it is known that prolonged oral corticosteroid exposure is associated osteoporosis, cardiovascular disease, and diabetes mellitus; however, patients on prolonged (>1 year) high-dose ICS are also subject to similar side effects.2
The European position paper guidelines recommend continued use of intranasal corticosteroids during biologic therapy treatment.3 In the current study's cohort, significantly fewer patients were using intranasal steroid sprays. Therefore, while patients who undergo ESS demonstrate high rates of recurrence without continued medical therapy, patients on dupilumab may not require as frequent topical therapy.
Our study is consistent with trials leading to the approval of dupilumab, demonstrating significant reduction in oral antibiotics.4 Several mechanisms have been proposed to explain this reduction. With type 2 inflammation, the airway epithelium is damaged, which can increase susceptibility to infection. Therefore, by limiting inflammation, the respiratory epithelial barrier may be restored.4
This study is the first to demonstrate a decrease in leukotriene receptor antagonist (LTRA) use in this cohort. LTRAs are recommended as an adjuvant option for persistent asthma symptoms despite low doses of ICS.5 Cysteinyl leukotrienes are inflammatory mediators produced by leukocytes that induce potent bronchoconstriction. LTRAs prevent the binding of leukotrienes to their corresponding receptors, preventing bronchoconstriction. Dupilumab also targets leukotriene production. Dupilumab blocks the IL-4Rα that prevents IL-4 induction of leukotriene C4 synthase within mast cells.
This study demonstrates that with the addition of dupilumab, providers can deescalate medications for patients with CRSwNP and asthma safely with minimal impact on CRS burden. However, it should be interpreted with caution as a minority of patients had a relatively limited burden of CRSwNP disease and it is a relatively small sample.
4 CONCLUSION
Initiation of dupilumab for CRSwNP and asthma patients had a significant reduction on medication use including oral antibiotics, ICS, LTRA, oral steroids, and topical medications for both indications.